Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2022) Volume 13, Issue 2
Post COVID Vaccination Reactive Arthritis: A Contemporary Assailant
Richmond R Gomes*Received: 01-Mar-2022, Manuscript No. JVV-22-15640; Editor assigned: 03-Mar-2022, Pre QC No. JVV-22-15640 (PQ); Reviewed: 21-Mar-2022, QC No. JVV-22-15640; Revised: 28-Mar-2022, Manuscript No. JVV-22-15640 (R); Published: 04-Apr-2022, DOI: 10.35248/2157-7560.22.13.479
Abstract
The severe acute respiratory syndrome coronavirus 2-induced coronavirus disease 2019 (COVID-19) has had a global spread. While most patients with coronavirus disease 2019 (COVID-19) present with mild or moderate symptoms, 15% may develop severe pneumonia, 5% develop acute respiratory distress syndrome (ARDS), septic shock, and multiple organ failure. Some patients may also experience arthralgia or arthritis. Cases of reactive arthritis have been reported during or after COVID-19. Vaccines play an essential role in preventing the spread. However, almost all types of vaccines have been reported to be associated with adverse events. With the approval of the use of COVID-19 vaccines, the vaccination program was started in our country and is still continuing .Reactive arthritis (ReA) after vaccination has been reported; however, ReA after COVID-19 vaccination has not been reported widely. We reported a 26-year’sold woman who suffered from an acute ReA on her left knee, left ankle and right wrist joint 8 days after COVID-19 vaccination and discussed the etiology and preventive strategy. She presented with oligo arthritis for 12 days eight days after COVID vaccination. Finally, she was diagnosed as ReA after COVID vaccination and was administered systemic steroid. The swelling and pain nearly disappeared after 7 days. On 1month follow-up, her condition was normal. ReA after COVID-19 vaccination is rare. The benefits of vaccination far outweigh its potential risks and vaccination should be administered according to the current recommendations. Further attentions should be put to determine which individual is at higher risk for developing autoimmune diseases after COVID-19 vaccination. More versatile and safer vaccines should be explored.
Keywords
COVID-19; SARS-CoV-2; Arthritis; Vaccination; Vaccine; Steroid
Introduction
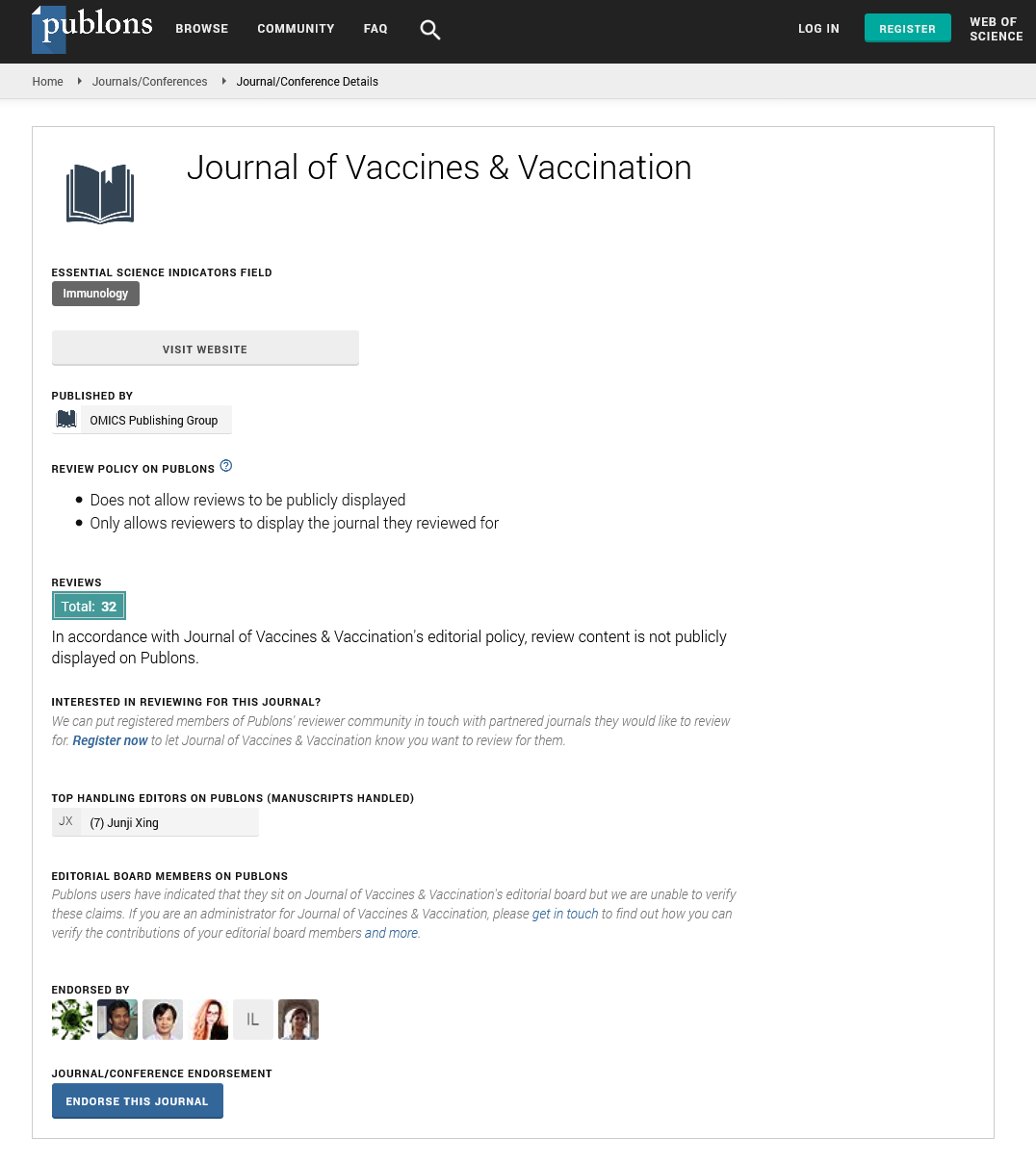
The Severe Acute Respiratory Syndrome Corona Virus 2 (SARSCoV- 2) virus-induced corona virus disease 2019 (COVID-19) has had a global spread. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first emerged in Wuhan, China, in December 2019, and the infection spread rapidly across the world. The disease caused by the virus was named coronavirus disease 2019, and was declared a global pandemic by the World Health Organization (WHO) in March 2020 [1]. While the symptoms are mild or moderate in most patients, severe pneumonia can develop in 15%, and Acute Respiratory Distress Syndrome (ARDS), septic shock, and multiple organ failure in 5% [1]. A comprehensive strategy for precautions includes hand washing, social distancing, isolation and mask-wearing. Besides, vaccines play an essential role in preventing the spread. With the advent of COVID-19 vaccinations, a vaccination program was started and is still ongoing in Bangladesh. Several different types of vaccines including inactivated vaccines, protein vaccines, vectored vaccines, and nucleic acid vaccines have been developed. So far, there is no conclusion about which vaccine is the most efficient; however, safety is a top consideration. Almost all types of vaccines have been reported to be associated with Adverse Events (AEs). Most AEs are mild and serious conditions are rare [2]. AEs range from local reactions such as injection-site pain to systemic side effects, such as fever, headache, coughing, loss of appetite, vomiting, diarrhea, joint pain, and autoimmune conditions. Autoimmune inflammatory diseases (AIIDs)following vaccinations include Reactive Arthritis (ReA), systemic lupus erythematosus, diabetes mellitus, thrombocytopenia, vasculitis, dermatomyositis, Guillain–Barré syndrome, demyelinating disorders, etc [3]. ReA was first used in 1969 to describe a sterile arthritis usually developing 1-3 weeks after a genitourinary or gastrointestinal bacterial infection; however, viruses including SARS-CoV-2have also been reported to trigger ReA [4]. The mechanisms of ReA are plausible. Homology between human and viral proteins is an established factor in viral or vaccine-induced autoimmunity. Positive HLA-B27 is known to be an important susceptible factor for the development of ReA [5]. The majority of people can vaccinate without any risk of autoimmunity onset, and autoimmune reactions after vaccination constitute probably less than 0.01% worldwide. Although rare, we should pay special attention to those susceptible individuals. Here, we reported a 26-yearoldwoman who suffered from an acute ReA on her left knee, left ankle and right wrist for 8 days after COVID-19 vaccination and discussed the etiology and preventive strategy. To our knowledge, this is the fourth report on the ReA after COVID-19 vaccination (Figure 1) [6].

Figure 1: Arthritis before and after COVID-19 vaccination.
Case Study
p>A 26-year-old female presented at our clinic with complaints of swelling and pain in the left knee, left ankle and right wrist, which had been ongoing for approximately 12 days. The pain and swelling had started 8 days after the patient had received the first dose of SARS-CoV-2 inactive vaccination (AstraZeneca) administered to the left deltoid region. The pain and swelling started at left knee thereafter left ankle and right wrist was involved concurrently. She took naproxen and indomethacin with little benefit. In the physical examination, there was swelling and redness over left knee, left ankle and right wrist. There was also painful restriction of both active and passive movements over these joints. Axial skeleton was not involved. There was no feature suggestive of enthesitis. There was neither history of arthritis or rheumatic disease nor any history of any urethral discharge or bloody diarrhoea prior the joint pain. She also denied skin rash, morning stiffness, oral or genital ulcer or red eye. Her bowel habit was normal. She had no similar family history and no history of drug allergy. Her vital signs were normal. Nasopharyngeal swabs were negative for COVID-19. The pulmonary radiograph was normal. The patient had not contracted COVID-19. In the laboratory tests, the Erythrocyte Sedimentation Rate (ESR) and C-reactive Protein (CRP) level were elevated (ESR: 94 mm/h, (reference, <20 mm/h) CRP: 50.6 mg/dl (reference, <5 mg/dl). The full blood count, uric acid and urine analysis results were normal. Rheumatoid factor, anti-nuclear, anti-cyclic citrullinated peptide antibodies, ASO titre and HLA-B27 were negative. Tests for syphilis, HIV, Hepatitis B and C were negative in serum. Immunoglobulin G was 24.36 g/L (reference, 7.5-16.5 g/L).According to the diagnostic criteria for ReA, she was diagnosed as ReA after COVID vaccination [6]. Treatment was started of 40 mg/day prednisolone. After 1 week, the complaints of the patient were reduced and the ESR and CRP values had decreased to 23 mm in 1st hour and 11 mg/dl respectively. A program of tapering prednisolone was applied. While using 5 mg/day prednisolone, the patient received the second dose of SARS-CoV-2 inactive vaccination after 2 months and no side-effects developed. The arthritis did not recur.Results and Discussion
Vaccinations are the primary tool in combating infectious diseases. However, local, systemic, and autoimmune (Autoimmune/Inflammatory Syndrome Induced by Adjuvants [ASIA syndrome]) side-effects have been reported associated with vaccinations. It is thought that vaccinations can trigger or develop autoimmunity, although the effect mechanism is not fully known [7]. It has been reported that this may be caused by the immunogenic content (inactivated virus) or adjuvants found in the vaccination. Therefore, while vaccines prevent the development of autoimmune diseases triggered by infections, autoimmunity can also be triggered after vaccination.
Risk factors for ASIA syndrome include a history of autoimmune phenomenon following vaccination, a history of autoimmunity or allergic reaction especially to vaccinations, family history of autoimmunity, or being an asymptomatic autoantibody carrier [6]. Autoimmune conditions such as arthritis, systemic lupus erythematosus, diabetes mellitus, thrombocytopenia, vasculitis, dermatomyositis, and Guillain- Barré syndrome have been reported to be seen following vaccinations [8].
ReA after vaccination, being one of AIIDs, has been reported and the etiologies are multiple with a combination of familial, genetic, hormonal, environmental, or other risk factors for overstimulation of the immune system. For this patient, some elements are typical for ReA including youth, a delay of 1 week between the vaccination and the beginning of the Rheumatological picture, oligoarticular inflammatory disease predominantly in the lower limbs, and the good effect treating with systemic corticosteroid. Some are however atypical: the female gender and the negative HLA-B27 [9].
Vaccines with inactivated viral products or attenuated living microorganisms may operate as autoimmune disease-triggering agents. Adjuvants within vaccines may also cause specific autoimmune AEs which are named as “Autoimmune/ inflammatory Syndrome Induced by Adjuvant (ASIA)” [10].Four groups of individuals who might be susceptible to develop vaccination induced ASIA were defined: patients with prior post vaccination autoimmune phenomena, patients with a medical history of autoimmunity, patients with a history of allergic reactions, and individuals who are prone to develop autoimmunity [6]. For these individuals, if vaccination is of utmost importance, it might be given, but the patients should be followed closely and treated if necessary. Two main mechanisms have been offered to explain the development of autoimmunity: one is antigen-specific, such as the molecular mimicry, the other is nonspecific known as “bystander activation”. Molecular mimicry refers to a significant similarity between certain pathogenic elements contained in the vaccine and specific human proteins [11]. This similarity may lead to immune crossreactivity, wherein the reaction may harm the similar human proteins, essentially causing autoimmune disease. The latter is characterized by auto reactive B and T cells that undergo activation in an antigen-independent manner. For this patient, her elevated immunoglobulin G antibody level was correlated with the immune response for generating the neutralizing antibodies after vaccination.
Arthritis was reported in 2 cases following the diptheria, poliomyelitis, and tetanus toxoid combined vaccination. The first case was a 17-year-old female who developed arthritis in the right knee 12 days after vaccination, and was applied with synovectomy as no response was obtained to intra-articular steroids. The second cases were a 22-year-old female who developed arthritis in the right ankle one day after vaccination, and recovered in 3 days with NSAID treatment [12]. In another case report, a patient who developed reactive arthritis after tetanus vaccination is presented by Sahinet [13].
In a study by Geier et al., a significant correlation was determined between adult hepatitis B and rubella vaccinations and chronic arthritis [14]. Following rubella vaccination, arthritis was determined 3-fold more in females than males. The mean age was approximately 45 years and arthritis developed within a period of mean 10-11 days after the vaccination. Following hepatitis B vaccination, arthritis was seen 3.5-fold more in females than in males. The mean age was 33 years and arthritis was determined approximately 16 days after the vaccination. Asakawa et al. presented the case of a 79-year-old male who developed migratory polyarthritis starting from the 4th metacarpophalangeal joint 2 days after an influenza vaccination [15].
There are also case reports in literature of reactive arthritis developing during or after COVID-19 infection [16,17]. Ono et al. reported the development of bilateral ankle arthritis in a 50- year-old male patient on the 21st day after extubating following 11 days of intubation because of COVID-19 pneumonia [16]. The complaints recovered with NSAID and intra-articular steroids. Lopez et al. reported 4 cases of males aged 45-71 years who developed arthritis during COVID-19 infection [17]. Arthritis was seen in the knee, ankle, and 1st metatarsophalangeal joints. The time interval from the onset of COVID-19 symptoms to the onset of arthritis was approximately 8-27 days. A history of gout was present in 3 of the 4 patients. Left elbow arthritis was reported 1 week after vector-based SARS-CoV-2 vaccination [18]. In another case report, a patient who developed reactive arthritis 1 week after inactive SARSCoV- 2 vaccination is presented An QJ [19]. Watad et al. presented 27 patients with post-vaccine attack or newly developed immune-mediated disease [20]. Unlike my cases, the majority of vaccines are mRNA vaccines and only 2 are vectorbased vaccines. 21 patients had autoimmune or rheumatic disease prior to vaccination. 17 patients developed flare and 10 patients developed new-onset immune-mediated disorders. Polymyalgia rheumatica, myasthenia gravis, arthritis and skin manifestations have been reported. We cannot talk about a definite causal relationship between arthritis and vaccine. However, these post-vaccination disorders should be closely monitored.
Continuing assessment of post-license vaccine safety is important for the detection of rare and longer-term side effects [10].This is particularly important in a pandemic situation, such as the COVID-19 pandemic, as rapid clinical development of several vaccines is likely to take place and large numbers of people are likely to be vaccinated within a short time [11].
AstraZeneca, which is one of the COVID-19 vaccinations, is an inactive vaccination and contains alum as an adjuvant [21]. The patient presented in this paper was administered the vaccination in a hospital settings. Arthritis developed 8 days after the first dose in the patient.
Although there is a lack of reporting of all the vaccinations worldwide, autoimmune reactions develop in approximately 0.01% and most of these are mild and self-limiting findings [6]. Vaccination is of critical importance for infectious diseases and in the current global situation of the COVID-19 pandemic. Further studies with the reporting of arthritis related to COVID-19 and vaccinations will be able to provide more clarification.
Current vaccine development is largely “empirical vaccinology”, the “one-size-fits-all” approach, which ignores the complexity and diversity of the human immune system and host genome. In the future, however, personalized vaccinology is the goal of new vaccine development which means to provide the right vaccine for the right patient at the right time and with the right dose. Finally, more versatile and safer vaccines should be explored [22]. Different vaccine platforms have their own advantages and challenges. Recent studies demonstrate that mRNA vaccines surpass others in patients with AIIDs. The mRNA vaccines can be used to turn down an unwanted immune response and have shown promise in autoimmunity. Additionally, mRNA is a noninfectious, non-integrating vector. The possibility of contamination or insertional mutagenesis is not even theoretically present. Even so, real data on COVID-19 vaccines in patients with AIIDs tend to zero. It is imperative to develop better, safer vaccines [23,24].
Conclusion
In summary, ReA after COVID-19 vaccination is rare. Although vaccine administration has been associated with autoimmune manifestations in certain genetically predisposed individuals, the benefits of vaccination far outweigh its potential risks and vaccination should be administered according to the current recommendations. Further attention should be put to determine which individual is at higher risk for developing autoimmune diseases after COVID-19 vaccination. More versatile and safer vaccines should be explored.
REFERENCES
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
[Crossref] [Google Scholar] [Pub Med]
- Pellegrino P, Perrone V, Pozzi M, Carnovale C, Perrotta C, Clementi E, et al. The epidemiological profile of ASIA syndrome after HPV vaccination: an evaluation based on the Vaccine Adverse Event Reporting Systems. Immunol Res.2015;61(1):90-96.
[Crossref] [Google Scholar] [Pub Med]
- Velikova T, Georgiev T. SARS-CoV-2 vaccines and autoimmune diseases amidst the COVID-19 crisis. Rheumatol Int. 2021;41(3):509-518.
[Crossref] [Google Scholar] [Pub Med]
- Wendling D, Verhoeven F, Chouk M, Prati C. Can SARS-CoV-2 trigger reactive arthritis?. Spine J. 2021;88(1):105086.
[Crossref] [Google Scholar] [Pub Med]
- Lyons-Weiler J. Pathogenic priming likely contributes to serious and critical illness and mortality in COVID-19 via autoimmunity. J Transl Autoimmun. 2020;3:100051.
[Crossref] [Google Scholar] [Pub Med]
- Soriano A, Nesher G, Shoenfeld Y. Predicting post-vaccination autoimmunity: who might be at risk?. Pharmacol. Res. 2015;92:18-22.
[Crossref] [Google Scholar] [Pub Med]
- Shoenfeld Y, Aron-Maor A. Vaccination and autoimmunity—‘vaccinosis’: a dangerous liaison?. J Autoimmun. 2000;14(1):1-10.
[Crossref] [Google Scholar] [Pub Med]
- Perricone C, Colafrancesco S, Mazor RD, Soriano A, Agmon-Levin N, Shoenfeld Y. Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) 2013: Unveiling the pathogenic, clinical and diagnostic aspects. J Autoimmun.2013;47: 1-6.
[Crossref] [Google Scholar] [Pub Med]
- Gershwin LJ. Adverse reactions to vaccination: from anaphylaxis to autoimmunity. Veterinary Clinics: Small Animal Practice. 2018; 48(2):279-290.
[Crossref] [Google Scholar] [Pub Med]
- Moro PL, Haber P, McNeil MM. Challenges in evaluating post-licensure vaccine safety: observations from the Centers for Disease Control and Prevention. Expert Rev Vaccines. 2019;18(10):1091-1101.
[Crossref] [Google Scholar] [Pub Med]
- Pollard AJ, Bijker EM. A guide to vaccinology: from basic principles to new developments. Nat Rev Immunol.2021;21(2):83-100.
[Crossref] [Google Scholar] [Pub Med]
- Maillefert JF, Tonolli-Serabian I, Cherasse A, Demoux AL, Tavernier C, Piroth L. Arthritis following combined vaccine against diphtheria, polyomyelitis, and tetanus toxoid. Clin Exp Rheumatol. 2000;18(2):255-256.
- Sahin N, Salli A, Enginar AU, Ugurlu H. Reactive arthritis following tetanus vaccination: a case report. Mod Rheumatol. 2009;19(2):209-211.
[Crossref] [Google Scholar] [Pub Med]
- Geier DA, Geier MR. A one year followup of chronic arthritis following rubella and hepatitis B vaccination based upon analysis of the Vaccine Adverse Events Reporting System (VAERS) database. Clin Exp Rheumatol. 2002;20(6):767-772.
- Asakawa J, Kobayashi S, Kaneda K, Ogasawara H, Sugawara M, Yasuda M, et al. Reactive arthritis after influenza vaccination: report of a case. Mod Rheumatol. 2005;15(4):283-285.
[Crossref] [Google Scholar] [Pub Med]
- Ono K, Kishimoto M, Shimasaki T, Uchida H, Kurai D, Deshpande GA, et al. Reactive arthritis after COVID-19 infection. RMD Open.2020; 6(2):e001350.
[Crossref] [Google Scholar] [Pub Med]
- Peral-Garrido ML, Calabuig I, Tovar-Sugrañes E, Jovani V, Bernabeu P, García-Sevila R, et al. Case series of acute arthritis during COVID-19 admission. Ann Rheum Dis.2021;80(4):e58.
[Crossref] [Google Scholar] [Pub Med]
- Baimukhamedov C. Arthritis of the left elbow joint after vaccination against SARS-CoV-2 infection. Int J Rheum Dis. 2021;24(9):1218.
[Crossref] [Google Scholar] [Pub Med]
- An QJ, Qin DA, Pei JX. Reactive arthritis after COVID-19 vaccination. Hum. Vaccin. Immunother. 2021;17(9):2954–2956.
[Crossref] [Google Scholar] [Pub Med]
- Watad A, De Marco G, Mahajna H, Druyan A, Eltity M, Hijazi N, et al. Immune-mediated disease flares or new-onset disease in 27 subjects following mRNA/DNA SARS-CoV-2 vaccination. Vaccines. 2021;9(5):435.
[Crossref] [Google Scholar] [Pub Med]
- Kashte S, Gulbake A, El-Amin III SF, Gupta A. COVID-19 vaccines: rapid development, implications, challenges and future prospects. Hum. Cell. 2021;34(3):711-733.
[Crossref] [Google Scholar] [Pub Med]
- Poland GA, Ovsyannikova IG, Kennedy RB. Personalized vaccinology: a review. Vaccine. 2018;36(36):5350-5357.
- Villanueva MT. Suppressing autoimmunity with mRNA vaccines. Nat Rev Drug Discov. 2021; 20(2):99-100.
[Crossref] [Google Scholar] [Pub Med]
- Flemming A. mRNA vaccine shows promise in autoimmunity. Nat Rev Immunol. 2021;21(2):72.
[Crossref] [Google Scholar] [Pub Med]
Citation: Gomes RR (2022) Post COVID Vaccination Reactive Arthritis: A Contemporary Assailant. J Vaccines Vaccin. 13:479.
Copyright: © 2022 Gomes RR. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.