PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
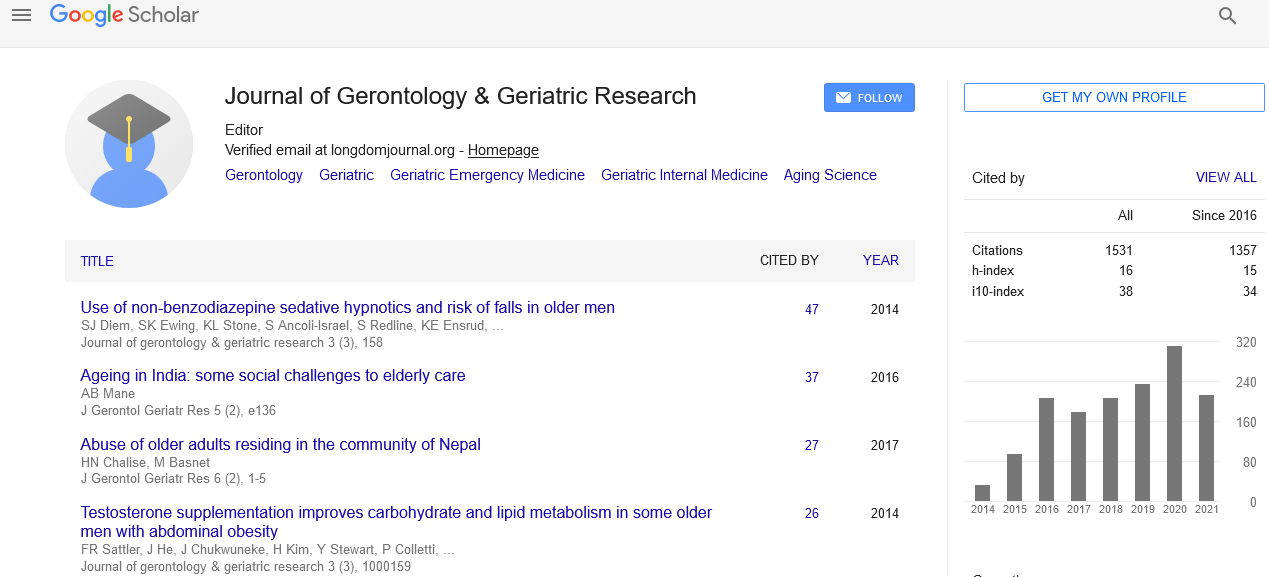
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2023) Volume 12, Issue 5
Polypharmacy in Geriatric Patients: Balancing Risks and Benefits
Agatha Khristie*Received: 02-Oct-2023, Manuscript No. jggr-23-23504; Editor assigned: 04-Oct-2023, Pre QC No. P-23504; Reviewed: 17-Oct-2023, QC No. Q-23504; Revised: 23-Oct-2023, Manuscript No. R-23504; Published: 30-Oct-2023, DOI: 10.35248/2167-7182.2023.12.700
Introduction
Polypharmacy is a prevalent and concerning issue in geriatric medicine, where elderly patients often take multiple medications to manage various chronic conditions. While medications can provide significant therapeutic benefits, the concurrent use of multiple drugs can lead to various complications and risks. Balancing the potential benefits and risks of polypharmacy in geriatric patients is a complex and critical aspect of modern healthcare. This article delves into the concept of polypharmacy in geriatric patients, explores the associated risks, and discusses strategies for achieving a balance that optimizes the quality of care for this vulnerable population.
Description
Polypharmacy, generally defined as the concurrent use of multiple medications, is particularly prevalent in the geriatric population. This phenomenon can be attributed to several factors, including an increased prevalence of chronic medical conditions among older adults, advances in medical treatment options, and the natural aging process, which often necessitates more medications to manage age-related health issues. The term "polypharmacy" often carries a negative connotation due to the potential for adverse outcomes. However, it is essential to distinguish between appropriate and inappropriate polypharmacy. Appropriate polypharmacy occurs when multiple medications are prescribed and used effectively to address various medical conditions, improve overall quality of life, and extend life expectancy. Inappropriate polypharmacy, on the other hand, refers to the excessive, unnecessary, or inappropriate use of medications, leading to adverse effects, drug interactions, and decreased patient well-being [1].
Elderly individuals often have multiple chronic medical conditions, such as hypertension, diabetes, heart disease, arthritis, and more. Managing these conditions may require the use of several medications concurrently. Geriatric patients frequently receive care from multiple specialists, each prescribing medications to address specific health issues. Coordinating care and medications among various specialists can be challenging. As individuals age, physiological changes occur, affecting drug metabolism and distribution. This often necessitates adjustments in medication dosages. Prophylactic medications, such as aspirin for cardiovascular health or statins for cholesterol management, may be prescribed to reduce the risk of future health issues. Many elderly patients take medications for symptomatic relief, such as painkillers, sleep aids, or antacids [2].
As the number of medications increases, so does the risk of adverse drug reactions, which can be severe and life-threatening in older adults. Combining multiple medications can lead to drug interactions, altering the effectiveness or safety of individual drugs. The complexity of managing multiple medications can lead to non-adherence, where patients may forget to take their medications or intentionally skip doses due to concerns about side effects or costs. Certain medications, particularly those with anticholinergic properties, may contribute to cognitive impairment in older adults. Some medications can increase the risk of falls and fractures in the elderly, leading to hospitalizations and a decline in functional status. Polypharmacy-related complications often result in hospitalizations, adding to healthcare costs and disrupting patients' lives. Comprehensive Medication Review: Regularly reviewing a patient's medication regimen is essential to identify any potentially inappropriate medications, drug interactions, or duplications. This can be done by pharmacists or healthcare providers during medication reconciliation. Engaging geriatric patients and their caregivers in shared decision-making regarding their medication regimen can help ensure that treatment aligns with individual preferences and goals. Clinicians should critically assess each medication's benefit, necessity, and potential harm, and consider DE prescribing when appropriate. DE prescribing involves discontinuing medications that may no longer be needed or pose unnecessary risks [3-5].
Conclusion
Polypharmacy in geriatric patients is a complex issue that requires careful consideration and management. While multiple medications may be necessary to address the myriad of chronic conditions that older adults face, the risks associated with polypharmacy are significant and should not be underestimated. Balancing the benefits and risks of polypharmacy requires a multidisciplinary approach, including regular medication reviews, shared decision-making, rationalizing
Acknowledgement
None.
Conflict of Interest
None.
References
- Coelho EM, Da Mota MP, Fonseca SC, Matos AP, Carvalhal MI. Exercise with music: An innovative approach to increase cognition and reduce depression in institutionalized elderly. Rev Psicol Deporte. 2020; 29:49-56.
- Jung YH, Lee S, Kim WJ, Lee JH, Kim MJ, Han HJ. Effect of integrated cognitive intervention therapy in patients with mild to moderate Alzheimer's disease. Dement Neurocogn Disord 2020;19:86.
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695-699.
- Smith T, Gildeh N, Holmes C. The montreal cognitive assessment: Validity and utility in a memory clinic setting. Can J Psychiatry. 2007;52:329-332.
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: A preliminary report. "J Psychiatr Res.1982; 17:37-49.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Khristie A (2023). Polypharmacy in Geriatric Patients: Balancing Risks and Benefits. J Gerontol Geriatr Res.12:700.
Copyright: © 2023 Khristie A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.