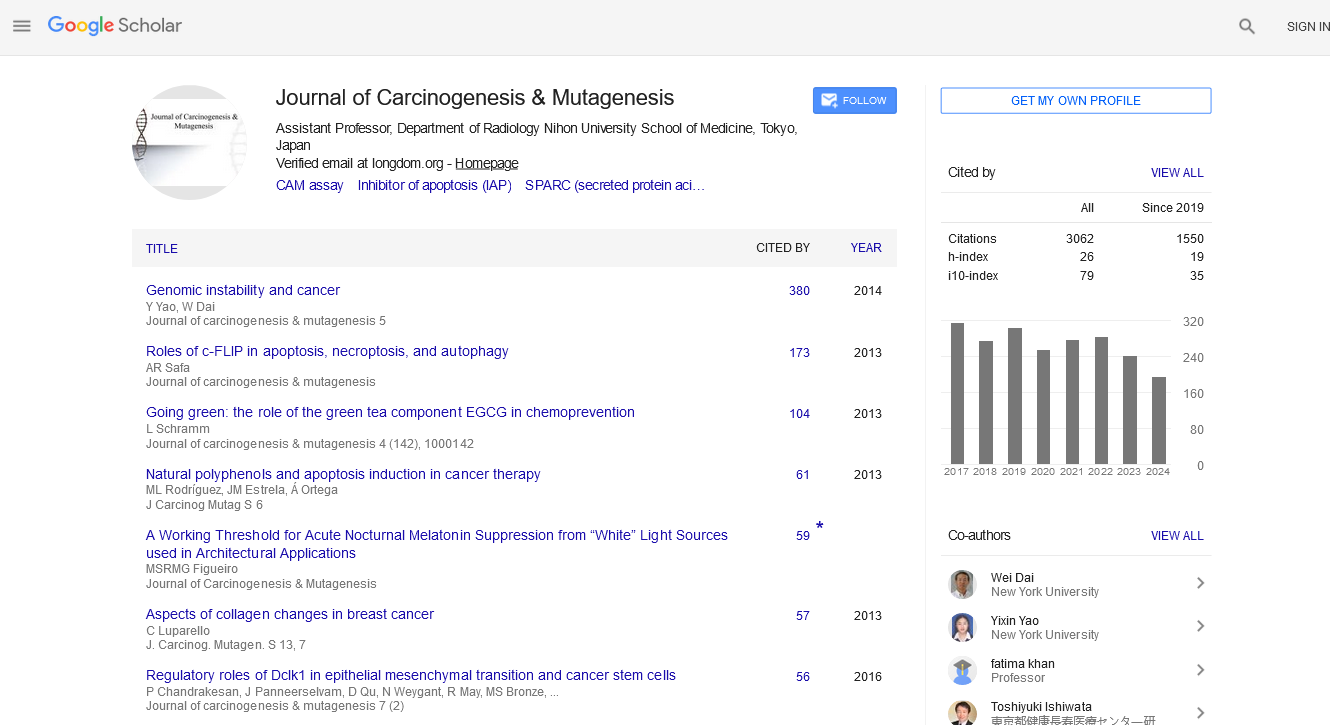
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2021) Volume 12, Issue 6
Polygenic Risk Score in NAFLD/NASH-Associated Hepatocellular Carcinoma Along With Multifactorial Process
Kazumi Fujioka*Received: 15-Dec-2021 Published: 07-Dec-2021
Abstract
The prevalence and incidence of Non-Alcoholic Fatty Liver Disease (NAFLD) is increasing due to the epidemics of obesity and Type 2 Diabetes Mellitus (T2DM). Recently, a link between NAFLD and hypertension along with new genetic expression has been identified. NAFLD is a multisystem disease and is associated with hepatic and extrahepatic diseases. The author previously described that in addition to the epidemiological and single genetic factors, the study of combined effect of the variants may be attributed to the risk stratification in NAFLD/NASHrelated hepatocellular carcinoma (HCC) and also suggested that the stratification of the risk of NAFLD related HCC especially non-cirrhotic HCC based on the characteristic clinical and genetic evidence may contribute to the prevention, prediction, and surveillance. The risk factors and multifactorial process include obesity, T2DM, hypertension, ethnicity, genetic Polymorphism PNPLA3, TM6SF2, GCKR, MBOA17, and HSD17B13, epigenetic factors, transcriptional factors, post-transcriptional modification, and hepatic lipogenesis carcinogenesis in NAFLD. In this article, the author reviewed the current knowledge of risk factors, multifactorial process, and polygenic risk score (PRS) in NAFLD-related HCC. Although several risk factors and complex and multifactorial process are present in the progression of NAFLD-related HCC, the author suggests that comprehensive determination using epidemiological factor and PRS including PNPLA3, TM6SF2, GCKR, MBOAT7, and HSD17B13 may be attributed to the risk stratification, prognosis, and therapeutic strategy in cirrhosis and non-cirrhosis patients with NAFLDrelated HCC.
Keywords
Polygenic risk score; Non-cirrhosis NAFLD-HCC; Multifactorial process; Hepatic lipogenesis carcinogenesis; Atherosclerosis
Introduction
The prevalence and incidence of NAFLD is increasing due to the epidemics of obesity and T2DM [1]. It is known that NAFLD is a multisystem disease and is associated hepatic and extrahepatic manifestations [2,3].The author previously described that on the basis of the characteristic clinical and genetic evidence, the risk stratification of the medium/high risk in NAFLD-related HCC, especially non-cirrhotic HCC may contribute to the prevention, prediction, and surveillance [4]. In this article, the current knowledge of the risk factors, complex and multifactorial process, and PRS in the development and progression of NAFLD-related HCC will be reviewed in detail. Non-Alcoholic fatty liver disease (NAFLD) is the common liver disease worldwide due to the increasing rates in parallel to obesity and T2DM [1]. Whereas the close association between NAFLD and hypertension associated with a new genetic has been identified [5]. Many studies provided that NAFLD associates with endothelial dysfunction assessed by Flow- Mediated vasodilation (FMD) study, increased Intima-Media Thickness (IMT) by evaluated common carotid artery, and increased Pulse Wave Velocity (PWV) that are established as CVD and atherosclerosis indicators [2]. Recent clinical report also suggested that endothelial dysfunction is independent of MS in patients with NAFLD [3,6].
Association between NAFLD/NASH and Atherosclerosis
The clinical practice guidelines stated that CVD should be identified in NAFLD irrelevant of the presence of traditional risk factors. The author previously described that an association between chronic liver disease (NAFLD/NASH and chronic C virus hepatitis: HCV infection) and systemic atherosclerosis may be present due to the presence of the inflammation as a common pathway [7]. Flow-mediated vasodilation (FMD) and nitroglycerin-mediated vasodilation (NMD) examinations in the brachial artery is a promising procedure for estimating vascular endothelial and vascular smooth muscle cell (VSMC) function in atherosclerosis [8]. The author has described several studies on the diseases of migraine, CVD, chronic kidney disease (CKD), dyslipidemia, aging liver, and COVID-19 using FMD and NMD tests [9-20].
Clinical Presentations in NAFLD/NASH-Related HCC
The growing incidence has showed that NASH/NAFLD has led to an increase of NASH-related HCC [21]. Regarding cirrhotic NAFLD-related HCC, the study by Grimaudo et al. and a metaanalysis have been identified [22,23]. With respect to noncirrhotic NAFLD-related HCC, the clinical practice guidelines stated that studies have associated obesity and T2DM with the risk of HCC and also indicated that patients with NAFLDderived HCC at diagnosis are older than those with non- NAFLD HCC, with a lower prevalence of cirrhosis. A multicenter prospective study by HCC-NAFLD Italian Study Group indicated that NAFLD-HCC is more often found at a later tumor stages. A United States multicenter study and a meta-analysis [3,24-26]. Described that HCCs developed in patient without cirrhosis and that NAFLD was the most common liver disease in these patients. Mohamad et al. mentioned that patients with non-cirrhotic NAFLD-related HCC are more likely to represent at an older age, larger tumor size, and higher rates of tumor recurrence. Bengtsson et al. reported that patients with non-cirrhotic NAFLD-related HCC were observed in 37% of NAFLD-HCC, suggesting that patients with non-cirrhotic NAFLD-HCC, compared with patients with cirrhotic NAFLD-HCC, were older, a lower prevalence of T2DM, larger tumors, and allocated treatments. The report by Anstee et al. described that up to 49% of NAFLD-derived HCC develop in patients without cirrhosis [27-29].
Non Invasive Elastography and Magnetic Resonance Imaging as Alternatives to Liver Biopsy
According to American Gastroenterological Association (AGA) clinical practice update, although NAFLD-related HCC may arise in non-cirrhotic status, is often diagnosed at advanced stages, guidelines provided limited guidance/recommendations addressing HCC surveillance in patients with non-cirrhosis [30]. Based on the evidence of reviews, they provided Best Practice Advice statements of clinical management in patients with NAFLD [30]. The new non-invasive, cost-effective diagnostic procedures are needed because of the progression to the liver fibrosis, cirrhosis and HCC in NAFLD. Non-invasive tests including vibration controlled transient elastography (VCTE), point shear wave elastography (pSWE), 2-dementional shear wave elastography (2DSWE), magnetic resonance elastography (MRE), and magnetic resonance imaging (MRI) have been proposed in patients with NAFLD [31]. It is suggested that the VCTE and 2D-SWE are potential tools in staging liver fibrosis in patients with NAFLD. It is thought that 2D-SWE also represents a significant procedure to differentiate malignant from benign focal liver lesions (FLLs) [32].To evaluate the severity of liver fibrosis and NASH (fatty inflammation), liver elastography and MRI tests have been noninvasively suggested as alternatives to liver biopsy in NAFLD patients [31]. From a systematic review and meta-analysis, they emphasized that elastography may assist in fibrosis evaluation and mentioned that some techniques of measuring liver stiffness had good performance for the diagnosis of severe liver fibrosis in patients with NAFLD. With the advance of new technology, elastography test as alternatives to liver biopsy may noninvasively assist in the severity of the fibrosis evaluation in patient with NAFLD.
Risk Factors and Multifactorial Process in NAFLD-Associated HCC
It is known that the progression of NASH-derived HCC is a complex and multifactorial process [33]. The study indicated that many risk factors including obesity, type 2 diabetes mellitus (T2DM), Hispanic ethnicity, and genetic polymorphism in PNPLA3, TM6SF2, GCKR, MBOA17, and HSD17B13 in NAFLD are independently associated with HCC [34]. It is thought that plausible mechanisms of diabetes-related carcinogenesis included inflammatory activation, insulin resistance (IR), hyperinsulinemia, and aberrations in insulin-like growth factor-1 (IGF-1) signaling [35,36]. Simon et al. described that T2DM is independently associated with the increased risk for HCC and suggested the importance of insulin resistance in the pathogenesis of HCC. Epidemiologic evidence has showed that T2DM is associated with an increased risk for many cancers, including colon, pancreas, liver, kidney, and breast [35]. Hagstrom et al. mentioned that the risk of extrahepatic malignancies has been increased indicating the most evidence for a link between NAFLD and colorectal cancer. Recently, Yang et al. suggested that T2DM is significantly associated with increased HCC risk in patient with NASH-related cirrhosis by multivariable analysis [37,38]. Regarding obesity status, it is known that BMI is associated with carcinogenesis risk [39]. Grohmann et al. have reported that obesity-related hepatic oxidative stress can independently contribute to development of NASH and HCC through pathways. Based on the current evidence, it is suggested that several risk factors including genetic and non-genetic and multifactorial process in the development and progression for NAFLD-related HCC have been identified [40-42].
Link between Hypertension and NAFLD along with Genetic Relation
The study indicated that 49.5% of patients with hypertension have NAFLD, and the prevalence of hypertension is significantly increased in individuals with NAFLD than in the general population [5,41,42]. Clinical and experimental studies suggested that NAFLD may promote the occurrence of hypertension, T2DM, and Cardiovascular Disease (CVD) [43]. Cai et al. mentioned that the relationship between NAFLD and hypertension is independent of other metabolic components [44]. It is putative that NAFLD may induce systemic inflammation, insulin resistance, oxidative stress, and increased vasoconstriction and decreased vasodilation, in turn leading to hypertension [5]. With respect to the link between NAFLD and vascular reactivity, clinical studies revealed that patients with NAFLD represent the increased level of circulating Asymmetrical Dimethylarginine (ADMA) which is an endogenous inhibitor of Nitric Oxide synthase (NOS), independent of classical cardiovascular (CV) risk factors [45]. The study also indicated that NAFLD is an independent factor in the development of arterial stiffness which reflects arteriosclerosis status [46]. Recent clinical report suggested that endothelial dysfunction is independent of metabolic syndrome (MS) in patients with NAFLD [6]. Although it is known that the close association between NAFLD and hypertension, however, there is limited evidence on the genetic relation between NAFLD and hypertension. PNPLA3 and TM6SF2 have been studied much more in CVD than in hypertension. The reports suggested that the ADIPOQ C11377G (rs266729) has been associated with a significantly increased risk of NAFLD and hypertension [47,48]. While, it has been suggested that the AGTR1 (angiotensin receptor type 1) gene might be involved in multiple pathways associated with the development in NAFLD using bioinformatics analysis [49]. It is putative that the new gene expression such as ADIPOQ C11377G and AGTR1 may robustly contribute to a link between NAFLD and hypertension. With respect to the recommendations, the clinical practice guidelines have stated that NASH patients with fibrosis associated with hypertension should receive a closer monitoring because this entity causes the disease progression with a higher risk.
The Key Factors in NAFLD-Associated HCC
It has been reported that genetic and epigenetic factors impact the initiation and progression of NAFLD-associated HCC. Additionally, transcriptional factors and post-transcriptional modification are significant for the development of HCC under inflammatory and fibrotic status [50]. Regarding epigenetic factors, it is thought that DNA methylation, long non-coding RNAs (lncRNAs), and miRNAs have profound impacts on NAFLD-associated HCC progression. With respect to the transcriptional factors, E2Fs transcriptional factors, hypoxiainducible factors (HIFs), Forkhead box (FOXO), and PPARs, modulate NAFLD progression through signaling pathways. With regard to the post-transcriptional modification, it is thought that RNA-binding proteins (RBPs) and RNA splicing factor (SF) is attributed to liver damage, NAFLD occurrences, and HCC progression [51].
Hepatic Lipogenesis Carcinogenesis
Liang et al. also mentioned evidence that HCC can occur in patients with non-cirrhotic NASH [52]. The study by Liang et al. provided that dietary cholesterol promotes NASH related HCC through dysregulated metabolism and calcium signaling. NASH development caused by dietary cholesterol is associated with aberrant gene expression which linked with inflammation, dysregulated metabolic and cancer pathways. It is suggested that integrated genetic and expressional alterations in NASH-related HCC affected distinct genes pertinent to five pathways including calcium signaling, insulin, cell adhesion, axon guidance, and metabolism. It has been reported that the novel aberrant gene expression, mutation and core oncogene pathways recognized in cholesterol-associated NASH-related HCCs in mice were observed in human NASH-related HCC [52]. The recurrently mutated genes included RYR1, MTOR, SDK1, CACNA1H and RYR2. Regarding metabolic-related genes, ALDH18A1, CAD, CHKA, POLD4, PSPH, and SQLE were included in human NASH-related HCCs. While, Ribas et al. provide the evidence for tumor promoter role of cholesterol in NASH-related HCC associated with an increased expression of the genes involved in immune checkpoints suggesting that cholesterol tends to favor a milieu of T-cell exhaustion. Zeng et al. [53,54] revealed that B cells, DCs, and MAIT cells are key dysregulated immune cells in NAFLD and progression of NAFLD-related HCC [53,54]. With regard to the immunologic pathways which subsequently activate oncogenic mechanisms, it has been demonstrated that ROS accompanied by the production of lipid peroxidation increases the release of inflammation and inhibitory cytokines including TNF-α, IL6, leptin, and adiponectin [33]. Kutlu et al. described molecular signaling pathways regarding their mechanism of action in NASH-related HCC. Based on the clinical and experimental studies, it is plausible that steatosis-related lipotoxicity may cause hepatocarcinogenesis [33].
Polygenic Risk Score for NAFLD-Related HCC
Current studies indicated that genetic susceptibility increases risks of NAFLD, NASH, and NASH-related cirrhosis [55]. It has been previously reported that five genes including PNPLA3, TM6SF2, GCKR, MBOAT7, and HSD17B13 known to be associated with NASH are involved in glucose and fat homeostasis regulatory pathways [55,56]. The most closely related genetic variant with NAFLD is PNPLA3-I148M [57]. TM6SF2 in hepatic lipid export, and GCKR and MBOAT7 increase triglyceride synthesis through canonical and noncanonical pathways of de novo lipogenesis [58]. Recently, Jamialahmadi et al. have showed 2 novel genetic variants in GPAM and APOE that are associated with liver fat content and liver disease indicating a strong association between liver damage and lipid biology [58]. The report by Gellert-Kristensen et al. suggested that a genetic risk score (GRS), combining the three genetic variants in PNPLA3 p.I148M, TM6SF2 p.E167K, and HSD17B13 rs72613567, was associated with cirrhosis and HCC in fatty liver including NAFLD and alcoholic type in individual from the general population, indicating that a GRS showed risk of cirrhosis by up to 12-fold and risk of HCC by up to 29-fold. Meanwhile, the report indicated that the risk of occurrence of NAFLD and associated complications is determined by the environmental and genetic factors [59,60]. In the NAFLD cohort, the recent study showed that PRS value predicted HCC more intensely than single variants [61]. They indicated that the relationship between PRS and HCC was detected in the subjects with and without the severe fibrosis. Whereas in the UKBB cohort, they showed that PRS predicted HCC irrespective of classic risk factors and liver cirrhosis condition. They described a causal association between liver fat and HCC suggesting that PRS improve the accurate diagnosis of HCC in individuals with and without severe fibrosis status. They suggested that the risk scores assisted to show the risk of HCC both in high-risk individuals and in the general population. As Long et al. described the polygenic risk score as a promising predictor for HCC in the population with NAFLD, they also suggest that the quantitative genetic features of ethnicity should be included as covariates in the association tests [62]. Jamialahmadi et al. also suggested that the PRS prediction for HCC in a large European NAFLD cohort was largely superior to that of the single genetic risk variants [62]. They stated that, as part of the ability of a PRS to predict HCC is mediated by the life-long burden of genetic variants on liver damage, suggesting that the PRS may be optimal to detect young at-risk individuals. Although several risk factors and complex and multifactorial process are present in NAFLD-related HCC, it is plausible that the comprehensive evaluation of the epidemiologic factor and PRS may be attributed to the risk stratification, prognosis, and therapeutic strategy in cirrhosis and non-cirrhosis patients with NAFLDrelated HCC.
Summary
With the advance of new technology, elastography test as alternatives to liver biopsy may noninvasively assist in the severity of the fibrosis evaluation in patient with NAFLD. It is putative that the genetic relation using new gene ADIPOQ C11377G and AGTR1 may robustly contribute to a link between NAFLD and hypertension. Based on the clinical and experimental studies, it is plausible that steatosis-related lipotoxicity may cause hepatocarcinogenesis. The author suggests that the comprehensive estimation of the epidemiological factor and PRS may contribute to the risk stratification, prognosis, and therapeutic strategy in cirrhosis and non-cirrhosis patients with NAFLD-related HCC.
Conclusion
The author suggests that based on the current evidence, the comprehensive determination using epidemiological factor and polygenetic risk score may be attributed to the risk stratification, prognosis, and therapeutic strategy in cirrhosis and non-cirrhosis patients with NAFLD-related HCC. Although several risk factors and complex and multifactorial process are present in the development and progression of NAFLD-related HCC.
REFERENCES
- Younossi ZM. Non-alcoholic fatty liver disease- a global public health perspective. Hepatology. 2019;70(3) :531-544.
- Francque SM, van der Graaff D, Kwanten WJ. Non-alcoholic fatty liver disease and cardiovascular risk: pathophysiological mechanisms and implications. J Hepatol. 2016; 65 (2): 425-443.
- Marchesini GEASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. Diabetelogia 2016; 59: 1121-1140.
- Fujioka K. Current genetic advances in NAFLD/NASH: related hepatocellular carcinoma along with characteristic clinical manifestations. J Carcinog Mutagene 2021; 12 (S17): 1000001.
- Zhao YC, Zhao GJ, Chen A, She ZG, Cai J, Li H. Nonalcoholic fatty liver disease: an emerging driver of hypertension. Hypertension 2020; 75: 275-284.
- Narayan J, Das HS, Nath P, Singh A, Mishra D, Padhi PK, et al. Endothelial dysfunction, a marker of atherosclerosis, is independent of metabolic syndrome in NAFLD patients. Int J Hepatol 2020; 17(7): 1825142.
- Fujioka K. Association between chronic liver disease and atherosclerosis: an inflammation as common pathway. J Clinical Trials. 2021;11(1): 444.
- Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002; 39: 257-265.
- Fujioka K, Oishi M, Fujioka A, Nakayama T. Increased nitroglycerin-mediated vasodilation in migraineurs without aura in the interictal period. J Med Ultrason 2018; 45:605-610.
- Fujioka K. Reply to: Endothelium-dependent and –independent functions in migraineurs. J Med Ultrason 2019; 46: 169-170.
- Fujioka K, Oishi M, Nakayama T, Fujioka A. Association of brachial artery measures with estimated GFR>60mL/min/1.73m2. in a cross-sectional study of the community-based women Angiol Open Access. 2019; 7(3): 231.
- Fujioka K. Propensity to the vascular smooth muscle cell abnormality in migraine without aura and vasospastic angina along with a genome-wide association studies. J Carcinog Mutagene. 2019; 10.334.
- Fujioka K, Oishi M, Fujioka A, Nakayama T, Okada M. Interrelationship among lipid profiles, arterial stiffness, and nitroglycerin-mediated vasodilation in the community-based setting of Japanese women. Angiol Open Access . 2019; 7: 235.
- Fujioka K. Effect on microRNA-92a in atherosclerosis along with flow-mediated vasodilation study. J Cancer Oncol. 2020; 4(1): 000153.
- Fujioka K. A novel biomarker microRNA-92a-3p as a link between cardiovascular disease and chronic kidney disease. J Carcinog Mutagen 2020;11 (2): 1000345.
- Fujioka K, Oishi M, Nakayama T, Fujioka A. Correlation between vascular failure (endothelial dysfunction) and fibrosis markers. Jpn J Med Ultrsonics. 2016; 43: Supplement S458.
- Fujioka K. NAFLD/NASH-related hepatocellular carcinoma: along with the role of genetics. J Cancer Oncol. 2020; 4(2): 000165.
- Fujioka K. A link between endothelial dysfunction and SARS-coV-2 infection in patients with COVID-19. CPQ Medicine 2021; 11(4): 01-08.
- Fujioka K. Cutaneous manifestation and vasculitis of COVID-19 in dermatology. Acta Sci Med Sci 2021; 5:16-19.
- Fujioka K. Clinical manifestation of endotheliitis in COVID-19 along with flow-mediated vasodilation study. J Clin Trials 2021; 11 (4): 1000469.
- Cholankeril G, Patel R, Khurana S, Satapathy SK. Hepatocellular carcinoma in non-alcoholic steatohepatitis: current knowledge and implications for management. World J Hepatol 2017; 9: 533-543.
- Grimaudo S, Pipitone RM, Pennisi G, Celsa C, Camma C, Marco VD, et al. Association between PNPLA3 rs738409 C>G variant and liver-related outcomes in patients with nonalcoholic fatty liver disease. Clin Gastronterol Hepatol. 2020; 18:935-944.
- Vilar-Gomez E, Caizadilla-Bertot L, Wai-Sun Wong V, Castellanos M, de la Fuente RA, Metwally M, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology. 2018; 155: 443-457.
- Piscaglia F, Svegliati-Baroni G, Barchetti A, Pecorelli A, Marinelli S, Tiribelli C, et al. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: a multicenter prospective study. Hepatology. 2016; 63:827-838.
- Gawrieh S, Dakhoul L, Miller E, Scanga A, deLemos A, Kettler C, et al. Characteristics, aetiologies and trends of hepatocellular carcinoma in patients without cirrhosis: a United States multiicentre study. Aliment Pharmacol Ther. 2019;50: 809-821.
- Stine JG, Wentworth BJ, Zimmet A, Rinella ME, Loomba R, Caldwell SH, et al. Systematic review with meta-analysis: risk of hepatocellular carcinoma in non-alcoholic steatohepatitis without cirrhosis compared to other liver diseases. Aliment Pharmacol Ther 2018; 48: 696-703.
- Mohamad B, Shah V, Onyshcheko M, Elshamy M, Aucejo F, Lopez R, et al. Characterization of hepatocellular carcinoma (HCC) in non-alcoholic fatty liver disease (NAFLD) patients without cirrhosis. Hepatol Int 2016; 10: 632-639.
- Bengtsson B, Stai P, Wahlin S, Bjorstrom N, Hagstrom H. Characteristics and outcome of hepatocellular carcinoma in patients with NAFLD without cirrhosis. Liver Intt. 2019; 39: 1098-1108.
- Anstee QM, Reeves HL, Kotsiliti E, Govaere O, Heikenwalder M. From NASH to HCC: current concepts and future challenges. Nat Rev Gastroenterol Hepatol 2019;16: 411-428.
- Loomba R, Lim JK, Patton H, EI-Serag HB. AGA clinical practice update on screening and surveillance for hepatocellular carcinoma in patients with nonalcoholic fatty liver disease: expert review. Gastroenterology 2020; 158: 1822-1830.
- Selvaraj EM, Mozes FE, Jayaswal ANA, Zafarmand MH, Vali Y, Lee JA, et al. Diagnostic accuracy of elastography and magnetic resonance imaging in patients with NAFLD: a systematic review and meta-analysis. J Hepatol 2021; 75: 770-785.
- Lupsor-Platon M, Serban T, Silion AI, Tirpe A, Florea M. Hepatocellular carcinoma and non-alcoholic fatty liver disease: a step forward for better evaluation using ultrasound elastography. Cancers. 2020 ;12: 2778.
- Kutlu O, Kaleli HN, and Ozer E. Molecular pathogenesis of nonalcoholic steatohepatitis- (NASH-) related hepatocellular carcinoma. Can J Gastroente Hepatol. 2018; 12(6) : 1-9.
- Ioannou GN. Epidemiology and risk-stratification of NAFLD-associated HCC. J Hepatol .2021 ; 75(6) : 1476-1484.
- Simon TG, King LY, Chong DQ, Nguyen L, Ma Y, VoPham T, et al. Diabetes, metabolic comorbidities, and risk of hepatocellular carcinoma: results from two prospective cohort studies. Hepatology 2018; 67: 1797-1806.
- Malaguamera R, Belfiore A. The emerging role of insulin and insulin-like growth factor signaling in cancer stem cells. Front Endocrinol. 2014; 5(1):1-10.
- Hagstrom H, Kechagias S, Ekstedt M. Risk for hepatic and extra-hepatic outcomes in nonalcoholic fatty liver disease. J Intern Med 2021; 12(7): 1-13.
- Yang JD, Ahmed F, Mara KC, Addissie BD, Allen AM, Gores GJ, et al. Diabetes is associated with increased risk of hepatocellular carcinoma in cirrhosis patients with nonalcoholic fatty liver disease. Hepatology 2020; 71: 907-916.
- Bhaskaran K, Douglas I, Forbes H, dos Santos-Silvia I, Leon D, Smeeth L. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet 2014; 384: 755-765.
- Grohmann M, Wiede F, Dodd G, Gurzov EN, Gurzov EN, Ooi GJ, et al. Obesity drives STAT-1-dependent NASH and STAT-3-dependent HCC. Cell 2018 ;175(5): 1289-1306.
- Lopez-Suarez A, Guerrero JMR, Elvira-Gonzalez J, Bettran-Robles M, Canas-Hormigo F, Bascunana-Quirell. Nonalcoholic fatty liver disease is associated with blood pressure in hypertensivie and nonhypertensive individuals from the general population with normal levels of alanine aminotransferase. Eur J Gatroenterol Hepatol 2011; 23: 1011-1017.
- Lorbeer R, Bayeri C, Auweter S, Rospleszcz S, Lieb W, Meisinger C, et al. Association between MRI-derived hepatic fat fraction and blood pressure in participants without history of cardiovascular disease. J Hypertens 2017; 35(3): 737-744.
- Lonardo A, Nascimbeni F, Mantovani A, Targher G. Hypertension, diabetes, atherosclerosis and NASH: cause or consequence? J Hepatol .2018 ;68(2): 335-352.
- Cai J, Zhang XJ, Ji YX, Zhang P, She ZG, Li H. Nonalcoholic fatty liver disease pandemic fuels the upsurge in cardiovascular diseases. Circ Res. 2020; 126: 679-704.
- Dogru T, Genc H, Tapan S, Ercin CN, Ors F, Asian F, et al. Elevated asymmetric dimethylarginine in plasma: an early marker for endothelial dysfunction in non-alcoholic fatty liver disease? Diabetes Res Clin Pract 2012; 96(1): 47-52.
- Li N, Zhang G-w, Zhang J-r, Jin D, Li Y, Liu T, et al. Non-alcoholic fatty liver disease is associated with progression of arterial stiffness. Nutr Metab Cardiovasc Dis 2015; 25(2): 218-223.
- Fan W, Qu X, Li J, wang X, Bai Y, Cao Q, et al. Associations between polymorphysms of the ADIPOQ gene and hypertension risk: a systematic and meta-analysis. Sci Rep 2017;9(2) 1-11.
- Liu M, Liu S, Shang M, Liu X, Wang Y, Li Q, et al. Association between ADIPOQ G276T and C11377G polymorphysms and the risk of non-alcoholic fatty liver disease: an update meta-analysis. Mol Genet Genomic Med 2019;7(5): e624
- Li L, Liu H, Hu X, Huang Y, Wang Y, He Y, et al. Identification of key genes in non-alcoholic fatty liver disease progression based on bioinformatics analysis. Mol Med Rep 2018; 17(6): 7708-7720.
- Zhang C and Yang M. The emerging factors and treatment options for NAFLD-related hepatocellular carcinoma. Cancers 2021; 13(5): 3740.
- Wang H, Lekbaby B, Fares N, Augustin J, Attout T, Schnuriger A, et al. Alteration of splicing factors’ expression during liver disease progression: impact on hepatocellular carcinoma outcome. Hepatol Int. 2019 ;13(4):454-467.
- Liang JQ, Teoh N, Xu L, Pok S, Li X, Chu ESH, et al. Dietary cholesterol promotes steatohepatitis related hepatocellular carcinoma through dysregulated metabolism and calcium signaling. Nat Commun 2018; 9(1): 4490.
- Ribas V, de la ROSA LC, Robles D, Nunez S, Segales P, Insausti-Urkia N, et al. Dierary and genetic cholesterol loading rather than steatosis promotes liver tumorigenesis and NASH-driven HCC. Cancers .2021; 13(5): 4091.
- Carlsson B, Linden D, Brolen G, LilJeblad M, Bjursell M, Romeo S, et al. Review article: the emerging role of genetics in precision medicine for patients with non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2020; 51(12): 1305-1320.
- Valenti LVC, Baselli GA. Genetics of nonalcoholic fatty liver disease: a 2018 update. Curr Pharm Des. 2018; 24(38): 4566-4573.
- Martin K, Hatab A, Athwal VS, Jokl E, Hanley KP. Genetic contribution to non-alcoholic fatty liver disease and prognostic implications. Curr Dia Rep. 2021; 21(3):8.
- Jamialahmadi O, Mancina RM, Ciociola E, Tavaglione F, Luukkonen PK, Baselli G, et al. Exome-wide association study on alanine aminotransferase identifies sequence variants in the GPAM and APOE associated with fatty liver disease. Gastroenterology 2021; 160: 1634-1646.
- Gellert-Kristensen H, Richardson T, Smith GD, Nordestgaard BG, Tybjaerg-Hansen A,Stender S. Combined effect of PNPLA3, TM6SF2, and HSD17B13 variants on risk of cirrhosis and hepatocellular carcinoma in the general population. Hepatology 2020; 72(3): 845-856.
- Trepo E, Valenti L. Update on NAFLD genetics: from new variants to the clinic. J Hepatol 2020; 72:1196-1209.
- Bianco C, Jamialahmadi O, Pelusi S, Baselli G, Dongiovanni P, Zanoni I, et al. Non-invasive stratification of hepatocellular carcinoma risk in non-alcoholic fatty liver using polygenic risk scores. J Hepatol 2021;74: 775-782.
- Long J, Bian J, Zhao H. Polygenic risk score: a promising predictor for hepatocellular carcinoma in the population with non-alcoholic fatty liver disease. J Hepatol 2021; 74: 1493-1494.
- Jamialahmadi O Bianco C, Pelusi S, Romeo S, Valenti L. Reply to: “Polygenic risk score: a promising predictor for hepatocellular carcinoma in the population with non-alcoholic fatty liver disease”. J Hepatol 2021; 74: 1491-1496.
Citation: Fujioka K (2021) Polygenic Risk Score in NAFLD/NASH-Associated Hepatocellular Carcinoma Along With Multifactorial Process. J Carcinog Mutagen. 12:370.
Copyright: © 2021 Fujioka K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.