Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 9, Issue 1
Physician Practice Habits Treating Claudicants who Smoke
Anthony Feghali1*, Stephanie Rakestraw2, Albert Crawford2, Babak Abai2, Dawn Salvatore2 and Paul DiMuzio22Department of Vascular Surgery, Thomas Jefferson University, Philadelphia, PA 19107, United States
Received: 04-Jan-2021 Published: 28-Jan-2021, DOI: 10.35248/2329-6925.9.37.404
Abstract
Introduction: Peripheral Arterial Disease (PAD) affects over 200 million people worldwide, with 30%-40% of patients presenting with intermittent claudication. Smoking is the most important modifiable risk factor in treating PAD. Smoking cessation is currently recommended before surgical intervention for intermittent claudication, but interventions are offered and conducted on a physician-specific basis. Our study aimed to identify global trends in surgical intervention for intermittent claudication in active smokers.
Methods: A 14-question survey was sent to members of the Society of Vascular Surgery (SVS) to collect information on demographics of the respondent and their intervention strategy in active smokers. A total of 729 interventions lists responded from every geographic region. Survey results were compiled and analyzed to determine trends in surgical intervention by geographic region, specialty, and years in practice.
Results: Physicians in North America were less willing to perform open (56.7% vs. 69.9% in Asia, 67.6% in Europe, and 66.7% of other regions, p=0.024) or endovascular surgery (68.4% vs. 77.1% of Asian physicians, 75.0% of European physicians, 74.2% of other regions, p=0.24) on actively smoking claudicants than physicians in other geographic regions. Asian and North American physicians were more likely to insist on one-month of smoking cessation prior to intervention (57.1% in Asia, 56.6% in North America vs. 34.9% in Europe and 40.1% in other regions, p=0.0003). Physicians with more years in practice (over 10 years) had an impact on open surgeries offered to active smokers (57.7% for <10 years vs. 67.7% for 10-20 years and 68.6% for >20 years, p=0.017), but did not significantly impact the offering of endovascular intervention (77.8% for 10-20 years vs. 69.5% for <10 years and 71.9% for >20 years, p=0.13).
Conclusion: Surgical interventions offered to actively-smoking claudicants vary by geographic region and physician years in practice. Physicians in regions of lower tobacco use prevalence are less willing to offer intervention to active smokers. Physicians with more years in training are more willing to offer open intervention to active smokers. Additional studies should be conducted as tobacco use trends change and to further evaluate the variations in provider specialty.
Keywords
Intermittent claudication; Tobacco using; Smoking; Endovascular; Vascular surgery; Peripheral arterial disease
Introduction
Peripheral arterial disease (PAD) affects over 200 million people worldwide, with 30%-40% of these patients presenting with claudication [1-5]. In North America and Europe over 410,000 inpatient admissions annually are attributed to PAD (3). However, the majority of PAD patients (70%) live-in low-income regions of the world with over 100 million in Asia [2]. Between 2000 and 2010, the number of PAD patients increased by 29% in low income countries and 13% in high income countries [2]. Among risk factors for PAD, tobacco abuse is the most important modifiable risk factor. Over 30% of patients with peripheral vascular disease are current smokers [4]. Smoking is known to increase the incidence of peripheral vascular disease more than threefold in a dose-dependent fashion by pack-year history. The Framingham Heart Study found that the risk for claudication was directly correlated with the number of cigarettes smoked [4]. There was a 1.4-fold increase risk of claudication for every 10 cigarettes smoked per day [6]. By quitting smoking, patients have better outcomes from cardiovascular disease to overall post-operative mortality. The Society for Vascular Surgery (SVS) gives smoking cessation for the medical management of intermittent claudication a 1A rating [4].
Prior studies have focused on quitting smoking before endovascular or surgical intervention. However, studies show less than 25% of these quit attempts are successful [4]. As many as 44% of patients are active smokers at the time of intervention [7]. Active tobacco use must therefore be considered when determining treatment options for peripheral vascular disease. In a review of Vascular Quality Initiative (VQI) records from interventions in the United States, active smoking status did not appear to influence the rate of open surgical intervention for intermittent claudication [4]. Little is known however about the influence of smoking on treatment on a global scale. We hypothesized that regions with a higher overall rate of tobacco use would be more willing to pursue invasive vascular interventions on claudicants who are active smokers.
The aim of this study was to determine the impact of active tobacco use on claudication intervention worldwide. This study provides a novel method of data collection by using social media to survey members of the Society of Vascular Surgery globally. This approach allowed responses to be collected from a variety of SVS. providers around the world from different practice types. We also analyzed years in practice to identify trends in invasiveness of interventions offered to active smokers.
Methods
In December 2017 to February 2018 surveys were distributed via Survey Monkey to all members of the Society of Vascular Surgery social media database. Our goal was to reach different providers across the world and see their practice habits and views on treating patients with claudication who smoke. A 14-question survey was shared with members nationally and internationally. Of 5800 members for who adequate contact information was available via email addresses, 837 responded, for a response rate of 17%.
Questions asked included physician characteristics-country of practice (recoded to continent), medical/surgical specialty, years in practice, type of fellowship training, approaches to treating claudicants-perform endovascular surgery, perform open surgery, duration of smoking cessation required of patients, how to verify that patients have stopped smoking, what services are offered to help patients stop smoking, and whether the physician treats patients who use e-cigarettes the same as smokers. For variables where respondents answered “other, specify” and provided more detailed answers, whenever possible, the authors recoded the detailed responses into the original categories. Due to 87% of respondents being vascular surgeons, other respondent specialties were excluded from analysis.
The 6 treatment variables were cross tabulated with the 4 physician characteristics, with the Chi-square test employed to assess statistical significance, with a=.05.
Results
We had a total of 837 responses, including 34% of responses from the US, 35% from Europe, 15% from Asia, and 6% from South America, and 10% from Africa and the Pacific nations. Further 87% of the respondents were vascular surgeons, 3% interventional radiologists, and 2% interventional cardiologists. About 45% of respondents have been in practice less than 10 years with 55% being in practice over 10 years (27.1% for 10-20 years and 27.5% for over 20 years). Demographic information is shown in Table 1.
| Number (n=708) | Percentage | ||
|---|---|---|---|
| Geographic region | Asia | 86 | 12.23 |
| Europe | 256 | 36.42 | |
| North America | 295 | 41.96 | |
| Other | 66 | 9.39 | |
| Years in practice | <10 years | 320 | 45.39 |
| 10-20 years | 191 | 27.09 | |
| >20 years | 194 | 27.52 | |
| Gender | Female | 102 | 14.43 |
| Male | 605 | 85.57 | |
| Hospital size | <100 beds | 41 | 5.81 |
| 100-400 beds | 207 | 29.32 | |
| >400 beds | 458 | 64.87 | |
| Area of practice | Rural | 43 | 6.11 |
| Suburban | 138 | 19.6 | |
| Urban | 523 | 74.29 |
Table 1: Respondent demographic information.
Vascular surgeons in North America were less willing to perform open surgery on claudicants who smoke than in any other geographic region (56.7% vs. 69.9% in Asia, 67.6% in Europe, and 66.7% of other regions, p=0.024) (Figure 1a). Vascular surgeons in North America were also less willing to perform endovascular surgery on claudicants who smoke than physicians in other geographic regions (68.4% vs. 77.1% of Asian physicians, 75.0% of European physicians, 74.2% of those in other regions, p=0.24) (Figure 1b).
Figure 1a: Percentages of respondents who perform open surgery on actively smoking claudicants. North American physicians have the lowest rate of open surgery on active smokers (p=0.024).
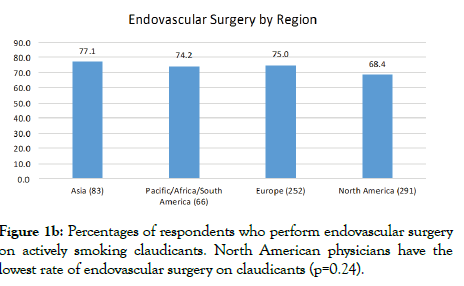
Figure 1b: Percentages of respondents who perform endovascular surgery on actively smoking claudicants. North American physicians have the lowest rate of endovascular surgery on claudicants (p=0.24).
Physicians in Asia and North America were more likely to insist on smoking cessation for one month before intervention than physicians in Europe or other regions (57.1%, 56.6% vs. 34.9%, 40.1%, p=0.0003) (Figure 2a). Physicians in North America were more likely to take a patient’s word that they had stopped smoking (81.0%), while physicians in Asia were less likely to trust patientreported cessation (37.6%). Physicians in Europe and other regions were somewhat likely to trust patient-reported smoking cessation (69.5%, 59.1%, p <0.0001) (Figure 2b).
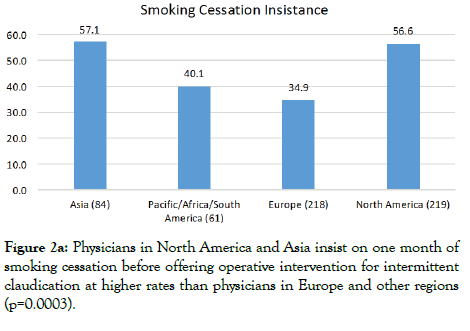
Figure 2a: Physicians in North America and Asia insist on one month of smoking cessation before offering operative intervention for intermittent claudication at higher rates than physicians in Europe and other regions (p=0.0003).
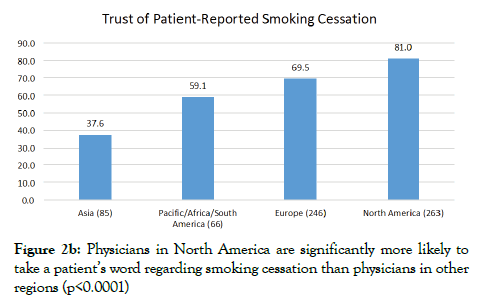
Figure 2b: Physicians in North America are significantly more likely to take a patient’s word regarding smoking cessation than physicians in other regions (p<0.0001)
Years in practice also affected the surgical interventions offered to patients who smoke. Physicians with less than 10 years in practice were less likely to perform open surgery on smokers than physicians with 10 or more years in practice (57.7% vs. 67.7%, 68.6%, p=0.017) (Figure 3a). There was a trend towards physicians with 10-20 years in practice being more willing than other groups to perform endovascular surgery (77.8% vs. 69.5%, 71.9%, p=0.13) (Figure 3b).
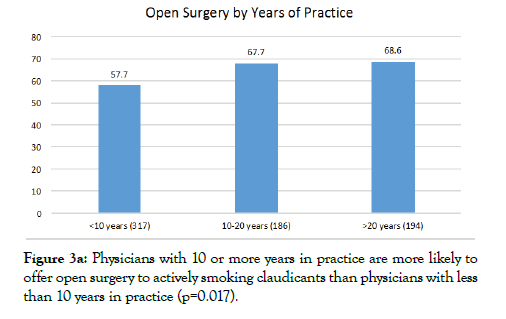
Figure 3a: Physicians with 10 or more years in practice are more likely to offer open surgery to actively smoking claudicants than physicians with less than 10 years in practice (p=0.017).
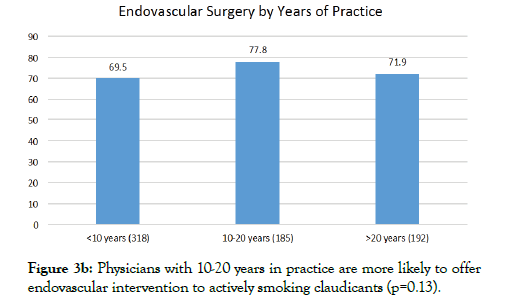
Figure 3b: Physicians with 10-20 years in practice are more likely to offer endovascular intervention to actively smoking claudicants (p=0.13).
Discussion
Tobacco use is one of the greatest risk factors for peripheral arterial disease (PAD) [3]. First-line treatment of intermittent claudication consists of smoking cessation, antiplatelet therapy, supervised walking, and statin therapy. Failure of first-line treatment and lifestyle-limiting claudication are indications for surgical intervention, although some physicians can be hesitant to intervene upon patients who are still smoking.
This study was conducted to analyze the impact of smoking on the offering of surgical intervention to claudicants in different geographic regions. This study was unique in that it illustrates a different approach to gaining insight into physician practice habits. By using a survey via the SVS. email platform, we were able to collect data on over 800 physicians globally.
There are a larger proportion of physicians willing to perform open surgery on claudicants who smoke outside of North America. This difference could be due to differences in tobacco use rates between regions. As of 2015, the World Health Organization estimates that roughly 1.1 billion people smoke. Far more males than females smoked tobacco. Although tobacco use rates are declining worldwide, the prevalence of tobacco smoking appears to be increasing in the WHO Eastern Mediterranean Region and the African Region. Smoking rates in the United States have dropped by over 50% from 1996 to 2012 [8]. In Western nations there continues to be a decline in tobacco use rates. However in Asia, tobacco use continues to rise. The largest rates of tobacco use are still seen in Asia, with Europe, South America, and Africa all having >30% of the population using tobacco (Figure 4). About one in every 3 cigarettes smoked worldwide are in China with over 50% of adult men there who currently smoke [9]. In fact, the number of cigarettes consumed in China in 2009 were more than the other top four tobacco-consuming countries combined (Indonesia, Japan, Russia, and the U.S).
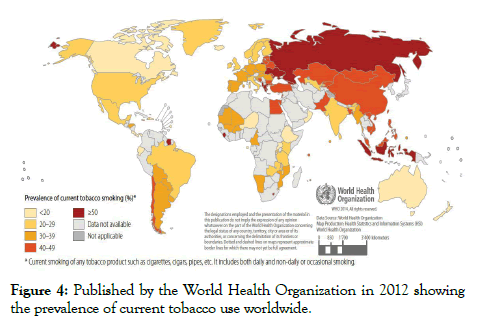
Figure 4: Published by the World Health Organization in 2012 showing the prevalence of current tobacco use worldwide.
Interestingly, our study showed more Asian physicians insisting on one month of smoking cessation prior to surgical intervention than physicians in any other region. Additionally, North America physicians were more likely to trust patient-reported smoking cessation while Asian physicians were more likely to be skeptical of self-reported smoking cessation. This trend could be a response to increasing rates of tobacco use in Asian nations and decreasing rates of tobacco use in North America.
Physicians with more years in practice were more likely to perform open surgery on claudicants who smoke. This trend was not as clear for endovascular surgery. There could be numerous reasons for this difference. Physicians with more than 20 years in practice were trained before the onset of the endovascular era and could be more comfortable with open procedures. More time in practice could also lend itself to a more skilled physician who is more willing to perform an open procedure. However, in light of the current warnings associated with paclitaxel-eluting stents, there could be a reduction in physicians offering endovascular treatment to smokers since the rate of stent failure could further increase [10].
The methods of this study have limitations. The survey was distributed via SVS. email and social media, requiring respondents to be those with an online presence. The study is also limited in the types of providers. The majority of responses was from vascular surgeons and did not capture a large number of intervention lists. Further study could be done with the Societies of Cardiology and Interventional Radiology to determine differences in interventions offered to smokers among all physicians treating PAD. Additionally, the response from physicians in South America, Africa, and the Pacific was not very robust. Given the low rate of tobacco use in Australia in contrast to the high rates of use in other Pacific nations, South America, and Africa, an increased response from these nations could show even more striking practice differences.
Despite the limitations of this study, it provides potential insight into understanding physician practice habits across specialty, nation, and years in practice. More work should be done to analyze changes in practice habits as tobacco use rates change. Another potential area of study is differences in treatments offered to males who smoke versus females who smoke, particularly in Asian nations where >50% of males smoke, but only 2.6% of females [11-13].
Conclusions
Increased prevalence of tobacco use and years in practice can impact physician decision making in intervention for intermittent claudication. Physicians in areas of increased tobacco use are more likely to offer intervention to claudicants who continue smoking, but are also more skeptical of patient-reported smoking cessation. Additional study in under-represented regions and specialties could provide more insight into the impact of active smoking on claudication treatment.
REFERENCES
- Dhaliwal G, Mukherjee D. Peripheral arterial disease: Epidemiology, natural history, diagnosis and treatment. Int J Angiol. 2007;16(2):36-44.
- Fowkes FG, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382(9901):1329-1340.
- Allison M, Ho E, Denenberg J, Langer R, Newman A, Fabsitz R, et al. (2007). Ethnic-Specific Prevalence of Peripheral Arterial Disease in the United States. Am J Prev Med. 2007;32(4):328-333.
- Kearns BC, Thomas SM. Cost-effectiveness of superficial femoral artery endovascular interventions in the UK and Germany: a modelling study. BMJ open. 2017;7(1):e013460.
- Fowkes FGR, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382(9901):1329-1340.
- Conen D, Everett BM, Kurth T. Smoking, smoking cessation, and risk for symptomatic peripheral artery disease in women: a cohort study. Ann Intern Med. 2011;154(11):719-726.
- Smeds M, Privratsky A, Thrush C, Barone C, Escobar G, Ali A, et al. Nicotine Dependence and Willingness to Quit Smoking in Vascular Surgery Patients. Ann Vasc Surg. 2017;45:144-153.
- Dwyer-Lindgren L, Mokdad A, Srebotnjak T, Flaxman A, Hansen G, Murray C. Cigarette Smoking Prevalence in US Counties: 1996-2012. Popul Health Metr. 2014;12(1):5.
- Vivian Tan, World Health Organization. Tobacco in China. 2019.
- Food and Drug Administration (FDA). Treatment of Peripheral Arterial Disease with Paclitaxel-Coated Balloons and Paclitaxel-Eluting Stents Potentially Associated with Increased Mortality. 2019.
- Liu S, Zhang M, Yang L, Li Y, Wang L, Huang Z, et al. Prevalence and patterns of tobacco smoking among Chinese adult men and women: findings of the 2010 national smoking survey. J Epidemiol Community Health. 2017;71(2):154-161.
- Dwyer-Lindgren L, Mokdad A, Srebotnjak T, Flaxman A, Hansen G, Murray C. Cigarette Smoking Prevalence in US Counties: 1996-2012. Population Health Metrics. 2014.
- Kearns BC, Thomas SM. Cost-effectiveness of superficial femoral artery endovascular interventions in the UK and Germany: a modelling study. BMJ open. 2017;7(1):e013460.
Citation: Feghali A, Rakestraw S, Crawford A, Abai A, Salvatore D, DiMuzio P (2021) Physician Practice Habits Treating Claudicants who Smoke. J Vasc Med Surg. 9: 404.
Copyright: © 2021 Feghali A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited

