Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
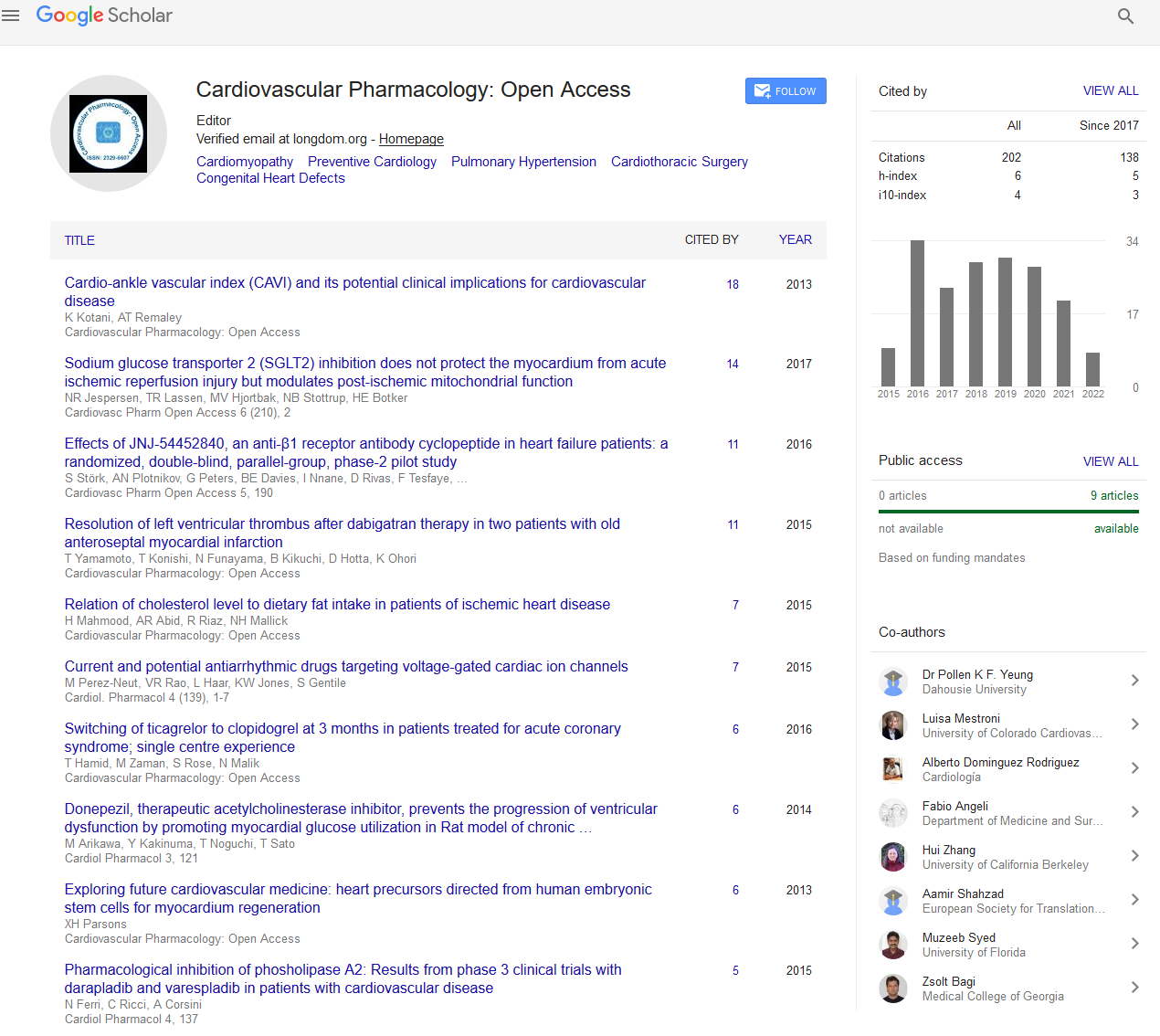
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2024) Volume 13, Issue 1
Pharmacological Interventions to Combat Thrombosis in Cardiovascular Disorders
Peter Keneally*Received: 04-Mar-2024, Manuscript No. CPO-24-25980 (PQ); Editor assigned: 06-Mar-2024, Pre QC No. CPO-24-25980 (PQ); Reviewed: 20-Mar-2024, QC No. CPO-24-25980 (PQ); Revised: 27-Mar-2024, Manuscript No. CPO-24-25980 (R); Published: 03-Apr-2024, DOI: 10.35248/2329-6607.24.13.389
Description
Thrombosis, the formation of blood clots within blood vessels, carriages a significant risk in cardiovascular disorders. From heart attacks to strokes, thrombosis can lead to severe complications and even mortalities if not managed effectively. Pharmacological interventions have long been a cornerstone in combating thrombosis, continually evolving to enhance efficacy and minimize adverse effects.
One of the primary pharmacological interventions in thrombosis management is antiplatelet therapy. Aspirin, a classic example, inhibits platelet aggregation by irreversibly acetylating cyclooxygenase, thereby disrupting the synthesis of thromboxane A2, a potent platelet activator. While aspirin remains a basis in preventing thrombosis in cardiovascular disorders, innovative antiplatelet agents have emerged to report limitations such as resistance and gastrointestinal side effects. Clopidogrel, prasugrel, and ticagrelor are examples of P2Y12 receptor antagonists that offer potent and more predictable antiplatelet effects, reducing the risk of thrombotic actions in patients with acute coronary syndromes and those experiencing percutaneous coronary interventions.
Anticoagulant therapy is another critical pharmacological approach in thrombosis management, particularly in conditions like atrial fibrillation and venous thromboembolism. Vitamin K antagonists, such as warfarin, have been widely used for decades to inhibit the synthesis of clotting factors II, VII, IX, and X. However, their narrow therapeutic window, need for frequent monitoring, and interactions with various foods and drugs have spurred the development of innovative oral anticoagulants. Direct oral anticoagulants (DOACs), including dabigatran, rivaroxaban, apixaban, and edoxaban, offer more predictable anticoagulant effects and have demonstrated non-inferiority or superiority to warfarin in preventing thromboembolic dealings while reducing the risk of bleeding complications.
Thrombolytic therapy represents a more aggressive pharmacological intervention aimed at rapidly dissolving existing blood clots. Tissue Plasminogen Activator (tPA) is the prototypical thrombolytic agent, catalyzing the conversion of plasminogen to plasmin, which degrades fibrin, the main component of blood clots. Thrombolytic therapy is primarily indicated in acute settings, such as myocardial infarction and ischemic stroke, where prompt restoration of blood flow is paramount to prevent tissue damage and improve clinical results. However, thrombolytic therapy carries inherent risks, including an increased risk of bleeding, particularly intracranial hemorrhage, necessitating careful patient selection and weighing the benefits against the risks.
Emerging pharmacological strategies in thrombosis management focus on targeting innovative methods involved in thrombus formation while minimizing adverse effects. One capable approach is the development of Protease-Activated Receptor (PAR) antagonists. PARs play an important role in platelet activation and thrombus formation upon exposure to thrombin. PAR-1 antagonists like vorapaxar have shown efficacy in reducing cardiovascular actions in patients with a history of myocardial infarction or peripheral artery disease, albeit with an increased risk of bleeding, particularly in patients with a history of stroke or transient ischemic attack.
Another area of active study is the modulation of coagulation cascade components beyond traditional targets. Factor XI, a component of the intrinsic coagulation pathway, has garnered attention as a potential target for antithrombotic therapy. Inhibition of factor XI may offer antithrombotic effects with a lower risk of bleeding compared to existing anticoagulants, as demonstrated in preclinical studies and early-phase clinical trials. Several factor XI inhibitors are currently under investigation, property ability for impending pharmacological interventions in thrombosis management.
Conclusion
Pharmacological interventions play a principal role in combating thrombosis in cardiovascular disorders. From antiplatelet and anticoagulant therapy to thrombolytic agents and original pharmacological targets, advancements continue to expand treatment options and improve outcomes for patients at risk of thrombotic events. However, the optimal selection and timing of pharmacological interventions require careful consideration of individual patient characteristics, underlying comorbidities, and the balance between thrombotic and bleeding risks. Arriving study efforts target to supplementary refine pharmacological strategies and concrete the way for personalized approaches to thrombosis management in cardiovascular disorders.
Citation: Keneally P (2024) Pharmacological Interventions to Combat Thrombosis in Cardiovascular Disorders. Cardiovasc Pharm. 13:389.
Copyright: © 2024 Keneally P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.