Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
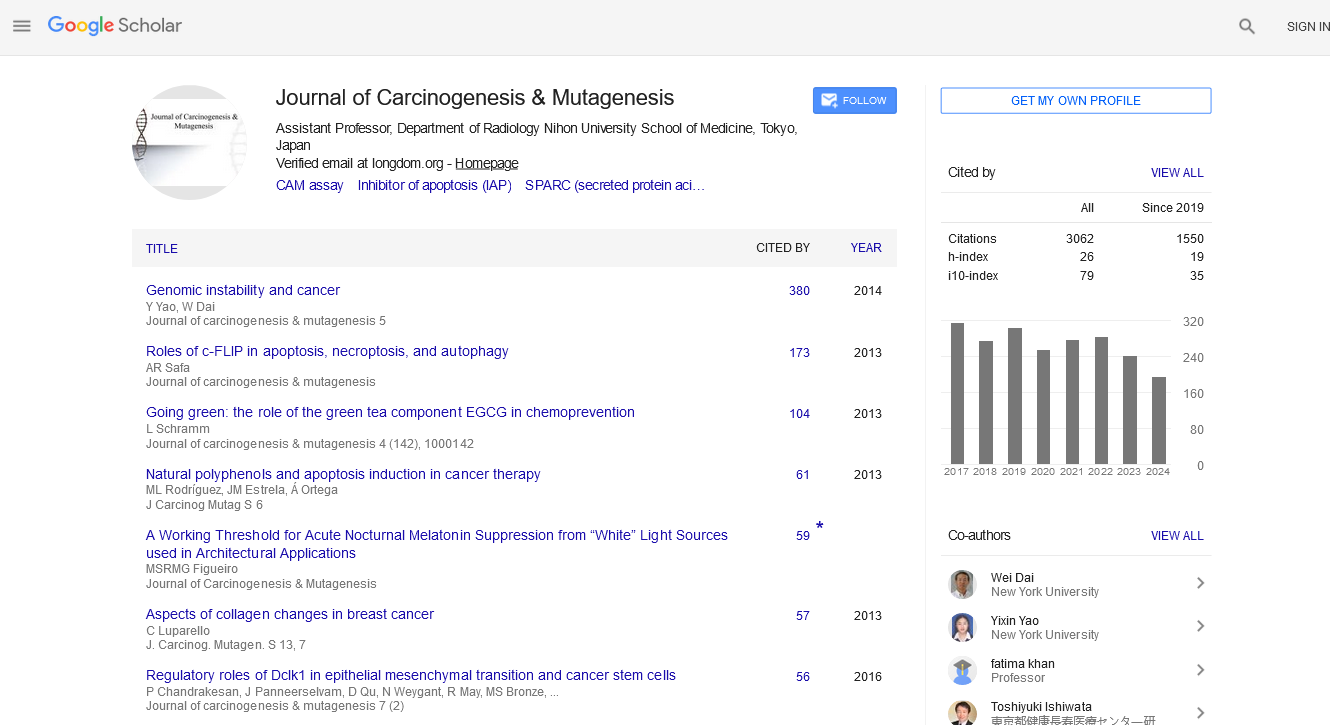
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2024) Volume 0, Issue 0
Personalized Medicine Approaches for Effective Cancer Management of Immuno-Oncology
Huchang Liao*Received: 30-Jul-2024, Manuscript No. JCM-24-26906; Editor assigned: 01-Aug-2024, Pre QC No. JCM-24-26906 (PQ); Reviewed: 15-Aug-2024, QC No. JCM-24-26906; Revised: 22-Aug-2024, Manuscript No. JCM-24-26906 (R); Published: 30-Aug-2024, DOI: 10.35248/2157-2518.24.S45.005
Description
Immuno-oncology, a rapidly advancing field within cancer research and treatment, focuses on using the body’s immune system to fight cancer. By harnessing the natural ability of immune cells to recognize and destroy abnormal cells, immuno-oncology is transforming the landscape of cancer therapy. This article explores the principles of immuno-oncology, current therapeutic strategies and the promising future of this innovative approach.
The immune system and cancer
The immune system plays a critical role in protecting the body from pathogens and abnormal cells, including cancer cells. Under normal circumstances, immune cells such as T cells, Natural Killer (NK) cells and macrophages are capable of identifying and eliminating cancerous cells. However, cancer cells often develop mechanisms to evade immune detection, leading to tumor growth and progression.
Immuno-oncology aims to overcome these mechanisms and restore the immune system's ability to target and destroy cancer cells effectively. This field encompasses a range of therapeutic strategies designed to enhance or restore the immune response against tumors.
Key strategies in immuno-oncology
Checkpoint inhibitors: One of the most significant breakthroughs in immuno-oncology is the development of checkpoint inhibitors. These drugs work by blocking proteins that inhibit immune responses, such as PD-1 (programmed death-1) and CTLA-4 (Cytotoxic T-Lymphocyte-Associated Protein 4). By inhibiting these proteins, inhibitors effectively unleash the immune system to target cancer cells more aggressively. Notable examples include pembrolizumab (Keytruda) and nivolumab (Opdivo), which have shown remarkable efficacy in treating various cancers, including melanoma, lung cancer and bladder cancer.
CAR-T cell therapy: Chimeric Antigen Receptor T-cell (CAR-T) therapy is a revolutionary approach that involves modifying a patient’s own T cells to express artificial receptors targeting specific cancer antigens. Once these engineered T cells are infused back into the patient, they can recognize and attack cancer cells more effectively. CAR-T therapy has demonstrated dramatic responses in hematologic malignancies, such as Acute Lymphoblastic Leukemia (ALL) and large B-cell lymphoma, with treatments like Kymriah and Yescarta leading the way.
Cancer vaccines: Therapeutic cancer vaccines aim to stimulate the immune system to recognize and attack cancer cells. Unlike preventive vaccines, therapeutic vaccines are designed for patients who already have cancer. These vaccines often include tumor-specific antigens or proteins that help the immune system recognize cancer cells as threats. The FDA-approved vaccine Sipuleucel-T (Provenge) for prostate cancer is an example, where patients’ dendritic cells are exposed to a prostate cancer antigen to elicit a targeted immune response.
Monoclonal antibodies: Monoclonal antibodies are laboratory- made molecules designed to bind specifically to cancer cells or proteins involved in cancer growth. They can work by directly targeting cancer cells for destruction or by blocking the signals that promote tumor growth. Drugs such as trastuzumab (Herceptin) and rituximab (Rituxan) are used to treat cancers with specific molecular targets, including HER2-positive breast cancer and CD20-positive lymphoma, respectively.
Challenges and future directions
While immuno-oncology has achieved significant advancements, several challenges remain. One major issue is the variability in patient responses to immunotherapies. Not all patients benefit equally and some may experience immune-related adverse events. Understanding the reasons behind these differences is important for optimizing treatment strategies.
Additionally, the high cost of immunotherapy and the need for specialized manufacturing processes, particularly for CAR-T therapy, present logistical and economic challenges. Expanding access to these cutting-edge treatments and reducing costs will be essential for broader implementation.
The future of immuno-oncology looks promising as research continues to evolve. Advances in understanding the tumor microenvironment, developing combination therapies and identifying new biomarkers for patient selection are likely to enhance the effectiveness of immunotherapy. Ongoing clinical trials are exploring novel approaches, such as bispecific antibodies and oncolytic virus therapy, which may further revolutionize cancer treatment.
Conclusion
Immuno-oncology represents a paradigm shift in cancer treatment by harnessing the power of the immune system to target and destroy cancer cells. With innovative therapies like checkpoint inhibitors, CAR-T cell therapy, cancer vaccines and monoclonal antibodies, this field offers new hope for patients with various types of cancer. As research and technology continue to advance, immuno-oncology is poised to become an integral part of cancer care, moving us closer to a future where cancer can be effectively managed or even eradicated.
Citation: Liao H (2024). Personalized Medicine Approaches for Effective Cancer Management of Immuno-Oncology. J Carcinog Mutagen. S45:005.
Copyright: © 2024 Liao H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.