Indexed In
- Open J Gate
- Genamics JournalSeek
- CiteFactor
- Cosmos IF
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Proquest Summons
- Scholarsteer
- ROAD
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
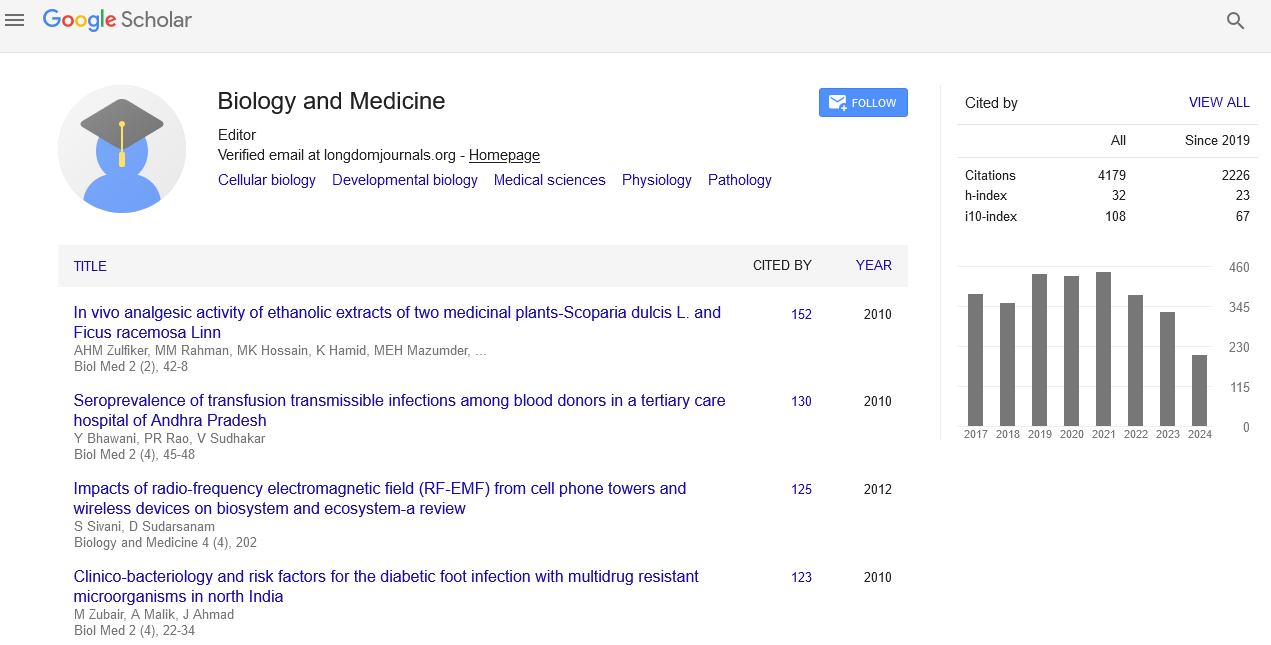
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2022) Volume 14, Issue 6
Pathogenicity of Neuroendocrine Tumors of Pancreas
Olivia Wu*Received: 26-May-2022, Manuscript No. BLM-22-17412; Editor assigned: 30-May-2022, Pre QC No. BLM-22-17412(PQ); Reviewed: 13-Jun-2022, QC No. BLM-22-17412; Revised: 20-Jun-2022, Manuscript No. BLM-22-17412(R); Published: 27-Jun-2022, DOI: 10.35248/0974-8369.22.14.494
Description
Pancreatic Neuroendocrine Tumors (PNETs) are a group of endocrine tumors that develop in the pancreas and are one of the most common neuroendocrine tumors. The genetic causes of familial and sporadic PNETs are reasonably understood, but their molecular causes are still unknown. Most Pancreatic neuroendocrine tumors are indolent, but can be malignant. The biological behaviour of a single PNET is unpredictable. Highgrade tumors, lymph node and liver metastases, and large tumor sizes generally indicate a poor prognosis. Pancreatic neuroendocrine tumors are a group of cancers that can occur in hormone-producing cells of the pancreas. Neuroendocrine tumors of the pancreas, also known as islet cell carcinoma, are extremely rare.
Neuroendocrine tumors of the pancreas begin with the small hormone-producing cells (islet cells) commonly found in the pancreas. Some neuroendocrine tumor cells in the pancreas continue to secrete hormones (known as functional tumors) and overproduce the hormones given to the body. Examples of these types include gastrinoma and glucagonoma. Many times these tumors do not secrete an excess amount of these hormones (known as non-functional tumors).
Pancreatic neuroendocrine tumors occur when pancreatic hormone-producing cells (islet cells) undergo changes (mutations) in their DNA. It is a material that directs all chemical processes in the body. DNA mutations cause changes in these Islet cells. The cells can begin to grow out of control and eventually form tumors, which are masses of cancer cells. Cancer cells can divide repeatedly and spread to other organs, such as the liver. Neuroendocrine tumor of the pancreas often referred to as "islet cell tumor" or "pancreatic endocrine tumor".
PanNETs are one type of neuroendocrine tumor, representing about one-third of gastroentero pancreatic neuroendocrine tumors. Many PanNETs are benign and some are malignant. Aggressive PanNET tumors have traditionally been termed as “islet cell carcinoma".
PanNETs are quite distinct from the usual form of pancreatic cancer, as the majority of which are adenocarcinomas, which arises from the exocrine pancreas. Only 1% or 2% of clinically significant pancreas neoplasms are PanNETs.
Some PanNETs do not cause any symptoms; they may be diagnosed incidentally on a CT scan performed for a different purpose. Symptoms such as abdominal or back pain or pressure, diarrhea, indigestion, or yellowing of the skin will occur. About 40% of PNETS have symptoms related to excessive secretion of hormones or active polypeptides and are accordingly labelled as "functional"; the symptoms reflect the type of hormone secreted. Up to 60% of PanNETs are non-secretory or non-functional, in which there is no secretion, or the quantity or type of products, such as pancreatic polypeptide, chromogranin A, and neurotensin, do not cause a clinical syndrome although blood levels may be elevated. In total, 85% of PanNETs have an elevated blood marker because symptoms are non-specific, diagnosis is often delayed. Measurement of hormones including pancreatic polypeptide, gastrin, proinsulin, insulin, glucagon, and vasoactive intestinal peptide can determine if a tumor is causing hypersecretion.
Multiphase CT and MRI are the primary diagnostic methods for morphologic imaging of PNETs. While MRI is superior to CT for imaging, both of the primary tumors and evaluation of metastases, CT is more readily available. Notably, while many malignant lesions are hypo dense in contrast-enhanced studies, the liver metastases of PNETs are hyper vascular and readily visualized in the late arterial phase of the post-contrast CT study. However, morphological imaging alone is not sufficient for a definite diagnosis.
On biopsy, immunohistochemistry is generally positive for chromogranin and synaptophysin. In general, treatment for PanNET encompasses the same array of options as like other neuroendocrine tumors. In functioning PanNETs, octreotide is usually recommended prior to biopsy or surgery, but in generally avoided in insulinomas to avoid profound hypoglycemia.
PanNETs in Multiple endocrine neoplasia type 1 are often multiple, and requires different treatment methods and surveillance strategies. Some PanNETs are more responsive to chemotherapy than gastroenteric carcinoid tumors. Several agents have shown activity when subjected to chemotherapy. In well differentiated PanNETs, chemotherapy is used as a treatment method generally reserved for when there are no other treatment options. Combinations of several medicines have been used, such as doxorubicin with streptozocin and fluorouracil and capecitabine with temozolomide as medications for treatment of PNETs.
Citation: Wu O (2022) Pathogenicity of Neuroendocrine Tumors of Pancreas. Bio Med. 14:494.
Copyright: © 2022 Wu O. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.