Indexed In
- Open J Gate
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2024) Volume 13, Issue 3
Opportunistic Invasive Fungal Infections
Saqib Bashir*, Aasia Sofi, Hanan and Jaya BhartiReceived: 03-Apr-2020, Manuscript No. CMO-24-3784; Editor assigned: 08-Apr-2020, Pre QC No. CMO-24-3784 (PQ); Reviewed: 22-Apr-2020, QC No. CMO-24-3784; Revised: 15-Jul-2024, Manuscript No. CMO-24-3784 (R); Published: 12-Aug-2024, DOI: 10.35248/2327-5073.24.13.399
Abstract
Invasive fungal infections (opportunistic) are significant wellbeing complications in immune compromised patients and in terminal stages of chronic diseases. The signs and manifestations differ and can range from colonization in hypersensitive bronchopulmonary sickness to dynamic infection by local infective agents. Many factors impact the seriousness and infection causing capacity of the fungus, for example, chemicals, dimorphic development in some Candida species, melanin creation and poison creation. Infection is affirmed when histopathology study is finished with the assistance of special stains shows fungal tissue involvement or when the infective agent is gotten from clinical examples by culture. Both obtained and intrinsic immunodeficiency may be related with increased weakness to systemic infections. Fungal infection can’t be treated because antifungal therapy for Candidiasisis still controversial and for molds, the clinician must have to affirm that the species acquired from the culture medium is the pathogen. Convenient inception of antifungal treatment is a basic segment influencing the results. The general spreading fungal infection requires the utilization of foundational operators with or without surgical activities and in some cases immunotherapy is additionally used. Preclinical and clinical examinations show a decent connection between medicate portion and treatment result. Medication portion movement is essential to ensure that therapeutic levels are accomplished for ideal clinical results. The goal of this audit is to examine opportunistic fungal infections, diagnostic methods and the administration of these diseases.
Keywords
Fungal disease; Medication; Laboratory methods; Opportunistic fungal diseases
Introduction
Some saprophytic fungus do not cause malady yet they can cause infection under some significant conditions for example, immune compromised persons and in terminal stages of chronic disease. These are called opportunistic fungi and the infection caused by them is called Invasive Fungal Infections (IFI).
Invasive Fungal Infections (IFI) (opportunistic) are spreading rapidly because due to advances in clinical consideration, widespread utilization of anti-microbials, corticosteroids and due to immunosuppressive medications. These types of contagious species are present in soil, plant debris and other natural substances and make up roughly 7 percent (611,000 species) of every single eukaryotic species on earth, out of which only about 600 species are human pathogen [1].
The variables responsible for Invasive Fungal Infections (IFI) include patients with neutropenia, hematological malignancies, bone marrow transplantation, patients taking wide-range antitoxins and delayed utilization of corticosteroids for treatment and chemotherapy, patients with HIV disease, invasive clinical procedures and because of resistant immune suppressive agents. Other risk factors are diabetes mellitus, lack of healthy nutrition, solid organ transplantation and significant medical procedure. There are also reports of the presence of infection in immunocompetent patients without signs or side effects of conditions related with immune compromised status.
Disease can be transmitted by the inward breath of spores, percutaneous immunization in cutaneous and subcutaneous diseases entrance into the mucosa by commensal living beings for example, Candida albicans and the ingestion of a poison in contaminated nourishment or drink (gastrointestinal disease) [2].
Case Presentation
Candidiasis
The causative agent of this fungal infection is Candida albicans (80%-90% of cases). It is yeast which live in small amounts in our mouth and belly or on skin. Candidiasis is a disease of skin, mucosa and also affects internal organs.
Thrush (Oropharyngal candidiasis)
Type of candidiasis when the yeast spreads to mouth and throat can cause an infection known as thrush. This infection can affect mostly newborns, old age groups and persons with weak immune system. And also can infect adults who are being treated with cancer, taking medications like corticosteroids and broad-spectrum anti-toxins and also infect diabetic patients [3].
Symptoms
• White or yellow patches on tongue, lips, gums and in inner
cheeks
• Rush in mouth and in throat
• Mouth cracking on corners
• Pain during swallowing (if spreads to throat)
Treatment
Thrush can be treated with antifungal medicines like clotrimazol, fluconazole, itraconazole and amphoteric B and washing of mouth with Chlrohexidine (CXN) can prevent the infection in persons with weak immune system (Figure 1).
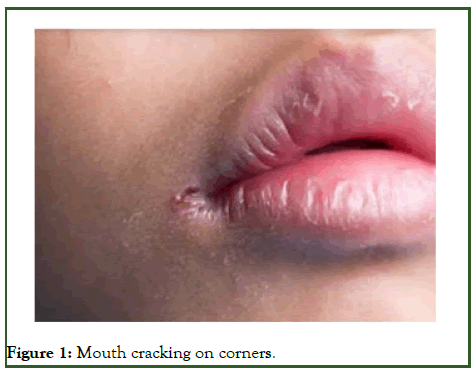
Figure 1: Mouth cracking on corners.
Genital yeast infection (genital candidiasis)
These are the Candida species that can cause infection in the genital tract of women the vagina and in men the penis will be affected with this infection. This happens when too much yeast grows in vagina and is more common in women’s as compared to men.
This occurs typically when the vaginal balance changes, which is caused by pregnancy, diabetes and due to use of spermicides.
Symptoms
• Vaginal itching
• Pain and burning during urination
• Pain during sexual intercourse
• Swelling of vagina and vulva
• A man with this infection has a itching on his penis
Treatment
The antifungal tablet or cream will cure the infection. Fluconazole an antifungal medicine can be prescribed [4].
Invasive candidiasis
This type of infection is caused when the yeast spreads to bloodstream by medical equipment’s or devices. This infection affects heart, brain, blood, eyes and also bones. The risk factors are weak immune system, kidney failure and use of antibiotics.
Symptoms
The symptoms of this infection include chills and fever. The infection can be treated with the use of antifungal medicines.
Laboratory diagnosis
Specimen: Urine in case of Urinary Tract Infection (UTI). Vaginal discharge in case of genital infection. Cerebrospinal fluid in case of Central Nervous System (CNS) infections.
Direct microscopy: Gram staining and potassium hydroxide (KOH) mounts shows gram positive yeast cell under microscope. Colonization is detected by demonstration of pseudohyphae [5].
Culture: Candida species can grow on Sabouard Dextrose Agar (SDA) media very well and also in ordinary bacteriological media like blood agar. The optimum temperature is 25°C-37°C. Creamy and pasty colonies will appear after 24 hours of incubation (Figures 2 and 3).

Figure 2: Candida albicans in gram staining.

Figure 3: Pseudohyphae of Candida albicans.
Aspergillosis
The Aspergillosis is caused by a mold (fungus) which is present everywhere. The Aspergillus fumigatus is the main causative pathogen. The fungus mainly affects respiratory tract.
The Aspergillosis is caused by the inhalation of Aspergillus conida or Mycelial fragments present in soil, in decaying matter. This fungus can cause three types of diseases:
Allergic reaction
Some persons with asthma can develop such type of reactions on exposure to aspergillus mold. These individuals develop a disease known as allergic bronchopulmonary Aspergillosis.
Treatment
These allergic reactions can be treated by oral corticosteroids to prevent the existing asthma or cystic fibrosis.
Symptoms
• Fever
• Cough with blood
Aspergilloma
This is a chronic lung disease in which fungus (Aspergillus) colonizes in pulmonary cavities and grows into a tangled mass known as aspergillomas. Also known as fungus ball [6].
Treatment: The aspergillomas cannot be treated with antifungal medicines, so by surgery the fungal mass is removed (Figure 4).

Figure 4: Fungus ball.
Symptoms
• Cough with blood (hemoptysis)
• Wheezing
• Difficulty in breathing
• Weight loss
• Fatigue
Invasive Aspergillosis
This is the most severe Aspergillosis and can spread to brain, heart and kidneys and also infects skin. Invasive Aspergillosis occurs in persons with weak immune system due to cancer chemotherapy, bone marrow transplantation. The untreated Aspergillosis can cause death.
Treatment
The invasive Aspergillosis can be treated with antifungal medicines like vericonazole, amphoteric B.
Symptoms
• Fever and chills
• Coughing with blood
• Chest pain
• Headache
• Skin lesions
Laboratory diagnosis
Specimen:
• Sputum (in case of respiratory infection)
• Biopsy
• Bronchoalveolar washing
Imaging test: A chest X-ray is done which produces the detailed images of the fungal mass in case of Aspergillomas infection.
Respiratory secretion (sputum) test: The sputum sample is stained and is checked under microscope for the presence of Aspergillus filaments. If the fungus is seen than the sample is cultured to confirm the diagnosis [7].
Biopsy: In case of invasive Aspergillosis the tissue from the infected lungs is examined under microscope to confirm the diagnosis (Figures 5 and 6).

Figure 5: A chest X-ray is done which produces the detailed images of the fungal mass in case of aspergillomas infection.

Figure 6: The sputum sample is stained and is checked under microscope for the presence of Aspergillus filaments.
Mucormycosis
Mucormycosis (previously called zygomycosis) is caused by Mucor, Rhizopus and Licheimia. These fungi are saprophytes of soil and decaying vegetables. The Mucormycosis are life threatening infections and the risk factors include diabetes, neutropenia and ketoacidosis. These fungus mainly affects the upper respiratory system, digestive tract, brain and also keratin tissue.
Symptoms: The symptoms depend on the type of Mucormycosis disease.
Rhino cerebral mucormycosis: The symptoms include fever, headache, reddish skin over nose, swelling of eyes, sinuses.
Pulmonary mucormycosis: Symptoms include coughing with blood, fever, difficulty during breathing [8].
GI mucormycosis: Symptoms include abdominal pain, vomiting with blood.
Cutaneous mucormycosis: Symptoms include reddish and swollen skin initially and later it becomes an ulcer with dark centre and sharp edges (Figure 7).

Figure 7: Cutaneous mucormycosis.
Results and Discussion
Laboratory diagnosis
Specimen:
• Scraping from the site of infection
• Nasal exudates
• Pus and sputum
Direct microscopy: KOH (Potassium hydroxide) mounts of samples shows non-septate hyphae. Tissues are stained with H and E stain and then seen under microscope for the demonstration of hyphae.
Culture: The samples can be cultured on Sabouard Dextrose Agar (SDA) media after that the colonies are identified. Lactophenol Cotton Blue (LCB) preparations show branched sporangiophores along aerial mycelium.
Treatment: The mucormycosis can treat by antifungal medicines such as amphoteric B, posaconazole and isavuconazole are given through vein to the patient with mucormycosis. These medicines are effective against this fungal disease.
Penicillosis
This fungal infection is caused by dimorphic fungi known as Penicillium rnarneffei. It is more common is persons which have the history of HIV (Human-Immunodeficiency-Virus) infection.
This fungal infection is endemic in southeast Asia and also in southern parts of China. The Penicillium marneffei is a saprophytic fungus and can cause penicillosis, keratitis, otomycosis and deep infections [9].
Previously this infection was named as talaromycosis and the causative fungus was called Talaromyces marneffei. But know a day it is called penicillosis and the fungus is known as Penicillium marneffei.
Symptoms:
• Bumps on skin, face and also in neck
• Fever
• Cough
• Enlargement of liver and spleen
• Abdominal pain and diarrhea
• Shortness of breathing
Laboratory diagnosis
Direct microscopy: The samples from different infected body parts are collected such as skin, bone marrow, lung or lymph node are cultured in laboratory in suitable media and the growth of septate hyphae of fungus is seen under microscope by making the smears.
Culture: The fungus can grow on Sabouard Dextrose Media (SDA) media and give the white colour colonies and later the colonies become powdery and blue in colour.
Treatment: The penicillosis can be treated by antifungal medicines such as amphoteric B, itraconazole, vericonazole and terbinafine. These medicines are seen effective against this infection [10].
Conclusion
The fungal infections are life threatening complications to every individual who is being infected. So the best approach to avoid these life threatening infections is the early detection of the causative agents, after the signs and symptoms are being identified. So that the appropriate treatment can be given as soon as possible.
Clinicians should be familiar about all the diagnostic methods and they have to use the suitable antifungal agents, because they can impact the largest outcome of patients. After the localized fungal infection the appropriate antifungal medicines should be advised by every physician.
References
- Mora C, Tittensor DP, Adl S, Simpson AG, Worm B. How many species are there on earth and in the ocean? PLoS Biol. 2011;9(8):e1001127.
[Crossref] [Google Scholar] [PubMed]
- Brown GD, Denning DW, Levitz SM. Tackling human fungal infections. Science. 2012;336(6082):647.
[Crossref] [Google Scholar] [PubMed]
- Muszewska A, Pawłowska J, Krzysciak P. Biology, systematics and clinical manifestations of zygomycota infections. Eur J Clin Microbiol Infect Dis. 2014;33:1273-1287.
[Crossref] [Google Scholar] [PubMed]
- Badiee P, Alborzi A, Farhoudi F. A case of Candida mediastinitis after dental extraction. J Infect Dev Ctries. 2011;5(01):075-078.
[Crossref] [Google Scholar] [PubMed]
- Buchacz K, Lau B, Jing Y, Bosch R, Abraham AG, Gill MJ, et al. Incidence of AIDS-defining opportunistic infections in a multicohort analysis of HIV-infected persons in the United States and Canada, 2000-2010. J Infect Dis. 2016;214(6):862-872.
[Crossref] [Google Scholar] [PubMed]
- Kontoyiannis DP, Lionakis MS, Lewis RE, Chamilos G, Healy M, Perego C, et al. Zygomycosis in a tertiary-care cancer center in the era of Aspergillus-active antifungal therapy: A case-control observational study of 27 recent cases. J Infect Dis. 2005;191(8):1350-1360.
[Crossref] [Google Scholar] [PubMed]
- Kradin RL, Mark EJ. The pathology of pulmonary disorders due to Aspergillus spp. Arch Pathol Lab Med. 2008;132(4):606-614.
[Crossref] [Google Scholar] [PubMed]
- Dhurat R, Kothavade RJ, Kumar A. A first-line antiretroviral therapy-resistant HIV patient with rhinoentomophthoromycosis. Indian J Med Microbiol. 2018;36(1):136-139.
[Crossref] [Google Scholar] [PubMed]
- Vanittanakom N, Cooper Jr CR, Fisher MC, Sirisanthana T. Penicillium marneffei infection and recent advances in the epidemiology and molecular biology aspects. Clin Microbiol Rev. 2006;19(1):95-110.
[Crossref] [Google Scholar] [PubMed]
- Martson AG, Alffenaar JW, Bruggemann RJ, Hope W. Precision therapy for invasive fungal diseases. J Fungi. 2021;8(1):18.
[Crossref] [Google Scholar] [PubMed]
Citation: Bashir S, Sofi A, Hanan, Bharti J (2024) Opportunistic Invasive Fungal Infections. Clin Microbiol. 13:399.
Copyright: © 2024 Bashir S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
