Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
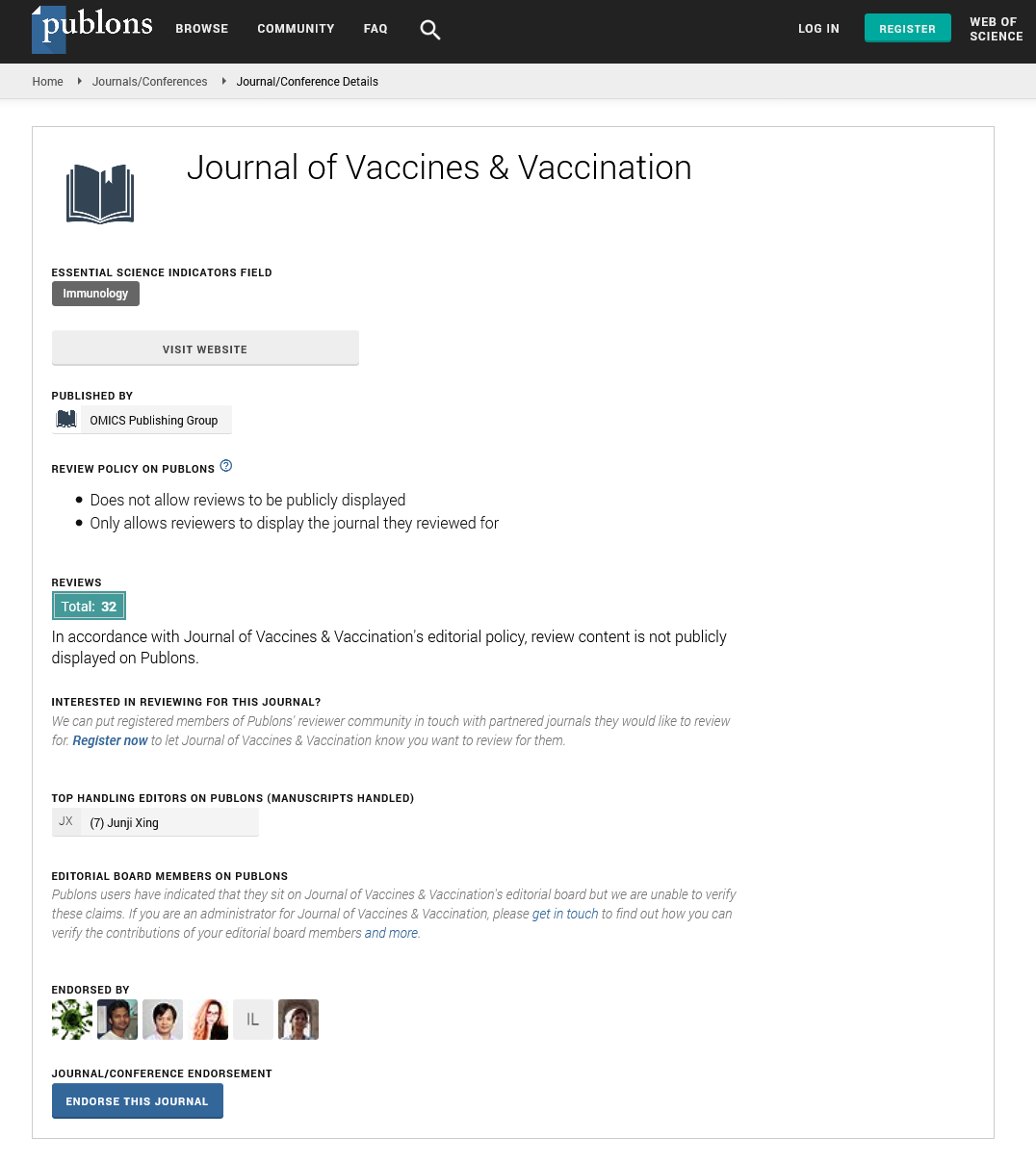
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2021) Volume 12, Issue 2
New Strategies for COVID-19 Vaccination and Adjuvant Prophylaxis
Aziz Rodan Sarohan*Received: 15-Feb-2021 Published: 08-Mar-2021, DOI: 10.35248/2157-7560.21.12.449
Abstract
Although more than a year has passed since the outbreak of the COVID-19 pandemic, the pathogenesis of the disease has not yet been clarified. For this reason, no significant improvement has been achieved regarding the treatment of the disease. The way to develop effective vaccines and drugs against COVID-19 is also through a clear understanding of the pathogenesis. The very frequent mutating nature of SARS-CoV-2 and the emergence of new variants have raised concerns that vaccines against COVID-19 may not work. In the defense mechanism of COVID-19, retinol and retinoic acids are used in the synthesis of Type I interferon and suppression of inflammation. However, due to the extremely large viral genome in COVID-19, retinol is used too much and is consumed quickly. Due to the retinoid signaling defect that develops, as a result, both Type I interferon synthesis is interrupted and the inflammation process gets out of control by exacerbating. In COVID-19, since low retinol causes suppression of the immune system, sufficient antibody titer cannot develop in the host during primary infection. Therefore, reinfections can be seen in COVID-19. Low retinol may also be the cause of inadequate antibody responses to vaccines. Another possible cause of reinfections is the frequent mutation of SARS-CoV-2 and the emergence of new SARS-CoV-2 variants. Some COVID-19 vaccines against these new variants were found to be unable to generate sufficient antibody titer. This shows that revising existing COVID-19 vaccines may not be enough against COVID-19. All these developments show that different vaccine and adjuvant applications are needed to cope with COVID-19. For this purpose, strengthening existing vaccines with adjuvants, combined and pure adjuvant vaccine applications, through the community's vitamin A screening by giving vitamin A supplements to those with vitamin A deficiency such as enhancing the vaccine response prophylactic adjuvant applications should be brought to the agenda and discussed in scientific circles.Keywords
COVID-19; Adjuvant; Vaccines; Vaccination; COVID-19 vaccines; Retinol
Introduction
COVID-19, whose agent is SARS-CoV-2, was declared as a pandemic by the World Health Organization (WHO) in March 2020. In this epidemic, more than two million people died and more than 100 million people were infected [1,2]. As of the beginning of 2021, when this review was written, NIH (American Health Institute) president Dr. Anthony Fauci declared that COVID-19 is now out of control. Similar statements came simultaneously from the World Health Organization. No specific treatment has so far been found against COVID-19, which causes severe socioeconomic problems and significant loss of life. And this epidemic, unfortunately, continues to exist as an important problem all over the world [3].
Many vaccines have been developed against COVID-19 at an unprecedented speed in history, in the span of a year or so. These vaccines were started to be administered at the same speed after passing the approval of regulatory centers [4]. However, because of the frequent mutation of SARS-CoV-2 and the emergence of new variants of the virus, it has raised concerns that vaccines developed against COVID-19 may not work [5].
This possibility, which at first seemed a prophecy, is, unfortunately, a fact with a high probability of realization. Another important problem with vaccines is the production capacity. Considering that billions of people will be vaccinated, it seems impossible for only 2-3 companies to meet this need. In addition to the vaccine supply problem, problems with logistical support have already started to occur. However, the biggest concern with vaccines is the fear and possibility that vaccines may not be effective against SARS-CoV-2 [6].
In order to control COVID-19, the biggest epidemic of modern times, the development of vaccines against COVID-19 continues at full speed all over the world. Some of the vaccines that have passed the accelerated phase phases are already in current use [5]. However, some question marks and concerns about the effectiveness and reliability of these vaccines against COVID-19 have existed since the beginning of the pandemic [6]. The long-term results of these vaccines are unknown, the very frequent mutation of SARS-CoV-2 and the emergence of new SARS-CoV- 2 variants, and the ineffectiveness of some vaccines against these new variants are the main sources of these concerns [6]. Unfortunately, we have no choice but to wait and see the long-term results of these vaccines, which are developed and produced very quickly.
As of now, five vaccine projects have come to the fore on a global scale. These; Prizer-BioNTech (Germany), Oxford Uni- Astra Zeneca (British), Moderna (USA), Sinovac (China), and Gamaleya-SputnicV (Russia) are vaccine projects. Some of these vaccines, whose 4 phase studies were completed and licensed from regulation centers, were started to be administered to humans [4,5]. Even if they have been able to create an antibody response against SARS-CoV-2 and have successfully passed the clinical phases, it is uncertain how long and effectively these vaccines will protect people against COVID-19 in the long term [6]. Some of these licensed vaccines have taken their place in the field, on the other hand, phase studies of dozens of vaccine projects are continuing at full speed. The uncertainty of whether these vaccines will continue to protect against SARS-CoV-2 (COVID-19) due to the mutations and newly emerged SARS-CoV- 2 variants has led to the growing concerns about the reliability of these vaccines [6].
Therefore, researches on the pathogenesis of COVID-19 and drug treatment of COVID-19 continue to be important [7]. While this enigma of COVID-19 pathogenesis and vaccines in the middle, drug development and drug repositioning options for COVID-19 treatment is progressing mediocre. Unfortunately, drug studies and other therapeutic options have fallen into the background in this process [7]. The idea of repositioning existing drugs against COVID-19 was highly sought after by scientific circles at the beginning of the pandemic [8]. However, due to the long duration of drug development and the predominance of the idea that the best way to cope with the epidemic is through vaccine development and vaccination of the society, vaccine development studies have come to the front. Another reason for the idea of vaccine development to come to the fore may be that vaccines allow for rapid commercialization [8].
Literature Review
COVID-19 pathogenesis, retinol depletion and retinoid signaling disorder
Unfortunately, the pathogenesis of COVID-19 remains a mystery despite all the research carried out in the period of about a year when the COVID-19 pandemic started [6,9]. However, as a result of the studies conducted by us, it has been determined that retinol is consumed excessively during host defense in COVID-19 and serum retinol levels are low in severe COVID-19 patients. In our recently concluded clinical study, which was published in medRxiv as preprint printing, it was found that serum retinol levels were significantly lower in severe COVID-19 patients compared to the control group [10]. Likewise, the basic condition of developing effective vaccines and drugs depends on a clear understanding and knowledge of how the virus affects the immune system [9].
Pathogenesis and tissue damage in viral infections usually occur in certain tissues and organs related to the cell and tissue tropism of the virus, and tissue damage and loss of function in the host are also limited to these cell and tissue systems [11]. Even, viruses are sometimes classified according to their affinity (tropism) to tissues and cells. Like neurotrophic, enterotropic, hepatotropic viruses. During the 11 pandemic period, most researchers lost time in pursuit of this viral tropism mechanism to solve the pathogenesis of COVID-19. This search remains a major obstacle to understanding the pathogenesis of COVID-19 even today.
COVID-19 also has a cell and tissue tropism through the ACE2 and TMPRSS2 receptors and is limited to a few organ involvements. This tropism is mainly associated with the respiratory and gastrointestinal tract involvement of SARS-CoV- 2. But, unlike other viral infections, in COVID-19, widespread organ involvement and devastating systemic effects that cannot be explained by cell and tissue tropism occur [12,13]. It is understood that this systemic involvement in COVID-19, which is quite severe and destructive, is caused by retinol depletion and retinoid signaling disorder. The intense and widespread activity of retinoid signaling in the body is interrupted by retinol depletion, causing such a picture and destructive consequences.
However, what makes the main difference in the pathogenesis of COVID-19 is the excessive size of the SARS-CoV-2 genome and the retinol depletion and retinoid signaling impairment caused by it. The genome size of other RNA viruses is 8-10 kB, while the genome size of SARS-CoV-2 is about 30 kB, and SARS-CoV- 2 is the virus with the largest genome among RNA viruses [14,15]. Because of this genome size, large amounts of viral RNA particles are released from viruses that are broken down by immune system cells during infection. Because of these scattered RNA ends, RIG-I and TLR receptors are overstimulated, consuming retinoic acids. Retinoic acids are used herein for Type I interferon synthesis via the RIG-I and TLR pathways [16,17]. In COVID-19, due to retinol depletion and retinoid signal disruption, Type interferon synthesis is interrupted and inflammatory processes are triggered. In COVID-19, due to the depletion of retinoic acids, the pressure on inflammatory mechanisms is removed and excessive inflammatory cytokine release and destructive systemic effects occur [18].
The weak antibody response caused by retinoid signal impairment also seems to be responsible for recurrent infections in COVID-19. During active infection in COVID-19, effective and permanent antibody response cannot occur due to decreased retinol levels due to excessive use in the Type I interferon synthesis pathway and retinoid signaling disorder. Vitamin A deficiency causes both susceptibilities to infection and the development of severe disease in COVID-19. Low vitamin A reserves cause early termination of Type I interferon synthesis and concurrently excessive inflammatory response. Excessive use and consumption of retinol during the clinical course of COVID-19 cause immune system suppression and TYPE I interferon synthesis defect, preventing the development of adequate antibody response against SARS-CoV-2 in the host [19,20].
Type I interferon synthesis defect in COVID-19 is the most important reason for the weak antibody response to SARS-CoV- 2 [16,19,21-23]. In a study conducted during previous SARS outbreaks, it was determined that SARS-CoV (SARS-CoV- 1) weakens host defense by inhibiting Type I interferon synthesis. However, interferon synthesis is blocked by a different mechanism here. Here, the N protein of the viral nucleocapsid binds to TRIM25 (Triple Motif Protein 25), which activates the RIG-I pathway. In this way, it blocks RIG-I activation and interferon synthesis [24]. As can be understood from here, Type I interferon synthesis blockage in viral pathogenesis has been investigated during other Coronavirus infections. However, the retinoid signaling defect was not investigated in these studies, and this issue was not raised at that time. Retinoid signaling defect in viral pathogenesis is brought to the agenda of the scientific world for the first time with the studies carried out by us [10,19].
Due to retinol depletion and retinoid signaling defect, Type I interferon synthesis defect and changes in immune system cells result in weakening of the host immune system and therefore the infection persists in some patients. Some patients with the out-patient disease remain viral for a long time and continue to spread the disease. Some patients also return to the hospital with a relapse of the disease after discharge. In addition to this persistence and recurrence, some patients experience reinfections after the recovery period. This suggests that stimulation of an immune response that eliminates the virus is difficult in some patients and vaccines may not work in this group of patients. These scenarios should be taken into account when determining vaccine development strategies. Additionally, there are many types or subtypes of coronavirus. Therefore, it will be difficult to develop vaccines that directly target SARS-CoV- 2 [25].
These patients recovered from the non-severe stage can be followed in terms of immunity with their T / B cell responses, but these patients can be given retinol supplements to support their immune system, clear the virus from the body and develop an adequate antibody response. All these reasons make vitamin A an important option for prophylaxis, treatment, and adjuvant applications in COVID-19. Having full vitamin A reserves before infection will provide mild and sequel-free recovery of COVID-19, as well as providing adequate antibody synthesis and permanent immune development, and prevent persistence, relapse, and re-infections.
SARS-CoV-2 mutations and new SARS-CoV-2 variants among other factors that can be effective in the development of reinfection, constantly occupy the world agenda and it continues to rank high in media news [26]. SARS-CoV-2 mutations and new variants deserve enough detail and importance to be discussed in another study. Therefore, mutations and new variants of SARS-CoV-2 were evaluated in terms of their interactions with current COVID-19 vaccines. In addition, these mutations and variants are briefly discussed here to provide a perspective for future vaccine and other treatment applications.
What do SARS-CoV-2 mutations and new SARS-CoV-2 variants tell us?
For the first time in the pandemic, the D614G mutation of SARS-CoV-2 was much talked about and discussed. The detection of a mutagenic strain of SARS-CoV-2 that disrupts binding to three types of antibodies in Bisons and the destruction of tens of thousands of Bison in Denmark and the Netherlands reminded epidemics in medieval Europe, which caused fear and anxiety in humans [27]. The detail in these mutations suggested that the vaccines currently being developed could fail [28]. Because the mutation here was in the receptorbinding area of the SARS-CoV-2 spike protein, to which the antibodies targeted to be developed in the host with vaccines will also bind, and it was a change that would disrupt the antibody binding for the vaccines being prepared. For him, this mutation was perceived as a serious threat to the COVID-19 vaccines under development [29].
Subsequent reports of mutations and new variants have deepened doubts about the effectiveness of vaccines. In the study carried out by the researchers at the Fred Hutchinson Institute, some mutations were detected in the parts of the host that are related to the structure of the SARS-CoV-2 Spike protein that binds to the ACE2 receptor, again disrupting the antibody binding [30,31]. It has been announced that the effectiveness of vaccines developed against the SARS-CoV-2 spike protein may decrease as a result of these mutations. These results declared that these vaccines prepared against the SARS-CoV- 2 spike protein could go to waste. Subsequently, update recommendations on vaccines began to be made [31].
Later, a new variant of SARS-CoV-2 was detected in genetic screening studies conducted by the COVID-19 Genomics UK (COG-UK) consortium in England [32]. This new variant, named "VUI-202012/01", which was first seen in Europe, but later appeared in America, Africa, and India, turned out to be much more contagious [32]. It was shared with the public that this variant is 70% more contagious. However, no data were shared regarding its pathogenicity and virulence [33]. Unfortunately, the emergence of new SARS-CoV-2 variants has further fueled concerns about vaccines. After these developments, updated suggestions on COVID-19 vaccines started to be made more frequently by some circles. Afterward, it was announced that the revision studies of the mRNA-based vaccine, which is being prepared against the new SARS-CoV-2 variants from the BioNTech-Pfizer joint venture [34].
Recent vaccination studies in South Africa found that COVID-19 vaccines by Johnson & Johnson and Novavax provided poor protection against the B.1.351 (501.V2) variant responsible for the majority of SARS-CoV-2 infections in South Africa [35-38]. The effectiveness of these vaccines against mild disease was 57% for J&J and 49% for Novavax (lower than in other countries where they were tested). In the meantime, data that the Astra Zeneca-Oxford vaccine prepared for COVID-19 did not provide adequate protection against the B.1.351 variant in South Africa was shared with the public [39]. All these developments have raised concerns about the effectiveness of the vaccines on mutagenic forms and new SARS-CoV-2 variants, and the Astra Zeneca vaccine project in South Africa was halted. Most recently, WHO has urged vaccine manufacturers to consider mutations and new SARS-CoV-2 variants. These developments have raised concerns about the effectiveness of vaccines and strengthened the hand of organized anti-vaccine social movements in Europe and America. These organized social structures also stand before us as another problem that can undermine the immunization process [40].
The Human Immunodeficiency Virus (HIV), which emerged in West Africa in the early 20th century, could not be detected in humans until the early 80s. The disease continued to spread insidiously for a long time, and the HIV virus was only noticed in the 1980s after it was recognized as an epidemic among gay men in the United States, causing AIDS [41]. Shortly after the HIV virus was identified in 1983, US Health and Human Services Secretary Margaret Heckler claimed that an effective vaccine against HIV would be developed within two years. However, despite the past 40 years, an effective vaccine against HIV has not been developed yet [41,42]. The frequently mutating nature of HIV, which many epidemiologists consider as an active pandemic, and its immune system targeting have made things extremely complicated [42,43].
On the other hand, AIDS, thanks to the drugs developed with the possibilities of modern medicine, has become a manageable and treatable disease, rather than being a death sentence for patients [42,43]. Due to frequent mutations, a new type of vaccine is developed every year against influenza virus Likewise, a seasonal polyvalent influenza vaccine is prepared every year for influenza outbreaks, using antigens belonging to four different influenza strains consisting of Influenza A and Influenza B serotypes. However, the effectiveness of these vaccines is low [44]. Likewise, due to the frequent mutations in SARS-CoV-2 and the emergence of a new SARS-CoV-2 variant, it is not a distant possibility that we will experience a fate similar to HIV and Influenza in COVID-19 in terms of vaccine studies.
New strategies and adjuvant prophylaxis in COVID-19 vaccination
The World Health Organization added vitamin A to its prevention programs during the measles epidemic in the 1950s and achieved successful results. Vitamin A reduced mortality from measles pneumonia by 50% in epidemics. However, a very heavy price was paid in the process until the measles vaccine was developed [45-47]. Impressive results have also been obtained from supportive therapies with vitamin A in AIDS patients [48]. In addition, vitamin A and its derivatives are currently used as vaccine adjuvants [49,50]. It has been determined in many previous studies that vitamin A deficiency reduces host resistance against viral infections and vitamin A levels decrease during viral infections [51,52].
Retinol levels decrease severely in COVID-19, which causes a severe infectious picture and systemic organ damage [19]. Retinol depletion and the resulting retinoid signal impairment in COVID-19 appear to be responsible for poor antibody responses after infection, particularly the Type I interferon synthesis defect and the devastating systemic inflammatory effects of the adaptive immune system. Weak antibody responses to vaccines may also be due to retinol depletion.
Likewise, in measles, as in COVID-19, people died due to a severe pneumonia picture, and COVID-19 is a devastating infection for vitamin A metabolism, like Measles [46,47]. It is also noteworthy that an adult with severe measles-induced pneumonia recovered rapidly with high doses of corticosteroids and vitamin A [53]. For COVID-19, we need to take advantage of vitamin A for both prophylactic, treatment, and adjuvant applications. In this context, it is just an intellectual irony that we do not benefit from the experiences gained with vitamin A during measles epidemics.
Vitamin A deficiency is associated with immune system failure. It has been well established that vitamin A deficiency is a dietary acquired immune deficiency disease characterized by widespread immune depression and increased infectious disease morbidity and mortality [54,55]. In addition, it has been found that vitamin A levels decrease and immune system suppression develops during the course of some infections such as HIV, RSV, and Measles. In humans, most understanding of vitamin A-related immunodeficiency has come from studies involving children rather than adults. Post-mortem autopsy studies in children found that vitamin A deficiency is associated with atrophy of the thymus, lymph nodes, and spleen [56,57].
In vitamin, a deficiency, disruption in the mucosal barriers in the gastrointestinal system and respiratory system, weakening in monocyte, macrophage, and natural killer functions, decrease in the number of T helper and B lymphocyte cells, and impairment in their functions. Disruption of T and B cell functions causes immune system suppression and impairment in antibody responses. Vitamin A plays an important role in lymphopoiesis. With vitamin A supplements, an increase in total lymphocyte count, CD4 T cells, and NK cells can be achieved [51,52,54,58]. Studies in HIV-infected adults have found a fairly consistent association between low vitamin A levels and low CD4 counts. Carotenoid supplementation increased CD4 T cell count in adults with HIV [59]. In children with AIDS, high-dose vitamin A supplementation increased circulating CD4 T cells and NK cells [60].
In vitamin, a deficiency, depression, and dysregulation in the immune system are clearly seen in both AIDS patients and COVID-19 patients. Likewise, the immune system changes were seen in COVID-19; unfortunately, resemble the immune system suppression seen in vitamin A deficiency dramatically [61-63]. The harsh inflammatory response of the adaptive immune system in COVID-19 should not lead to a false belief that the immune system is strong and healthy. Likewise, in severe COVID-19 patients, the innate component of the immune system, which provides Type I interferon synthesis and is mainly responsible for the primary host defense, has collapsed [64,65]. In severe COVID-19, as with vitamin A deficiency, leukocytes, especially neutrophils, are increased [66]. In addition, COVID-19 has a reduction in total lymphocyte count, CD4+T cells, CD8+T cells, regulatory T cells, natural killer cells, B lymphocytes, plasma cells, B and T memory cells, and dendritic cells [67-69].
Vitamin A and its derivatives, provide their main protective effects against viral infections with the synthesis of Type I interferon (IFNα and IFNβ) beyond the mucosal immunity and mechanical protection they provide by secretory IgA activity and mucosal barrier formation [70]. Type I interferon’s are the strongest endogenous antiviral mediators in host defense and provide the clearance of the virus from the body and the development of a permanent immune response with antibody synthesis [71,72]. Type I interferon is synthesized mainly in RIGI and TLR3 pathways through nuclear retinoic acid receptors and transcription factors, in a retinoic acid-dependent manner [73-75]. Type I interferon synthesis is at the forefront especially in plasmocidic dendritic cells in the lungs where atRA synthesis also takes place [76].
The main strength of vitamin A and its active derivatives, retinoic acids, in host defense comes from their effects on Type I interferon synthesis. Type I interferon is required for a robust immune defense, immune system regulation, and effective antibody responses [77,78]. Unfortunately, adequate and effective antibody response does not develop due to retinol depletion in COVID-19 and Type I interferon synthesis defect caused by retinoid signaling impairment [79]. In COVID-19, the inadequate antibody response is the cause of weak immune response and reinfections. The main reason for this is the decreased retinol levels and retinoid signaling disorder in COVID-19. The reasons for insufficient antibody response to COVID-19 vaccines are immune system depression and Type I interferon synthesis defect due to low retinol and retinoid signaling disorder.
Vitamin A deficiency leads to immune depression and immune dysfunction by weakening antibody responses primarily with the insufficient activity of IFNα and IFNβ, over activity of inflammatory cytokines such as IFNγ, and activity impairment in dendritic cells of the adaptive immune system [58,63,77]. In COVID-19, the impairment in the number and functions of T and B cells impairs both cellular and humoral immunity. The decrease in T lymphocyte, B lymphocyte, and memory cells also weaken antibody synthesis and the antibody-mediated defense system [51,80]. Retinoic acids are essential for antibody production and normal activity of B lymphocytes while providing CD8+T lymphocyte survival, proliferation, and activity. Therefore, vitamin A deficiency also impairs vaccination responses [51,81]. Relatedly, in a study of children with vitamin A deficiency in Indonesia, children who received vitamin A supplements had higher antibody responses after tetanus vaccination than children who did not receive vitamin A supplements [82].
While hot discussions continue about the effectiveness of vaccines in COVID-19, it is worth mentioning the adjuvant role of vitamin A from the COVID-19 perspective [83]. Although SARS-CoV-2, creates an extreme inflammatory reaction, it is a fact that it targets the immune system and especially collapses the innate component of the immune system [84]. While it is evident that vitamin A levels decrease during COVID-19 and the vaccine responses are weakened, vitamin A and its derivatives are a boon for adjuvant applications in COVID-19. In addition, retinol screening with ongoing vaccination programs and vaccination with vitamin A supplements to individuals with vitamin A deficiency will increase the response and effectiveness of vaccines against COVID-19. We can call this prophylactic adjuvant administration or adjuvant prophylaxis.
Another adjuvant administration option for strong RIG-I stimulation and efficient Type I interferon synthesis in the host is RIG-I agonists. The RIG-I pathway initiates antiviral programs, i.e Type I interferon synthesis, in RNA virus infections that restrict virus infection and activate many cell types, including dendritic cells and macrophages for antigen presentation and cytokine production [85]. RIG-I agonists can be a good option to strengthen the congenital immune component that is weakened in COVID-19. Likewise, retinol and retinoic acids will be required for RIG-I synthesis and activity. As the name suggests, RIG-I synthesis and activity are provided by retinoic acids. RIG-I synthesis is provided by the activation of transcription factors by retinoic acids. Therefore, RIG-I agonists will not work without sufficient Retinoic Acid (atRA).
The frequent mutation of SARS-CoV-2 and the emergence of new SARS-CoV-2 variants also bring to mind combined vaccine adaptations. One of these options is to prepare new polyvalent COVID-19 vaccines using antigens belonging to many SARS-CoV- 2 variants, as in seasonal influenza vaccines [86]. With a vaccine to be prepared in this way, protection against more than one SARS-CoV-2 variant can be provided. It is also conceivable to augment such a vaccine with retinol. With the COVID-19 pandemic, new technology vaccines such as mRNA, DNA, and vector vaccines have entered our lives in addition to the classic inactivated vaccines. However, the fact that these vaccines are very new and the lack of experience with them, the protection of these vaccines, and especially the side effects will keep our minds busy for a while.
All these data show that retinol and retinoic acids are essentially involved in the regulation of immune defense. It is seen that vitamin A and its derivatives are indispensable in all stages of the immune defense process, from the identification of cells (differentiation) to antibody synthesis and even the formation of immune memory. Retinol and retinoid signaling appear to be absolutely necessary both for the regulation and activity of the innate defense of the host and for optimal benefit from vaccines. Unfortunately, vaccines will not work unless retinol reserves are filled in the host and retinoid signaling disorder in COVID-19 is eliminated. A robust and effective vaccination program can only be carried out thanks to a properly functioning immune defense system with adequate retinol reserve and healthy retinoid metabolism. The success of this application in COVID-19 will also enable us to cope with other infections that collapse the immune system, especially HIV.
Conclusion
We wake up almost every day with the news of a new mutation and a new SARS-CoV-2 variant. Moreover, new data emerging that the effectiveness of current COVID-19 vaccines is weak against new variants revealed the need for new and different searches for COVID-19 vaccines and treatment approaches. In this context, updating of existing vaccines has been widely discussed. However, scientific circles have not talked about the enrichment of vaccines with adjuvant compounds, pure adjuvant vaccine applications, and adjuvant prophylactic applications. In this chaotic pandemic period, it is vital to take advantage of the proven adjuvant effectiveness of vitamin A and atRA for COVID-19.
Since it is clear that COVID-19 is destructive for vitamin A metabolism and causes serious clinical pictures and re-infections with this mechanism, protective and therapeutic options regarding vitamin A should be evaluated at the highest level. Likewise, vitamin A and its derivatives are already used with many vaccines as adjuvant compounds to increase antibody responses. In this context, based on the fact that COVID-19 is destructive for vitamin A metabolism, adjuvant vaccines and adjuvant prophylactic applications should be considered for COVID-19. Therefore, including the revision of existing vaccines, adjuvant-boosted vaccines, pure adjuvant vaccines, and prophylactic adjuvant applications should be considered again and again from a different perspective and especially for COVID-19.
The success of current COVID-19 vaccines against SARS-CoV-2 has not yet been clarified. Therefore, attention should be paid to the researches to be carried out for the treatment of COVID-19 with medication. We need to make the most of the adjuvant modifications of vitamin A and therapeutic drug development efforts to deal with COVID-19 as well as similar outbreaks that may occur in the coming years. For all these reasons, vitamin A anti-infectious, anti-inflammatory, immunomodulatory, and proven adjuvant efficacy are should not be ignored. Today, vitamin A's immune system enhancing effect seems to be underestimated or forgotten. With this COVID-19 pandemic, it is time to rediscover vitamin A again and again. In this context, we should consider the COVID-19 outbreak as a phenomenon that we have gained experience to combat epidemics that may occur in the coming years.
REFERENCES
- World Health Organization. Novel Coronavirus Situation Report-Weekly Epidemiological Update.2020.
- Punlons. The socio-economic impact of COVID-19 in fragile settings: Peace and social cohesion at risk.2020.
- Lai CC, Wang CY, Wang YH, Hsueh SC, Ko WC, Hsueh PR. Global epidemiology of coronavirus disease 2019 (COVID-19): Disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int J Antimicrob Agents. 2020;55(4):105946.
- International Labor Organisation.COVID-19 Vaccines within WHO EUL/PQ evaluation process. Status of COVID-19 Vaccines within WHO EUL/PQ evaluation process. 2020.
- International Labor Organisation. Status of COVID-19 Vaccines within WHO EUL/PQ evaluation process. 2020.
- BBC News. Is the Covid vaccine safe? By Michelle Roberts. Health Editor,2020.
- Zhou B, Kojima S, Kawamoto A, Fukushima M. COVID‐19 pathogenesis, prognostic factors and treatment strategy: urgent recommendations. J Med Virol. 2020.
- Wu C, Liu Y, Yang Y, Zhang P, Zhong W, Wang Y, et al. Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods. Acta Pharm Sin B. 2020;10(5):766-788.
- Olwenyi OA, Dyavar SR, Acharya A, Podany AT, Fletcher CV, Ng CL, et al. Immuno-epidemiology and pathophysiology of coronavirus disease 2019 (COVID-19). J Mol Med. 2020:1-5.
- Sarohan AR, Akelma H, Arac E, Aslan O. Retinol Depletion in Severe COVID-19. medRxiv. 2021.
- Baron S. Leptospira--Medical Microbiology. University of Texas Medical Branch at Galveston; 1996.
- Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271-280.
- Harrison AG, Lin T, Wang P. Mechanisms of SARS-CoV-2 transmission and pathogenesis. Trends Immunol. 2020.
- Naqvi AA, Fatima K, Mohammad T, Fatima U, Singh IK, Singh A, et al. Insights into SARS-CoV-2 genome, structure, evolution, pathogenesis and therapies: Structural genomics approach. Biochim Biophys Acta Mol Basis Dis. 2020:165878.
- Chen Y, Liu Q, Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol. 2020;92(4):418-423.
- Yoneyama M, Kikuchi M, Natsukawa T, Shinobu N, Imaizumi T, Miyagishi M, et al. The RNA helicase RIG-I has an essential function in double-stranded RNA-induced innate antiviral responses. Nat. Immunol. 2004;5(7):730-737.
- Choe J, Kelker MS, Wilson IA. Crystal structure of human toll-like receptor 3 (TLR3) ectodomain. Science. 2005;309(5734):581-585.
- Fang Y, Zhou X, Lin M, Ying M, Luo P, Zhu D, et al. Inhibition of all‐Trans‐retinoic acid‐induced proteasome activation potentiates the differentiating effect of retinoid in acute myeloid leukemia cells. Mol Carcinog. 2011;50(1):24-35.
- Sarohan AR. COVID-19: Endogenous Retinoic Acid Theory and Retinoic Acid Depletion Syndrome. Medical hypotheses. 2020;144:110250.
- Ross AC. Vitamin A deficiency and retinoid repletion regulate the antibody response to bacterial antigens and the maintenance of natural killer cells. Clin Immunol Immunopathol. 1996;80(3):S63-S72.
- Liu Y, Olagnier D, Lin R. Host and viral modulation of RIG-I-mediated antiviral immunity. Front. Immunol. 2017;7:662.
- Huang Z, Liu Y, Qi G, Brand D, Zheng SG. Role of vitamin A in the immune system. J Clin Med. 2018;7(9):258.
- Mantlo E, Bukreyeva N, Maruyama J, Paessler S, Huang C. Antiviral activities of type I interferons to SARS-CoV-2 infection. Antiviral Res. 2020;179:104811
- Hu Y, Li W, Gao T, Cui Y, Jin Y, Li P, et al. The severe acute respiratory syndrome coronavirus nucleocapsid inhibits type I interferon production by interfering with TRIM25-mediated RIG-I ubiquitination. J Virol. 2017;91(8).
- Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, et al. COVID-19 infection: the perspectives on immune responses. Nature. 2020; 27:1451–1454.
- Park A. The COVID-19 Virus Is Mutating. What Does That Mean for Vaccines. 2020.
- SARS-CoV WH. Mink-Associated Variant Strain–Denmark. WHO; 2020.
- Greaney AJ, Starr TN, Gilchuk P, Zost SJ, Binshtein E, Loes AN, et al. Complete mapping of mutations to the SARS-CoV-2 spike receptor-binding domain that escape antibody recognition. Cell host & microbe. 2021;29(1):44-57.
- Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, et al. Tracking changes in SARS-CoV-2 Spike: evidence that D614G increases infectivity of the COVID-19 virus. Cell. 2020;182(4):812-827.
- Weisblum Y, Schmidt F, Zhang F, DaSilva J, Poston D, Lorenzi JC, et al. Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants. Elife. 2020;9:e61312.
- Grubaugh ND, Hanage WP, Rasmussen AL. Making sense of mutation: what D614G means for the COVID-19 pandemic remains unclear. Cell. 2020;182(4):794-795.
- Wise J. Covid-19: New coronavirus variant is identified in UK. BMJ 2020;371:m4857.
- Singh J, Ehtesham NZ, Rahman SA, Hasnain SE. Structure-function investigation of a new VUI-202012/01 SARS-CoV-2 variant. bioRxiv. 2021;01.
- FENG E. Transboundary Disease News. 2020.
- Madhi SA, Baillie VL, Cutland CL, Voysey M, Koen AL, Fairlie L, et al. Safety and efficacy of the ChAdOx1 nCoV-19 (AZD1222) Covid-19 vaccine against the B. 1.351 variant in South Africa. medRxiv. 2021.
- Dong Y, Dai T, Wei Y, Zhang L, Zheng M, Zhou F. A systematic review of SARS-CoV-2 vaccine candidates. Signal Transduct Target Ther. 2020;5(1):1-4.
- Lauring AS, Hodcroft EB. Genetic Variants of SARS-CoV-2—What Do They Mean? JAMA. 2021;325(6):529-531.
- Callaway E. Could new COVID variants undermine vaccines? Labs scramble to find out. Nature. 2021;589(7841):177-178.
- Cohen J. South Africa suspends use of AstraZeneca’s COVID-19 vaccine after it fails to clearly stop virus variant. 2021.
- Jennings W, Stoker G, Willis H, Valgardsson V, Gaskell J, Devine D, et al. Lack of trust and social media echo chambers predict COVID-19 vaccine hesitancy. medRxiv. 2021.
- AIDS Institute.Where did HIV come from? AIDS-101.Org
- Dinsa Sachan.The long road to an HIV vaccine. 2017.
- Larijani MS, Ramezani A, Sadat SM. Updated studies on the development of HIV therapeutic vaccine. Curr HIV Res. 2019;17(2):75-84.
- Sautto GA, Kirchenbaum GA, Ross TM. Towards a universal influenza vaccine: different approaches for one goal. Virol J. 2018;15(1):1-2.
- WHO U. Global Action Plan for Prevention and Control of Pneumonia (GAPP): Technical Consensus Statement. Geneva: World Health Organization and United Nations Children’s Fund. 2009.
- Yang HM, Mao M, Wan C. Vitamin A for treating measles in children. Cochrane Database of Systematic Reviews. 2005;(4).
- Grotto I, Mimouni M, Gdalevich M, Mimouni D. Vitamin A supplementation and childhood morbidity from diarrhea and respiratory infections: A meta-analysis. J Pediatr. 2003;142(3):297-304.
- Mehta S, Fawzi W. Effects of vitamins, including vitamin A, on HIV/AIDS patients. Vit Hormon. 2007;75:355-83.
- Penkert RR, Rowe HM, Surman SL, Sealy RE, Rosch J, Hurwitz JL. Influences of vitamin A on vaccine immunogenicity and efficacy. Front Immunol. 2019;10:1576.
- Tan X, Sande JL, Pufnock JS, Blattman JN, Greenberg PD. Retinoic acid as a vaccine adjuvant enhances CD8+ T cell response and mucosal protection from viral challenge. J Virol. 2011;85(16):8316-8327.
- Stephensen CB. Vitamin A, infection, and immune function. Ann Rev Nutr. 2001;21(1):167-192.
- C Pinnock. Vitamin A. Nurs J India. 1991;82(11):307-308.
- Rupp ME, Schwartz ML, Bechard DE. Measles pneumonia: treatment of a near-fatal case with corticosteroids and vitamin A. Chest. 1993;103(5):1625-1626.
- Semba RD (1999) Vitamin A and immune function. Institute of Medicine (US) Committee on Military Nutrition Research. (edn) Military Strategies for Sustainment of Nutrition and Immune Function in the Field. Washington, DC: National Academies Press, USA.
- Calder PC. Nutrition, immunity and COVID-19. BMJ Nutrition, Prevention & Health. 2020;3(1):74.
- Blackfan KD, Wolbach SB. Vitamin A deficiency in infants: A clinical and pathological study. J Pediatr. 1933;3(5):679-706.
- Wolbach SG, and Howe PR. Tissue changes following deprivation of fat-soluble A vitamin. J Exp Med. 1925;42(6):753-777.
- Ross AC, Chen Q, Ma Y. Vitamin A and retinoic acid in the regulation of B-cell development and antibody production. Vit Hormon. 2011;86:103-126.
- Phuapradit W, Chaturachinda K, Taneepanichskul S, Sirivarasry J, Khupulsup K, Lerdvuthisopon N. Serum vitamin A and β-carotene levels in pregnant women infected with human immunodeficiency virus-1. Obstet Gynecol. 1996;87(4):564-567.
- Hussey G, Hughes J, Potgieter S, Kessow G, Burgess J, Beatty D, et al. Vitamin A status and supplementation and its effects on immunity in children with AIDS. InReport of the XVII International Vitamin A Consultative Group Meeting, Guatemala City, Guatemala. International Life Sciences Institute, Washington, DC. 1996;81.
- Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, et al. Characteristics of lymphocyte subsets and cytokines in peripheral blood of 123 hospitalized patients with 2019 novel coronavirus pneumonia (NCP). MedRxiv. 2020.
- Ahmad T, Chaudhuri R, Joshi MC, Almatroudi A, Rahmani AH, Ali SM. COVID-19: The emerging immunopathological determinants for recovery or death. Front Microbiol. 2020;11.
- Duriancik DM, Lackey DE, Hoag KA. Vitamin A as a regulator of antigen presenting cells. Journal Nutr. 2010;140(8):1395-1399.
- Mortaz E, Tabarsi P, Varahram M, Folkerts G, Adcock IM. The immune response and immunopathology of COVID-19. Frontiers in Immunology. 2020;11.
- Kahinho P. Muyayalo, Dong‐Hui Huang, Si‐Jia Zhao, Ting Xie, Gil Mor, Ai‐Hua Liao. COVID-19 and Treg/Th17 imbalance: Potential relationship to pregnancy outcomes. Am J Reprod Immunol. 2020;e13304.
- Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, et al. COVID-19 infection: The perspectives on immune responses. 2020;27:1451-1454.
- Shibabaw T. Inflammatory Cytokine: IL-17A Signaling Pathway in Patients Present with COVID-19 and Current Treatment Strategy. J Inflam Res. 2020;13:673.
- Wu D, Yang XO. TH17 responses in cytokine storm of COVID-19: An emerging target of JAK2 inhibitor Fedratinib. J Microbiol Immunol Infect. 2020;53(3):368-370.
- Wang F, Hou H, Luo Y, Tang G, Wu S, Huang M, et al. The laboratory tests and host immunity of COVID-19 patients with different severity of illness. JCI insight. 2020;5(10).
- Mucida D, Park Y, Kim G, Turovskaya O, Scott I, Kronenberg M, et al. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science. 2007;317(5835):256-260.
- Xiao S, Jin H, Korn T, Liu SM, Oukka M, Lim B, et al. Retinoic acid increases Foxp3+ regulatory T cells and inhibits development of Th17 cells by enhancing TGF-β-driven Smad3 signaling and inhibiting IL-6 and IL-23 receptor expression. J Immunol. 2008;181(4):2277-2284.
- Rampal R, Awasthi A, Ahuja V. Retinoic acid‐primed human dendritic cells inhibit Th9 cells and induce Th1/Th17 cell differentiation. J Leuk Biol. 2016;100(1):111-120.
- Takahashi H, Kanno T, Nakayamada S, Hirahara K, Sciumè G, Muljo SA, et al. TGF-β and retinoic acid induce the microRNA miR-10a, which targets Bcl-6 and constrains the plasticity of helper T cells. Nat Immunol. 2012;13(6):587-595.
- Wang C, Kang SG, HogenEsch H, Love PE, Kim CH. Retinoic acid determines the precise tissue tropism of inflammatory Th17 cells in the intestine. J Immunol. 2010;184(10):5519-5526.
- Matsumiya T, Stafforini DM. Function and regulation of retinoic acid-inducible gene-I. Crit Rev Immunol. 2010;30(6).
- Takeuchi H, Yokota-Nakatsuma A, Ohoka Y, Kagechika H, Kato C, Song SY, Iwata M. Retinoid X receptor agonists modulate Foxp3+ regulatory T cell and Th17 cell differentiation with differential dependence on retinoic acid receptor activation. J Immunol. 2013;191(7):3725-3733.
- C Le Page, P Génin, M G Baines, J Hiscott. Interferon activation and innate immunity. Rev Immunogenet. 2000;2(3):374-86.
- Weber F. Antiviral Innate Immunity: Introduction. Reference Module in Life Sciences. 2020.
- Schreiber G. The Role of Type I Interferons in the Pathogenesis and Treatment of COVID-19. Front Immunol. 2020;11:595739.
- Ross AC. Vitamin A supplementation and retinoic acid treatment in the regulation of antibody responses in vivo. Vitam Horm. 2007;75:197-222.
- Kandasamy S, Chattha KS, Vlasova AN, Saif LJ. Prenatal vitamin A deficiency impairs adaptive immune responses to pentavalent rotavirus vaccine (RotaTeq®) in a neonatal gnotobiotic pig model. Vaccine. 2014;32(7):816-824.
- Semba RD, Scott AL, Natadisastra G, Wirasasmita S, Mele L, Ridwan E, et al. Depressed immune response to tetanus in children with vitamin A deficiency. J Nutr. 1992;122(1):101-7.
- Mwanza-Lisulo M, Kelly P. Potential for use of retinoic acid as an oral vaccine adjuvant. Philos Trans R Soc Lond B Biol Sci. 2015;370(1671):20140145.
- Yazdanpanah F, Hamblin MR, Rezaei N. The immune system and COVID-19: Friend or foe? Life Sci. 2020;256:117900.
- Loo YM, Wilkins CR, Dong R, Pattabhi S, Wang ML, Muñoz EJ, et al. 118: Small molecule RIG-I agonists as vaccine adjuvants and antiviral therapy. Cytokine. 2014;70(1):56.
- Blow RJ. Polyvalent Influenza Vaccine in General Practice. Br Med J. 1964; 2(5414): 943.
Citation: Sarohan AR (2021) New Strategies for COVID-19 Vaccination and Adjuvant Prophylaxis. J Vaccines Vaccin. 12:449.
Copyright: © 2021 Sarohan AR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.