Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Publons
- International committee of medical journals editors (ICMJE)
- Geneva Foundation for Medical Education and Research
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2024) Volume 27, Issue 2
Multiple Relapse in Schizophrenia, Possible Causes and Prevention
Esther I Ezeani1, Obinna V. Chukwuma2, Oluwatosin O. Arubuolawe3, Victory I. Afolabi4, Joanna Obitiye Igo5, Linda Angela Mbah6 and Okelue Edwards Okobi7*2Department of Psychology, Purdue University Global, Indiana, United States of America
3Manhattan Psychiatry Center, New York, United States of America
4Department of Medicine, University of Ibadan, Ibadan, Nigeria
5Department of Medicine, McMaster University, Ontario, California, United States of America
6United States Department of Veterans Affairs, Indiana, United States of America
7Department of Family Medicine, Larkin Community Hospital, Miami, United States of America
Received: 08-Apr-2024, Manuscript No. JOP-24-25422; Editor assigned: 11-Apr-2024, Pre QC No. JOP-24-25422 (PQ); Reviewed: 25-Apr-2024, QC No. JOP-24-25422; Revised: 02-May-2024, Manuscript No. JOP-24-25422 (R); Published: 09-May-2024, DOI: 10.35248/2378-5756.24.27.674
Abstract
In persons with schizophrenia, multiple relapses depict the course of illness, yet the nature of these episodes has not been extensively researched and clinicians may not always be aware of important implications. Most individuals living with schizophrenia experience multiple relapses in the course of their lifetimes. While behaviors may precede the relapses, it has been disclosed that 71% of the behavioral changes may be noticed two weeks prior to the relapses compared to the anomaly rates at other times. Moreover, almost 3 out of every five individuals with schizophrenia experience a relapse in their symptoms after commencing treatment/medication. In most instances, the multiple relapses are increasingly distressing to the patients, their families, and their societies, and not only disrupt the recovery process but also increase the risk of treatment resistance. The objective of this systematic review is, therefore, to evaluate the causes of multiple relapses in patients with schizophrenia, and identify effective ways to prevent the relapses. This study reviewed selected literature concerning the nature and possible causes of multiple relapses in schizophrenia patients and the prevention of relapse. The findings have shown that the key causes of multiple relapses in patients with schizophrenia include non-adherence to treatment, lack of effective social support, substance use and abuse, mental illness-associated stigma, unavailability of essential psychotic medications, and delays in care seeking. The findings of this systematic review indicate that multiple relapse rates are increasingly higher in schizophrenia patients in instances where the treatments have been discontinued, even following a single psychotic episode and that prolonged treatment duration before discontinuation does not result in a reduction in multiple relapse risks. Despite of, timely and effective detection of the relapses and the taking of effectual preventive measures against the potential causative factors are vital for improved prognosis of multiple relapse in schizophrenia patients. Given the inefficiencies of various treatments to prevent full-blown relapse and the possible adverse outcomes, medication adherence and various factors predisposing to multiple relapses need to be the key focus in the management of schizophrenia.
Keywords
Schizophrenia; Multiple relapses; Antipsychotics; Discontinuation
Introduction
Recently, mental disorders have comprised one of the highest global burdens of disease, in which relapse is considered a significant barrier to full recovery and effective rehabilitation. Multiple relapses in schizophrenia is a major issue of concern to patients, their families, and caregivers/healthcare professionals, as it leads to higher distress levels and poor quality of life for the patients [1-3]. Thus, in Schizophrenia, multiple relapses imply the frequent return of the various symptoms following an improvement period marked by severe psychotic exacerbations [4,5]. Multiple relapse in schizophrenia is linked to frequent hospitalization and lead to significant mental care costs [6,7].
During the Schizophrenia course, relapse becomes a common occurrence even in instances where the patients are undergoing treatments. For example, for individuals with schizophrenia, the relapse rate has been acknowledged to range between 50% and 92% globally, even as it is approximated that the rate of relapse is approximately 3.5% per month in psychotic individuals treated using depot antipsychotic treatments [8,9]. Moreover, the initial 2 to 5 years are considered as major determinants of both clinical and functional prognosis related to schizophrenia. The study conducted by Bergé et al. indicated that the relapse rate in schizophrenia was 31% after a year, and a further 43% following 2 years of treatment [10]. A comparable study has disclosed that the rate of relapse during the initial year following the onset of schizophrenia was approximated to be nearly between 34% and 37%, even as the risk of multiple relapse in a lifetime was shown to be approximately 70%, regardless of the pharmacological treatments offered [11,12]. Further, a systematic review and meta-analysis of several longitudinal studies focusing on patients who had experienced an initial episode of psychosis, it was disclosed that the pooled relapse prevalence with regard to positive symptoms was approximately 28% within the 1 year of follow-up, 43% within 2 years of follow-up, and approximately 54% within 3 years of follow-up [13]. Based on such observation Porcelli et al. has maintained that the increment in the number of relapses increases the risk of severity of schizophrenia with severe functional impairments [14]. Thus, multiple relapses have been directly linked to gradual functional deterioration, cognitive impairment, poor clinical prognosis, and increased hospitalizations, which, in turn, result in considerable burdens for both patients and their families [15]. Also, multiple relapses have been noted to increase the risks of social impairment and self-harm [16].
A number of earlier studies have reported on the different modifiable risk factors for multiple relapses in schizophrenia, including lack of proper and effective social support, poor compliance to treatment, substance use and abuse, mental illness-associated stigma, unavailability of essential psychotic medications, and delays in care seeking [17]. The identification of the various factors linked to multiple relapses will aid in the prediction and prevention of relapses in schizophrenia patients. Despite of, available evidence on the related factors and magnitude of multiple relapses in schizophrenia patients remains scarce. As such, the objective of this study is to evaluate the cause of multiple relapse in patients with schizophrenia and how the multiple relapse can be effectively prevented.
Materials and Methods
To collect the relevant literature published in the English language, the researchers performed an in-depth search on a number of online medical databases, including PubMed, Embase, Google Scholar, Web of Science, and SCOPUS, up to January 2024. For this systematic review, the articles had chosen included epidemiological studies and assessment studies, which included anonymized data and different multi-center studies, alongside published review articles. A comparison of the study was also performed to identify duplicate data sources and articles from comparable population years, even as study sources that had increasingly valid details were included and used. Moreover, for the literature search, keywords, including “schizophrenia,” “relapse,” and “multiple relapse,” were used. A total of 769 articles were yielded through the literature search.
Inclusion and exclusion criteria
After the removal of all identified duplicates, relevant literature/ articles were subsequently selected in three distinctive stages. The first stage involved the screening of the selected literature’s titles and abstracts, even as the second stage involved the exclusion of all articles found to be irrelevant to this study. The third stage involved the performance of an in-depth full-text exploration of the selected literature with the aim of ensuring the right and relevant articles are selected and included. The three stages of literature screening stages were carried out by three independent reviewers, and the resolution of the discrepancies realized was done through consultations and consensus.
Further, the inclusion criteria included original studies, including crossover design studies, Randomized Controlled Trials (RCTs), and prospective cohort studies that met the following set criteria: studies had to focus on relapse in schizophrenia patients and treatment of multiple relapse; studies on persons with schizophrenia; medical interventions; published in English language, and conducted between 2000 and 2014. Additionally, sponsored clinical trials, narrative reviews and editorials were excluded. The initial evaluation of the abstracts of the articles resulted in the removal of 478 articles. Additionally, for this systematic review, vita data from the qualified literature was extracted as follows: (i) general attributes of the study, such as the names of the authors, study year, publication year, and the employed sampling methods; (ii) the attributes of the study population, including race, participants age and gender/sex, sample size, and follow-up; (iii) type of intervention and duration, and measures used in assessing weight; and (iv) the major findings of the study.
Lastly, for this systematic review, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was utilized in the literature selection process. From the literature selection process, 769 articles were retrieved following the performance of an in-depth database search. The subsequent screening of the articles resulted in the removal of 478 duplicates together 122 articles determined to be ineligible through automation, and an extra 73 articles were excluded for other notable reasons, including the failure to align with this study's objectives, and animal-based studies. Further, dissertations and studies published in non-peer-reviewed journals were excluded. Still, studies initially published in non- English languages were excluded alongside opinion pieces, scoping reviews, non-academic articles, secondary studies, and other research types that were not primary studies were also excluded. Therefore, 96 eligible articles were further screened leading to the exclusion of 45 articles. The remaining 51 articles were sought for retrieval, and 8 articles could not be retrieved. As a result, 43 articles were assessed for eligibility and 17 articles were excluded following full-text screening for reasons that included: full text not retrievable after contacting the authors (5 articles), preprints (2 articles); failure to assess targeted interventions (4 articles); protocol (3 articles), and failure to report on the limitations (3 articles). The PRISMA flow diagram presented in Figure 1, below indicated the article selection process.
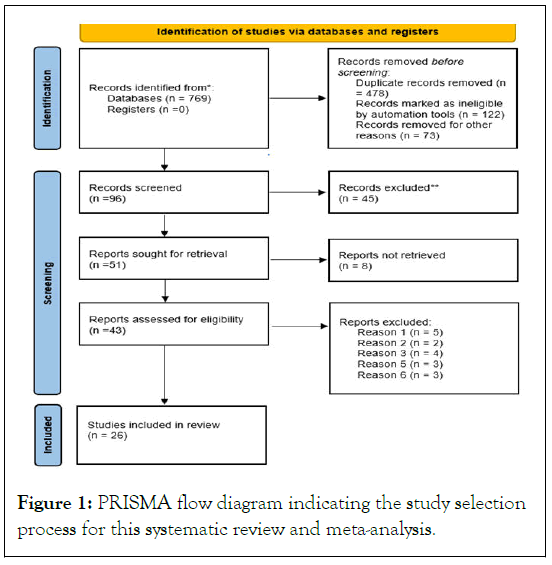
Figure 1: PRISMA flow diagram indicating the study selection process for this systematic review and meta-analysis.
Results and Discussion
The evaluation and management of incidences of multiple relapse in patients with schizophrenia is of immense importance to clinical practice, in addition to being an important aspect for the controlled clinical studies. Therefore, increased awareness on the various factors linked to both the increment and decrement of the relapse rates need to invariably aid the clinical practice and also benefit the patients with schizophrenia. Studies have indicated that some of the most notable factors linked to multiple relapse in schizophrenia include the psychotic episodes frequency, substance use and misuse, comorbid psychiatric conditions, non-adherence to treatment, stressful life events, unemployment, psychotic stress, and treatment side effects [13,18]. In this regard, a number of studies have shown that following 1-3 years of schizophrenia episodes, the patients often have a relapse rate ranging between 19% to 65% [19,20]. The anticipation of the relapse is considered a vital aspect in treatment planning and also for prospective studies; for instance, a study conducted in Germany disclosed that slightly higher than 50% of patients with schizophrenia experienced multiple relapses and also that approximately 40% of patients with schizophrenia who were treated using atypical antipsychotic medications were prone to experience multiple relapses within 1 year following discharge from hospital [20,21]. Additional approximations have placed the probability of multiple relapses at 77% during the initial year, as well as up to 90% during the second and third years, despite the approximation that only 3% of patients with schizophrenia who continue with the medication regime tend to experience multiple relapses [22]. A study conducted in Ethiopia in 2010 has disclosed that more than 60% of the mental-related hospitalizations were mainly schizophrenia-related, and this had higher levels of impairment, stigma, family hardships, human rights abuses and mortality. Still, a number of recent cross-sectional studies that evaluated prevalence of schizophrenia revealed that multiple relapses were noted in between 24% to 88% of patients hospitalized as a result of schizophrenia [23]. The cost of care associated with multiple relapses in patients with schizophrenia has been the underlying aspect in the relapse prevention efforts.
Moreover, as a chronic disorder, schizophrenia is mainly characterized by the sporadic episodes of severe exacerbation along with partial or full remission. A recent study has indicated that approximately 57% of patients with schizophrenia experience multiple relapses in their lifetime, with nearly 31% of them experiencing relapses within 2 years, even as 48% and 21% of them experience relapses within 2 to 5 years and after 5 years following treatment, respectively [24]. Even though the atypical antipsychotics have been found to be efficient with regard to reduction of the severe symptoms and delaying or preventing relapse in a number of trials, the relapse rates have remained high, leading to the increment in poor prognosis and economic burdens for the patients and their families [16,25,26]. Given that the key purpose of antipsychotic medications and therapy, other than from the initial use in managing the symptoms, may be to avert potential relapse devoid of increasing the possible negative effects, this shows the enduring unmet needs with regard to schizophrenia treatment.
The notable causes of multiple relapse in schizophrenia patients include lack of adherence to the treatment, lack of insight into the condition, acute residual psychopathology and comorbid substance abuse, poor relationship with family and care providers [8]. Thus, it has been shown that non-compliance with treatment, caregiver’s criticism, persistent substance use, and poor premorbid adjustments considerably increases the risk of multiple relapse following the initial psychosis episode [13]. A prospective 5-year follow-up study has additionally disclosed that the most common risk factor for multiple relapse in schizophrenia patients was the discontinuation of antipsychotic medication [27]. Despite of the identified underlying factors for multiple relapse, poor or non-compliance to treatment regimen has been highlighted at the key contributory cause [28]. Nonadherence may be attributed to patient-related factors that include cognitive impairment, psychopathology, age, gender/sex, insight, comorbidity, and personality traits, as well as treatmentrelated factors like tolerability, admission route, and personality traits, as well as treatment-settings-related factors such as social support, therapeutic relationships, treatment supervision, treatment provision location, illness social ranking, and patient, physician attitudes towards treatment [29].
In comparison to the conventional antipsychotics, the Extrapyramidal Symptoms (EPS) lower levels alongside the Adverse Events (AEs) often experienced by schizophrenia patients who have been prescribed atypical antipsychotics may be anticipated to bring about improvements in compliance to treatments, and as a result, lead to low relapse rates [30]. In this regard, a study conducted on patients with schizophrenia has indicated considerably reduced relapse rates in patients who underwent atypical antipsychotic treatments in comparison to those treated using haloperidol. The multiple relapses in schizophrenia have additionally been attributed to the rebound effects linked to haloperidol, chlorpromazine, and other notable typical antipsychotic medications following the sudden interruption of treatment [31]. The kinds of adverse events related to the withdrawal effects of the different antipsychotics like chlorpromazine include headache, nausea and vomiting, perspiration, diarrhea, sleeplessness, and restlessness, all of which are not just transient but also occurring during the initial two weeks [32].
Non-adherence to the prescribed medication regimen remains a vital factor for multiple relapse in patients with schizophrenia, subsequently increasing hospital admission risks [33,34]. The outcomes of medication non-adherence include poorer care/ clinical outcomes, lower quality of life, increase in disability and morbidity, decrements in personal and work productivity, and increased cost of healthcare [35]. While the causes of medication non-compliance remain multifactorial, negative attitudes have been noted to play a key role in non-compliance [34]. Adherence to medication is, therefore, among the most effective ways of averting multiple relapses in patients with schizophrenia [36].
Additionally, multiple relapses in schizophrenia have been linked to disease progression [27]. Also, multiple relapse has been linked to psychosocial risks, as active psychosis tends to have fundamental effects on the brain. A number of recent studies have, in this regard, proposed that psychosis might be neurotoxic, and severe psychotic exacerbations are representative of the active periods of the morbid process, leading to the progression of the disease and the treatment response impairments [27,37,38]. Initially, evidence supporting this observation has been offered by a well-replicated study finding that showed that prolonged and untreated psychosis was linked to poor long-term outcomes [39]. Still, relapses in patients with schizophrenia are representative of active psychosis episodes and might be linked to the progression of the disease. Despite of, at present, limited empirical evidence supporting the hypothesis on neurotoxic psychosis exists, and particularly for the progression of the illness following relapses. An in-depth literature search has, however, revealed that treatment response improved during the initial episode of schizophrenia in comparison to subsequent multiple relapse episodes [38]. Furthermore, a recent study that utilized a neuroleptic threshold principle disclosed that the first-episode schizophrenia patients needed lower haloperidol dosages to realize optimal clinical response compared to patients who have experienced multiple relapse episodes, raising the probability of development of antipsychotics effects tolerance [40]. Still, 80% of schizophrenia patients have been observed to have experienced considerable deterioration overtime in a follow-up study conducted over a 7- year period, even as the deterioration level had a considerable correlation with multiple relapses experienced by patients [41]. Consequently, an additional study has, however, disclosed that multiple relapse in patients with schizophrenia is not linked to the progression of the disease, given that the symptoms often resumes the baseline upon the patients’ resumption of antipsychotic medications immediately after the symptoms recurrence [42].
Additionally, stressful life events alongside the existence of other major comorbid mental conditions are considered as factors capable of causing multiple relapses in patients with schizophrenia [23,43]. A study conducted by Beards et al. disclosed that patients who underwent three or more stressful life events had twice odds (AOR of 2.40) of experiencing multiple relapse compared to other schizophrenia patients, and this has been further supported by a study conducted in Iraq and a recent meta-analysis [44,45]. It has also been noted that patients with schizophrenia who experience multiple relapse had increasingly recurrent relationship challenges and personal stressors in comparison to patients who had not experienced relapse [2]. This may be clarified through the use of the Stress- Vulnerability model that places emphasis on the observation that patients with schizophrenia possess biologically-mediated susceptibility to various stressful events that might bring about severe psychosis. Stress presents direct psychological effects on the human body, behavioral and cognitive effects, as well as secondary effects through exacerbation of illnesses, in addition to causing delays in recovery [46]. Therefore, cognitive susceptibility improves the individual vulnerability to stressful events, and can be regarded as a major reason for relapse in patients with schizophrenia. This necessitates the evaluation of cognitive disturbance alongside the execution of coping skills training as schizophrenia patients tend to have less effectual coping skills [45].
In a recent study conducted in Ethiopia and Pakistan, the researchers disclosed that odds of experiencing multiple relapse in schizophrenia patients with comorbidity of other mental disorders was nearly 1.84 times, with an AOR of 1.84, and increased in instances where comparison was made in relation to patients who did not have any comorbidity of other major mental conditions [29,43]. The existence of comorbid mental illnesses often compromises the psychotropic medication compliance. The findings of other studies have shown that medication non-compliance was linked to the existence of comorbidities with the extant mental disorder (schizophrenia) [47,48]. Further, the comorbid mental disorders existence may themselves be considered a key risk factor for medication non-compliance. For instance, depression has been directly linked to medication non-compliance in persons with psychiatric diagnoses. Non-compliance as a result of comorbid psychiatric disorder mainly results from the increased complexity of the medication regimen, as well as the increased concerns regarding the treatment’s potential adverse consequences, even as non-adherence, in turn, results in relapse [43,49,50]. This demonstrates the importance of medication adherence for patients, as it enables effective control of the symptoms and prevents multiple relapses. Therefore, interventions and strategies that seek to enhance adherence to medication will aid in the prevention and mitigation of multiple relapses in patients with schizophrenia. Moreover, screening for the mental illness comorbidities and various stressful life events, the provision of specific treatments, as well as aiding schizophrenia patients with the development of coping strategies, will help in the prevention and decrement of the risks associated with multiple relapses.
Still, the other notable factor that has been attributed to cause multiple relapse in patients with schizophrenia is unemployment. Various studies have disclosed that the prevalence rate of unemployment among individuals with schizophrenia ranged between 75% to 90% in adult persons with schizophrenia, and that unemployment was a major contributor to multiple relapses in the group [51]. Hypothetically, unemployment can be linked to an additional high risk aspect, for instance, the household income. Despite of, no collinearity exists between the two aspects are shown in Table 1.
| Biological factors | Psychological factors | Social factors | Environmental factors |
|---|---|---|---|
| Genetic predisposition | Stress and trauma | Lack of social support | Substance abuse |
| Neurochemical imbalance | Poor coping mechanisms | Stigma and discrimination | Urbanisation |
| Neuroanatomical abnormalities | Cognitive deficits | Family dysfunction | Life events and changes |
| Abnormalities in brain structure and function | Emotional dysregulation | Housing instability | Excessive noise and crowding |
| Pharmacological factors (medication non-adherence, adverse effects) | Maladaptive beliefs and attitudes | Unemployment and financial strain | Urban environment |
| Neurodevelopmental abnormalities | Excessive self-criticism | Social isolation | Exposure to violence or trauma |
| Neuroinflammation | Perceived social threat | Relationship conflicts | Access to mental health care |
| Hormonal fluctuations | Lack of insight | Caregiver stress | Substance availability and exposure |
| Immunological factors | Rumination | Cultural factors | High levels of pollution |
Table 1: Some causes of multiple relapses in schizophrenia.
A potential clarification for this entails the observation that the household income does not aptly mirror the individual incomes of the patients with schizophrenia, and that only a portion of the patients (approximately 4.2%) are living alone [52]. Further, it has been disclosed that the challenging daily living ability was predictive of multiple relapse in patients with schizophrenia [52]. As such, various social skills training is proposed to enhance the deficits in the daily life abilities of patients with schizophrenia [53]. In addition to the numerous aptly documented factors linked to psychotic relapse, the significant role of household income along with the medical costs selfpayment in relation to multiple relapse has been emphasized [52]. A clarification provided through the use of the decision tree model entailed the observation that the unemployment and lower income schizophrenia patients seemed to be a key predictors of household incomes and medical costs. The above two risk factors have not been considered as major predictors of multiple relapse in schizophrenia patients in earlier studies carried out in developed nations [54-56], and this can be attributed to the nations’ comparatively advanced public health services and healthcare systems. For instance, in China, hospitals are placed in a three-tier system, including primary, secondary, and tertiary hospitals, which acknowledge the ability of a hospital to offer the necessary care services to patients [57]. It has further been disclosed that schizophrenia patients receiving treatment in various non-tertiary healthcare institutions, including primary and secondary institutions, are highly prone to experience multiple relapses, and this observation has been supported by the findings of the study conducted Mi et al., which has proposed improvement of the ability of primary and secondary institutions to treat mental illnesses [52,57].
Prevention of multiple relapse
In acknowledging the various related risks, it has been observed that enhancing medication adherence not only improves multiple relapse prevention but is additionally a major schizophrenia management component [24]. Patients treated with atypical antipsychotics have lower Extrapyramidal Symptoms (EPS) and adverse events thus improves medication adherence and reduces relapse rates [58]. To this end, a recent study of patients with schizophrenia had indicated considerably lower relapses rates, particularly in patients who were treated using atypical antipsychotics in comparison to those treated using haloperidol [59]. In addition to being the 1st line schizophrenia treatment, atypical antipsychotic quetiapine has shown increased efficiency across a wider array of symptoms and has been compared to other atypical antipsychotics [60]. Moreover, quetiapine has demonstrated increased efficiency with regard to treatment of different anxiety symptoms in patients with bipolar disorder, as well as agitation in schizophrenia patients [61,62]. Additionally, earlier evidence has shown efficiency in the treatment of major depressive disorder and generalized anxiety disorder [63]. Still, quetiapine has shown low propensity to cause EPS in comparison to chlorpromazine, risperidone, and haloperidol, and also has EPS incidence, such as akathisia, alongside prolactin levels comparable to placebo treatments throughout the dose range among schizophrenia patients [64-66]. Studies have also shown quetiapine to be linked to a considerably reduced tardive dyskinesia risk in schizophrenia patients in comparison to the conventional antipsychotics [67].
Additionally, various studies have focused on prevention of single relapse and multiple relapses in patients with schizophrenia. From the selected literature, there were 36 occurrences, within 27 publications, related to factors that might aid in the reduction of the relapse rates in patients with schizophrenia. The antipsychotic treatments’ potential to effectively minimize and prevent multiple relapse has been evaluated by a total of (number of studies) that met the inclusion criteria in this systematic review. One of the studies reviewed was a 3-year follow-up study comprising a bigger cohort (n=6516) of patients with schizophrenia who participated in an observational and prospective European Schizophrenia Outpatient Health Outcomes study [68]. The study disclosed a higher relapse rate among patients on typical antipsychotics, particularly depot, in comparison to those on atypical antipsychotic medications, including olanzapine. Further, significant differences with regard to the risk rate for multiple relapse was between atypical antipsychotic (olanzapine) and other notable second generation antipsychotics [68]. An additional study indicated that schizophrenia patients treated using depot antipsychotics presented higher multiple relapse rates alongside increased hospitalization rates in comparison to patients who were not given depot antipsychotics [69]. Further, the Risperidone Long- Acting Injectable (RLAI)’s effects with regard to relapse rate and the duration of relapses in comparison to the baseline or patients with schizophrenia treated using oral antipsychotics has been reported on a number of studies [70]. Similarly, higher relapse rates, attributable to the rebound effects have previously been reported with the use of typical antipsychotics that include haloperidol and chlorpromazine, following sudden interruption of schizophrenia treatment [71]. The withdrawal of antipsychotics like chlorpromazine includes headaches and migraines, perspiration, sleeplessness, restlessness, diarrhea, and nausea and vomiting, which are all transient and happen during the initial two weeks [72,73]. In another 2-year study that focused on oral antipsychotic and a RLAI, the administration of RLAI to schizophrenia patients was directly linked to a 9.3% relapse rate in comparison to 42.1%relapse rate in patients treated using oral antipsychotics [74]. Additionally, in a study comparing hospitalization at 1 and 2 years after RLAI initiation, greater decreases from baseline in the number of patients hospitalized and the number and length of hospital stays in patients who continued with RLAI treatment were observed, compared with those who discontinued [74].
Although antipsychotics are considered effective in the prevention of multiple relapses in patients with schizophrenia, they have been linked to a number of considerable side effects, and Cochrane review has disclosed that 24% of schizophrenia patients tend to experience a relapses within one year following treatment, regardless of the drug therapy [75]. As a result, numerous psychological and psychosocial interventions have been developed with the objective of preventing multiple relapses in individuals with schizophrenia. These nonpharmacological interventions play an important role with regard to prevention of multiple psychotic episodes [76].
Still, various non-pharmacological interventions aimed at reducing multiple relapses, including Cognitive Behavioral Therapy (CBT) and psychoeducation have been widely reported as key factors that aid in the reduction of multiple relapses in patients with schizophrenia. Despite of the above non-pharmacological interventions have been evaluated in patients who have been on antipsychotic medication treatments, with a number of studies highlighting a tendency that associates nonpharmacological interventional therapies like psychoeducation and CBT with reduction in relapse rates, even as they failed to show statistically significant effects within the naturalistic or observational contexts [77,78].
Further, the findings of this systematic review have disclosed that family interventions, CBT, family psycheducation, patient psycheducation, relapse prevention programs, and integrated interventions are superior compared to the standard care programs only in the prevention of multiple relapses at 1 year after the initial treatment. Thus, the above interventions have been found to have indicated consistent patterns during three time points considered, even as there was broader overlapping of confidence intervals, with limited notable exceptions [79]. However, it is worth noting that family psychoeducation and family interventions have been found to be less effective than the conventional treatment at 6 months, even though they are more effective than conventional treatment after 1 year [80]. The above observation is consistent with the findings of the Cochrane study conducted by Giron et al [81]. On the other hand, assertive community treatment was found to be effective at only 6 months following the initial treatment, even as CBT was found to be more effective at 1st year following the initial treatment, but ineffective in the long run. Remarkably, different studies have indicated results at divergent time points, with fewer studies reporting data at 6 months and over 1 year, in comparison to 1 year, resulting in low power at the different secondary time points.
Additionally, family interventions have been effective in enhancing other outcomes that include schizophrenia symptoms and functioning. As such, the prevention effects on multiple relapses might be effectively mitigated through other factors, including improved functioning, better compliance/adherence to medication, symptoms reduction, and direct family involvement [79]. Family members may be increasingly capable of managing crises, thereby reducing relapse rates and hospital admissions. Simple interventions such as family psychoeducation have been acknowledged to be effective with regard to prevention of multiple relapses and enhancing the symptoms of schizophrenia in patients [79,82]. Thus, in instances where resources are inadequate, the provision of family psychoeducation is considered as the most appropriate minimum solution. However, family psychoeducation and family interventions require a lot of time to be effective, and have been acknowledged to minimize the risk of multiple relapse after one year [82]. On the contrary, studies have indicated that, unlike family interventions and psychoeducation, the provision of mere support for either family or relation did not have any effects [83]. The divergent family interventions types’ effects are still under study in continuing network meta-analysis [83]. It has also been disclosed that patient psychoeducation is usually more effective in comparison to treatment at 1st year, but not effective at 6 months and after 1 year, even though with increasingly overlapping confidence intervals [80].
The Cochrane review conducted by Xia et al. has reported that patient psychoeducation is effective in prevention of multiple relapse in schizophrenia patients after 1 year. Moreover, based on this review, we have observed that patient psychoeducation in patients with schizophrenia is effective in the reduction of symptoms and in enhancing adherence in comparison to normal treatment. Also, CBT (Cognitive Behavior Therapy) has been reported to be effective in reduction of the rate of relapse in schizophrenia patients at 1st year, as well as in enhancing the secondary outcomes. Consistent with the outcomes of the study conducted by Jørgensen et al., the advantages of reduction of relapse in the long-term remains unclear [78]. Although CBT has not been developed particularly for the prevention of relapse, its main objective is to reduce the persistent psychotic symptoms, which it has effectively achieved [84]. In this regard, it has been proposed that other CBT modules may be developed with the objective of enhancing its effects for the long-term prevention of multiple relapse in schizophrenia.
Lastly, the psychosocial interventions that include assertive community treatment, rehabilitation, and case management whose objective is to provide a structure to the patient’s life outside the hospital, through home visitation of the patient, provision of the reference figure for the service organization, and provision of effective rehabilitation activities. While rehabilitation has been noted to have promising outcomes with regard to prevention of multiple relapses, assertive community treatment has been noted to reduce the relapse risk at 6 months, even as the case management had confidence intervals that included probability of no dissimilarity with normal treatment. The above observations are consistent with earlier findings of reviews that disclosed that assertive community treatment was effective in the prevention of multiple relapses in schizophrenia, even as case management did not prefer any protective effect [85,86]. Other notable psychosocial interventions were not effective in reducing the relapse risk in schizophrenia. However, for a number, this might not be surprising, given that they are mainly developed with different objectives other than focus on prevention of relapse. It focuses on training social skills, in addition to availability of little evidence as seen in the case of telemedicine and cognitive training.
Conclusion
In summary, the present systematic review has revealed that the effect of multiple relapse in schizophrenia was as widespread as noted in earlier studies. Thus, approximately three out of every five patients with schizophrenia had experienced multiple symptoms relapse during their lifetime following hospitalization and commencement of medication. Despite of, this systematic review has also disclosed that multiple relapse was widespread in persons with other comorbid psychological conditions, shorter treatment durations, stressful life events, and treatment nonadherence. Therefore, the present systematic review provides study evidence indicating that poor adherence to medication, stressful events related to unemployment and difficulties in activities of daily living, low household incomes, and medical insurance costs were the key multiple relapse predictors in patients with schizophrenia, particularly 1 year following discharge from hospital. Adherence to medication has been found to be a major predictor of multiple relapses in schizophrenia. The study revealed the use of atypical antipsychotics and long acting antipsychotics injectable improved adherence hence reduced multiple relapses in the management of schizophrenia. Also non-pharmacological management of schizophrenia such as CBT, family intervention, family psychoeducation, patient psychoeducation, relapse prevention programmes and community treatment rehabilitation have aided in reduction of multiple relapse in schizophrenia. There is a need for studies that evaluate intervention strategies to focus on the reduction of relapse rates and enhancement of insights into schizophrenia. Lastly, careful considerations are needed in relation to determination of the effects of the discontinuation of antipsychotic medication in both clinical practice and the placebo-controlled clinical studies.
References
- Funk, M., Ivbijaro, G. Integrating mental health into primary care: A global perspective. World Health Organization. 2008.
- Kazadi NJ, Moosa MY, Jeenah FY. Factors associated with relapse in schizophrenia. S Afr J Psychi. 2008;14(2):52-62.
- Adebiyi MO, Mosaku SK, Irinoye OO, Oyelade OO. Socio-demographic and clinical factors associated with relapse in mental illness. Int J Afr Nurs Sci. 2018;8:149-153.
- Kane JM. Treatment strategies to prevent relapse and encourage remission. J Clin Psychiatry. 2007;68:27.
- Chaurotia VK, Verma KK, Baniya GC. A study of psychosocial factor related with relapse in schizophrenia. IOSR J Dent Med Sci Ver XIV. 2016;15(4):2279-2861.
- Capdevielle D, Boulenger JP, Villebrun D, Ritchie K. Schizophrenic patients' length of stay: Mental health care implication and medicoeconomic consequences. L Encephale. 2009;35(4):394-399.
- Papakostas S, Dar A, Ratna L. Sociodemographic factors and medication administration factors affecting re–hospitalization in patients with schizophrenia–spectrum disorders. Psychiatr Q. 2020;91:1363-1369.
- Csernansky JG, Schuchart EK. Relapse and rehospitalisation rates in patients with schizophrenia: Effects of second generation antipsychotics. CNS Drugs. 2002;16:473-484.
- Weret ZS, Mukherjee R. Prevalence of relapse and associated factors in patient with schizophrenia at Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia: Institution based cross sectional study. Int J Interdiscip Multidiscip Stud. 2014;2(1):184-1892.
- ' D, Mané A, Salgado P, Cortizo R, Garnier C, Gomez L, et al. Predictors of relapse and functioning in first-episode psychosis: a two-year follow-up study. Psychiatr Serv. 2016;67(2):227-233.
- Addington DE, Patten SB, McKenzie E, Addington J. Relationship between relapse and hospitalization in first-episode psychosis. Psychiatr Serv. 2013;64(8):796-799.
- Sommer IE, Tiihonen J, van Mourik A, Tanskanen A, Taipale H. The clinical course of schizophrenia in women and men—a nation-wide cohort study. NPJ schizophrenia. 2020;6(1):12.
- Alvarez-Jimenez M, Priede A, Hetrick SE, Bendall S, Killackey E, Parker AG, et al. Risk factors for relapse following treatment for first episode psychosis: a systematic review and meta-analysis of longitudinal studies. Schizophr Res. 2012;139(1-3):116-128.
- Porcelli S, Bianchini O, De Girolamo G, Aguglia E, Crea L, Serretti A. Clinical factors related to schizophrenia relapse. Int J Psychiatry Clin Pract. 2016 Apr 2;20(2):54-69.
- Pigott TA, Carson WH, Saha AR, Torbeyns AF, Stock EG, Ingenito GG. Aripiprazole for the prevention of relapse in stabilized patients with chronic schizophrenia: A placebo-controlled 26-week study. J Clin Psychiatry. 2003;64(9):1048-1056.
- Almond S, Knapp M, Francois C, Toumi M, Brugha T. Relapse in schizophrenia: Costs, clinical outcomes and quality of life. B J Psych. 2004;184(4):346-51.
- Fikreyesus M, Soboka M, Feyissa GT. Psychotic relapse and associated factors among patients attending health services in South west Ethiopia: A cross-sectional study. BMC Psychiatry. 2016;16:1-0.
- Alphs L, Nasrallah HA, Bossie CA, Fu DJ, Gopal S, Hough D, et al. Factors associated with relapse in schizophrenia despite adherence to long-acting injectable antipsychotic therapy. Int Clin Psychopharmacol. 2016;31(4):202-209.
- Lee SU, Soh M, Ryu V, Kim CE, Park S, Roh S, et al. Analysis of the health insurance review and assessment service data from 2011 to 2015. Int J Ment Health Syst. 2018;12(1):1-9.
- Schennach R, Obermeier M, Meyer S, Jäger M, Schmauss M, Laux G, et al. Predictors of relapse in the year after hospital discharge among patients with schizophrenia. Psychiatr Serv. 2012;63(1):87-90.
- Emsley R, Chiliza B, Asmal L, Harvey BH. The nature of relapse in schizophrenia. BMC Psychiatry. 2013;13:1-8.
- Zipursky RB, Menezes NM, Streiner DL. Risk of symptom recurrence with medication discontinuation in first-episode psychosis: a systematic review. Schizophr Res. 2014;152(2-3):408-414.
- Ayano G, Duko B. Relapse and hospitalization in patients with schizophrenia and bipolar disorder at the St Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia: A Comparative quantitative cross-sectional study. Neuropsychiatr Dis Treat. 2017:1527-1531.
- Moges S, Belete T, Mekonen T, Menberu M. Lifetime relapse and its associated factors among people with schizophrenia spectrum disorders who are on follow up at Comprehensive Specialized Hospitals in Amhara region, Ethiopia: A cross-sectional study. Int J Ment Health Syst. 2021;15(1):42.
- Leucht S, Barnes TR, Kissling W, Engel RR, Correll C, Kane JM. Relapse prevention in schizophrenia with new-generation antipsychotics: A systematic review and exploratory meta-analysis of randomized, controlled trials. Am J Psychiatry. 2003;160(7):1209-1222.
- Guinart D, Taipale H, Rubio JM, Tanskanen A, Correll CU, Tiihonen J, et al. Risk factors, incidence, and outcomes of neuroleptic malignant syndrome on long-acting injectable vs. oral antipsychotics in a nationwide schizophrenia cohort. Schizophr Bull. 2021;47(6):1621-1630
- Brandt L, Ritter K, Schneider-Thoma J, Siafis S, Montag C, Ayrilmaz H, et al. Predicting psychotic relapse following randomised discontinuation of paliperidone in individuals with schizophrenia or schizoaffective disorder: An individual participant data analysis. The Lancet Psychiatry. 2023;10(3):184-196.
- Leucht S, Heres S. Epidemiology, clinical consequences, and psychosocial treatment of nonadherence in schizophrenia. J Clin Psychia. 2006;67:3.
[Google Scholar] [PubMed]
- Fleischhacker WW, Oehl MA, Hummer M. Factors influencing compliance in schizophrenia patients. J Clin Psychia. 2003;64:10-13.
[Google Scholar] [PubMed]
- Citrome L, Volavka J. The promise of atypical antipsychotics: Fewer side effects mean enhanced compliance and improved functioning. Postgrad. Med. 2004;116(4):49-63.
- Horowitz MA, Jauhar S, Natesan S, Murray RM, Taylor D. A method for tapering antipsychotic treatment that may minimize the risk of relapse. Schizophr Bull. 2021;47(4):1116-1129.
- Buckley PF. Receptor-binding profiles of antipsychotics: clinical strategies when switching between agents. J Clin Psychia. 2007;68:5.
[Google Scholar] [PubMed]
- Üçok A, Polat A, Çakır S, Genç A. One year outcome in first episode schizophrenia: Predictors of relapse. Eur Arch Psychiatry Clin Neurosci. 2006;256:37-43.
- Yalcin-Siedentopf N, Wartelsteiner F, Kaufmann A, Biedermann F, Edlinger M, Kemmler G, et al. Measuring adherence to medication in schizophrenia: The relationship between attitudes toward drug therapy and plasma levels of new-generation antipsychotics. Int J Neuropsychopharmacol. 2015;18(5):pyu091.
- Rüsch N, Todd AR, Bodenhausen GV, Weiden PJ, Corrigan PW. Implicit versus explicit attitudes toward psychiatric medication: Implications for insight and treatment adherence. Schizophr Res. 2009;112(1-3):119-122.
- Velligan DI, Weiden PJ, Sajatovic M, Scott J, Carpenter D, Ross R, et al. Strategies for addressing adherence problems in patients with serious and persistent mental illness: recommendations from the expert consensus guidelines. J Psychiatr Pract. 2010;16(5):306-324.
- Goldsmith LP, Lewis SW, Dunn G, Bentall RP. Psychological treatments for early psychosis can be beneficial or harmful, depending on the therapeutic alliance: An instrumental variable analysis. Psychol Med. 2015;45(11):2365-2373.
- Fond G, d’Albis MA, Jamain S, Tamouza R, Arango C, Fleischhacker WW, et al. The promise of biological markers for treatment response in first-episode psychosis: a systematic review. Schizophr Bull. 2015;41(3):559-573.
- Tang JY, Chang WC, Hui CL, Wong GH, Chan SK, Lee EH, et al. Prospective relationship between duration of untreated psychosis and 13-year clinical outcome: A first-episode psychosis study. Schizophr Res. 2014;153(1-3):1-8.
- Barnes TR, Paton C. Antipsychotic polypharmacy in schizophrenia: benefits and risks. CNS Drugs. 2011;25:383-399.
- Uchida T, Suzuki T, Sakurai H, Tsutsumi C, Den R, Mimura M, et al. Ten year outcomes of outpatients with schizophrenia on conventional depot antipsychotics: A systematic chart review. Int Clin Psychopharmacol. 2013;28(5):261-266.
- Moncrieff J, Gupta S, Horowitz MA. Barriers to stopping neuroleptic (antipsychotic) treatment in people with schizophrenia, psychosis or bipolar disorder. Ther Adv Psychopharmacol. 2020;10:2045125320937910.
- Ahmad I, Khalily MT, Hallahan B. Reasons associated with treatment non-adherence in schizophrenia in a Pakistan cohort. Asian J Psychiatr. 2017;30:39-43.
- Beards S, Gayer-Anderson C, Borges S, Dewey ME, Fisher HL, Morgan C. Life events and psychosis: A review and meta-analysis. Schizophr Bull. 2013;39(4):740-747.
- Hussein HA, Jacoob S, Sharour LA. Impact of life events on the relapse of schizophrenic patients. J Educ Pract. 2016;7(10):40-47.
- Biliaminu A, Aina J. Assessment of factors associated with treatment relapse among patients diagnosed with psychotic illness in two psychiatric hospitals in South west, Nigeria. African Journal of Health, Nursing and Midwifery. 2020;3(5):12-53.
- Taj F, Tanwir M, Aly Z, Khowajah AA, Tariq A, Syed FK, et al. Factors associated with non-adherence among psychiatric patients at a tertiary care hospital, Karachi, Pakistan: A questionnaire based cross-sectional study. J Pak Med Assoc. 2008;58(8):432.
[Google Scholar] [PubMed]
- Sajatovic M, Valenstein M, Blow FC, Ganoczy D, Ignacio RV. Treatment adherence with antipsychotic medications in bipolar disorder. Bipol Dis. 2006;8(3):232-241
- Montes JM, Maurino J, de Dios C, Medina E. Suboptimal treatment adherence in bipolar disorder: impact on clinical outcomes and functioning. Patient Prefer Adherence. 2013:89-94.
- Hui CL, Tang JY, Leung CM, Wong GH, Chang WC, Chan SK, et al. A 3-year retrospective cohort study of predictors of relapse in first-episode psychosis in Hong Kong. Aust N Z J Psychiatry. 2013;47(8):746-753.
- Haslett WR, McHugo GJ, Bond GR, Drake RE. Use of software for tablet computers to promote engagement with supported employment: results from an RCT. Psychiatr Serv. 2014;65(7):954-956.
- Mi WF, Chen XM, Fan TT, Tabarak S, Xiao JB, Cao YZ, et al. Identifying modifiable risk factors for relapse in patients with schizophrenia in China. Front Psychiatry. 2020;11:574763.
- Fervaha G, Foussias G, Agid O, Remington G. A motivation and functional outcomes in early schizophrenia. Psychiatry Res. 2013;210(2):665-658.
- Novick D, Haro JM, Suarez D, Perez V, Dittmann RW, Haddad PM. Predictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophrenia. Psychiatry Res. 2010;176(2-3):109-113.
- Allen CG, Sugarman MA, Wennerstrom A. Community health workers: A resource to support antipsychotic medication adherence. The Journal of Behavioral Health Services & Research. 2017;44:341-346.
- Lacro JP, Dunn LB, Dolder CR, Jeste DV. Prevalence of risk factors for medication nonadherence in patients with schizophrenia: A comprehensive review of recent literature. The J Clin Psychia. 2002;63(10):15489.
- Xiao J, Mi W, Li L, Shi Y, Zhang H. High relapse rate and poor medication adherence in the Chinese population with schizophrenia: Results from an observational survey in the People’s Republic of China. Neuropsychiatr Dis Treat. 2015:1161-1167.
- Meltzer HY, Gadaleta E. Contrasting typical and atypical antipsychotic drugs. Focus. 2021;19(1):3-13.
- Honer WG. Better evidence for pharmacological maintenance treatment in nonaffective psychoses: Implications for relapse prevention. Am J Psychiatry. 2021;178(5):369-371.
- Tandon R, Jibson MD. Comparing efficacy of first-line atypical antipsychotics: No evidence of differential efficacy between risperidone, olanzapine, quetiapine, ziprasidone, and aripiprazole. Int J Psychiatry Clin Pract. 2005;9(3):204-212.
- Hirschfeld RM, Weisler RH, Raines SR, Macfadden W. Quetiapine in the treatment of anxiety in patients with bipolar I or II depression: a secondary analysis from a randomized, double-blind, placebo-controlled study. J Clin Psychia. 2006;67(3):355-362.
- Mouaffak F, Ferreri F, Bourgin-Duchesnay J, Baloche E, Blin O, Vandel P, et al. Dosing antipsychotics in special populations of patients with schizophrenia: Severe psychotic agitation, first psychotic episode and elderly patients. Expert Opin Pharmacother. 2021;22(18):2507-19.
- McIntyre A, Gendron A, McIntyre A. Quetiapine augmentation of SSRIs/SNRIs in major depression with anxiety. In Poster presented at the American Psychiatric Association 159th Annual Meeting, Toronto, Canada. 2006.
- Saha KB, Bo L, Zhao S, Xia J, Sampson S, Zaman RU. Chlorpromazine versus atypical antipsychotic drugs for schizophrenia. Cochrane Database Syst Rev. 2016(4).
- Copolov DL, Link CG, Kowalcyk B. A multicentre, double-blind, randomized comparison of quetiapine (ICI 204,636,‘Seroquel’) and haloperidol in schizophrenia. Psychol Med. 2000;30(1):95-105.
- Wu H, Siafis S, Hamza T, Schneider-Thoma J, Davis JM, Salanti G, et al. Antipsychotic-induced weight gain: Dose-response meta-analysis of randomized controlled trials. Schizophr Bull. 2022;48(3):643-54.
- Karlin DM, Nelson LA, Campbell AR. Dexmedetomidine sublingual film: A new treatment to reduce agitation in schizophrenia and bipolar disorders. Ann. Pharmacother. 2024;58(1):54-64.
- Gasquet I, Haro JM, Tcherny-Lessenot S, Chartier F, Lépine JP. Remission in the outpatient care of schizophrenia: 3-year results from the Schizophrenia Outpatients Health Outcomes (SOHO) study in France. Eur Psychiatry. 2008;23(7):491-496.
- Schooler NR. Relapse and rehospitalization: Comparing oral and depot antipsychotics. J Clin Psychia. 2003;64:14-17.
[Google Scholar] [PubMed]
- Gaebel W, Schreiner A, Bergmans P, De Arce R, Rouillon F, Cordes J, et al. Relapse prevention in schizophrenia and schizoaffective disorder with risperidone long-acting injectable vs. quetiapine: Results of a long-term, open-label, randomized clinical trial. Neuropsychopharmacology. 2010;35(12):2367-2377.
[Crossref] [Google Scholar] [PubMed]
- Bogers JP, Hambarian G, Michiels M, Vermeulen J, de Haan L. Risk factors for psychotic relapse after dose reduction or discontinuation of antipsychotics in patients with chronic schizophrenia: A systematic review and meta-analysis. Schizophrenia Bulletin Open. 2020;1(1):sgaa002.
- Bhargava S, Bairwa K, Motwani Y. Neuroleptic malignant syndrome after abrupt discontinuation of neuroleptic and anticholinergic drugs. Ind Psychiatry J. 2023;32(Suppl 1):S277-S278.
[Crossref] [Google Scholar] [PubMed]
- Brandt L, Schneider-Thoma J, Siafis S, Efthimiou O, Bermpohl F, Loncar L, et al. Adverse events after antipsychotic discontinuation: An individual participant data meta-analysis. Lancet Psychiatry. 2022;9(3):232-242.
[Crossref] [Google Scholar] [PubMed]
- Lian L, Kim DD, Procyshyn RM, Cázares D, Honer WG, Barr AM. Long-acting injectable antipsychotics for early psychosis: A comprehensive systematic review. PLoS One. 2022;17(4):e0267808.
[Crossref] [Google Scholar] [PubMed]
- American Psychiatric Association. The American Psychiatric Association practice guideline for the treatment of patients with schizophrenia. American Psychiatric Pub; 2020.
- Bighelli I, Rodolico A, García-Mieres H, Pitschel-Walz G, Hansen WP, Schneider-Thoma J, et al. Psychosocial and psychological interventions for relapse prevention in schizophrenia: A systematic review and network meta-analysis. Lancet Psychiatry. 2021;8(11):969-980.
[Crossref] [Google Scholar] [PubMed]
- National Institute for Clinical Excellence. Schizophrenia: Core interventions in the treatment and management of schizophrenia in primary and secondary care. Clinical guideline. 2002.
- Jørgensen KT, Bøg M, Kabra M, Simonsen J, Adair M, Jönsson L. Predicting time to relapse in patients with schizophrenia according to patients’ relapse history: A historical cohort study using real-world data in Sweden. BMC psychiatry. 2021; 21:1-12.
- Garety PA, Fowler DG, Freeman D, Bebbington P, Dunn G, Kuipers E. Cognitive-behavioural therapy and family intervention for relapse prevention and symptom reduction in psychosis: Randomised controlled trial. Br J Psychiatry. 2008;192(6):412-423.
[Crossref] [Google Scholar] [PubMed]
- Pitschel-Walz G, Leucht S, Bäuml J, Kissling W, Engel RR. The effect of family interventions on relapse and rehospitalization in schizophrenia—a meta-analysis. Schizophr Bull. 2001;27(1):73-92.
[Crossref] [Google Scholar] [PubMed]
- Giron M, Fernandez-Yanez A, Mana-Alvarenga S, Molina-Habas A, Nolasco A, Gomez-Beneyto M. Efficacy and effectiveness of individual family intervention on social and clinical functioning and family burden in severe schizophrenia: A 2-year randomized controlled study. Psychol Med. 2010;40(1):73-84.
[Crossref] [Google Scholar] [PubMed]
- Rummel-Kluge C, Kissling W. Psychoeducation for patients with schizophrenia and their families. Expert Rev Neurother. 2008;8(7):1067-1077.
[Crossref] [Google Scholar] [PubMed]
- Magliano L, Fiorillo A. Psychoeducational family interventions for schizophrenia in the last decade: From explanatory to pragmatic trials. Epidemiol Psychiatr Sci. 2007;16(1):22-34.
[Crossref] [Google Scholar] [PubMed]
- Schooler NR. Relapse prevention and recovery in the treatment of schizophrenia. J Clin Psychiatry. 2006;67:19.
[Google Scholar] [PubMed]
- Spaniel F, Bakstein E, Anyz J, Hlinka J, Sieger T, Hrdlicka J, et al. Relapse in schizophrenia: Definitively not a bolt from the blue. Neurosci Lett. 2018;669:68-74.
[Google Scholar] [Crossref] [PubMed]
- Herz MI, Lamberti JS, Mintz J, Scott R, O'Dell SP, McCartan L, et al. A program for relapse prevention in schizophrenia: A controlled study. Arch Gen Psychiatry. 2000;57(3):277-283.
[Google Scholar] [PubMed]
Citation: Ezeani EI, Chukwuma OV, Arubuolawe OO, Afolabi VI, Igo JO, Mbah LA, et al (2024) Multiple Relapse in Schizophrenia, Possible Causes and Prevention. J Psychiatry. 27:674.
Copyright: copy&; 2024 Ezeani EI, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

