Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
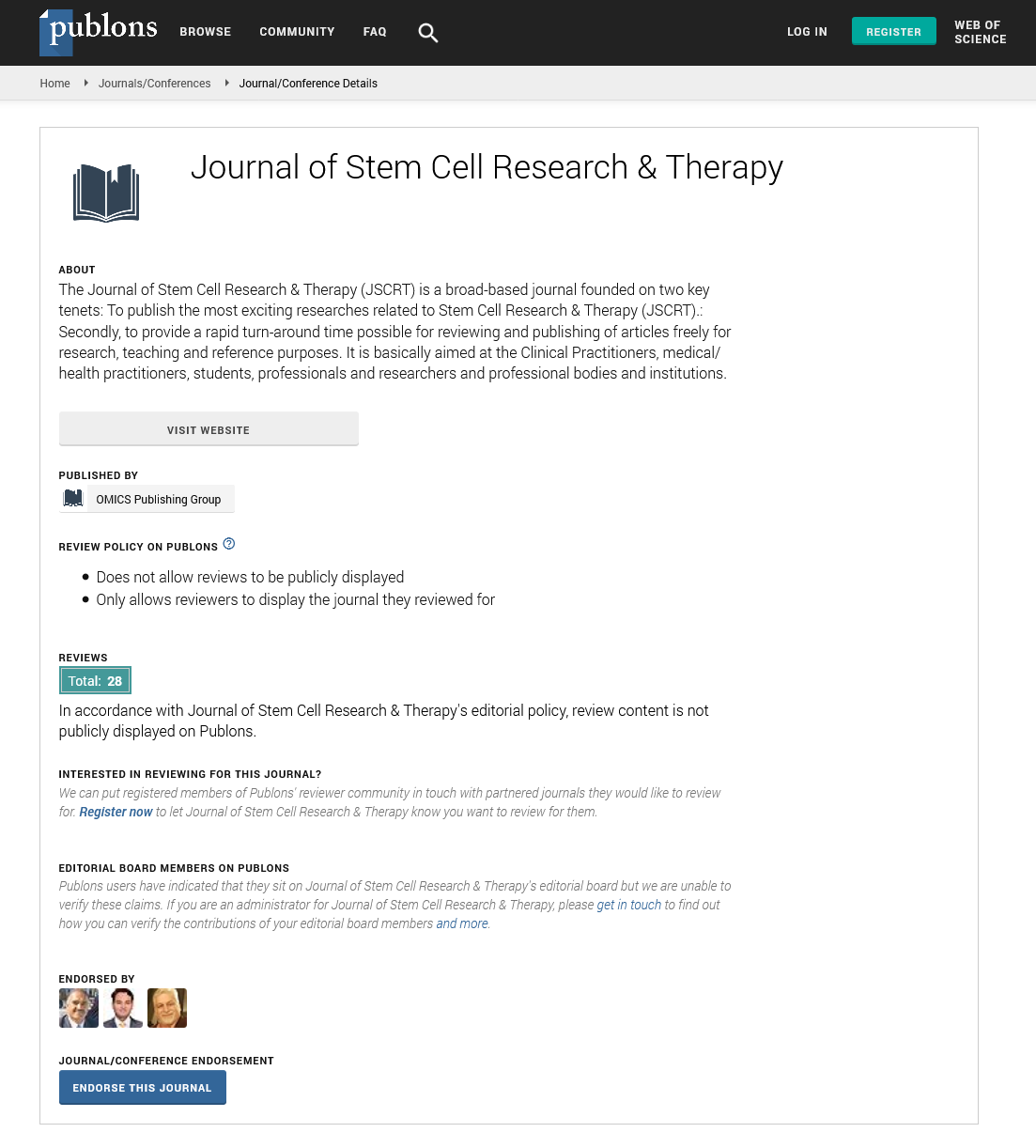
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2021) Volume 11, Issue 12
Minipigs as a Preclinical Model for Autologous Porcine Bone Marrow Mesenchymal Cell Regeneration
Cecilie Gudveig Gjerde*Published: 26-Dec-2021
Introduction
Regeneration of atrophied alveolar bone prior to insertion of dental implants is a major challenge for oral and maxillofacial surgery. It has been reported that Bone Marrow (BM) derived Mesenchymal Stromal Cells (MSC) retain therapeutic potential for bone regeneration. In the present study, a preclinical mini-pig model simulating the clinical setting was established in order to evaluate the efficacy of autologous MSC for mandible regeneration. Under general anaesthesia, BM aspirates were collected from tibia of mini-pigs (n = 5) and MSC were isolated, characterized and expanded. At the same time, a narrow alveolar ridge was simultaneously created by bilateral extraction of two premolar teeth and removal of the buccal bone in order to simulate the pathological situation in humans. After ex vivo expansion, cells were delivered fresh to the surgical operating room and seeded on Biphasic Calcium Phosphate (BCP) granules for 1 hour followed by implantation into the simulated alveolar defects in one pig. The surgical defects were closed with sutures and left to heal for eight weeks. A bone biopsy was taken and dental implants were placed in the newly formed bone.
Extensive bone loss due to trauma, inflammation or ablative tumour surgery may result in large bone defects, and reconstruction of these defects remains a major clinical challenge. In the mandible, the volume of the alveolar ridge may also be reduced to a varying degree as a result of congenital malformations, loss of teeth or aging.
Replacement of missing teeth with dental implants is a well-established clinical procedure, but requires an alveolar ridge with a minimum bone width of 6 mm. If the width is inadequate, augmentation of the existing bone volume is required.
Discussion
A common approach today to regenerate an alveolar bone involves the application of a barrier membrane to establish a suitable environment for ontogenesis, by excluding connective tissue cells from the bone defect. The barrier membrane maintains locally applied cells close to the bone defect, favouring contribution(s) from adjacent bone osteoprogenitor cells to improve bone healing. Other current therapeutic approaches include the application of bone grafts (autologous, allogeneic, xenogenic), as well as a technique known as segmental bone transport. In particular, autologous bone grafts have become the "gold standard" for bone augmentation since these grafts are osteoconductive, osteoinductive and contain osteogenic cells. However, there are drawbacks to this approaches it often requires a period of anaesthesia and high number of personnel, resulting in increased costs for the surgical procedures. Additionally, the quantity of the graft is often inadequate. Donor site morbidity is also a concern, with potentially serious sequela such as infections and nerve damage. The risks of bone graft failure, usually attributable to incomplete integration or infection, increases with defect size.
The search for alternative treatments of bone defects has led to the introduction of Tissue Engineering (TE) strategy combining biomaterials and Mesenchymal Stromal Cells (MSC), as demonstrated in preclinical and early clinical studies. Depending on the clinical indications, different biomaterials may be used as scaffolds for MSC in bone tissue engineering. Moreover, synthetic bone substitutes, such as Hydroxy Apatite (HA) and beta-Tricalcium Phosphate (β-TCP) are safe, bioactive and osteoconductive [9]. Several studies have demonstrated the bioactivity of ceramic materials combining HA and Biphasic Calcium Phosphate (BCP) in varying proportions. Furthermore, the feasibility and efficacy of combining BCP materials and MSC for bone regeneration have been demonstrated in experimental animal models. However, for a solid translation of bone tissue engineering from bench to bedside, preclinical testing in large animals is mandatory to ensure suitability and safety for patients. Porcine models are widely applied in regenerative medicine studies, using cells harvested from numerous sites, including bone marrow and adipose tissue. Since mini-pigs have genetic characteristics, gross anatomy, physiology, bone healing patterns and chewing apparatus comparable to those of humans, they are increasingly being used to study oral, maxillary and dental procedures. We therefore designed a study in mini-pigs to simulate the clinical conditions for the reconstruction of resorbed alveolar bone by using autologous culture expanded MSC associated to BCP granules and covered with a titanium reinforced Polytetrafluoroethylene (PTFE) barrier membrane. This study aimed at optimizing protocols for ex-vivo autologous MSC handling, testing surgical procedures and evaluating efficacy of this bone tissue engineering approach in a large animal model using critical sized defects in the alveolar bone.