PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
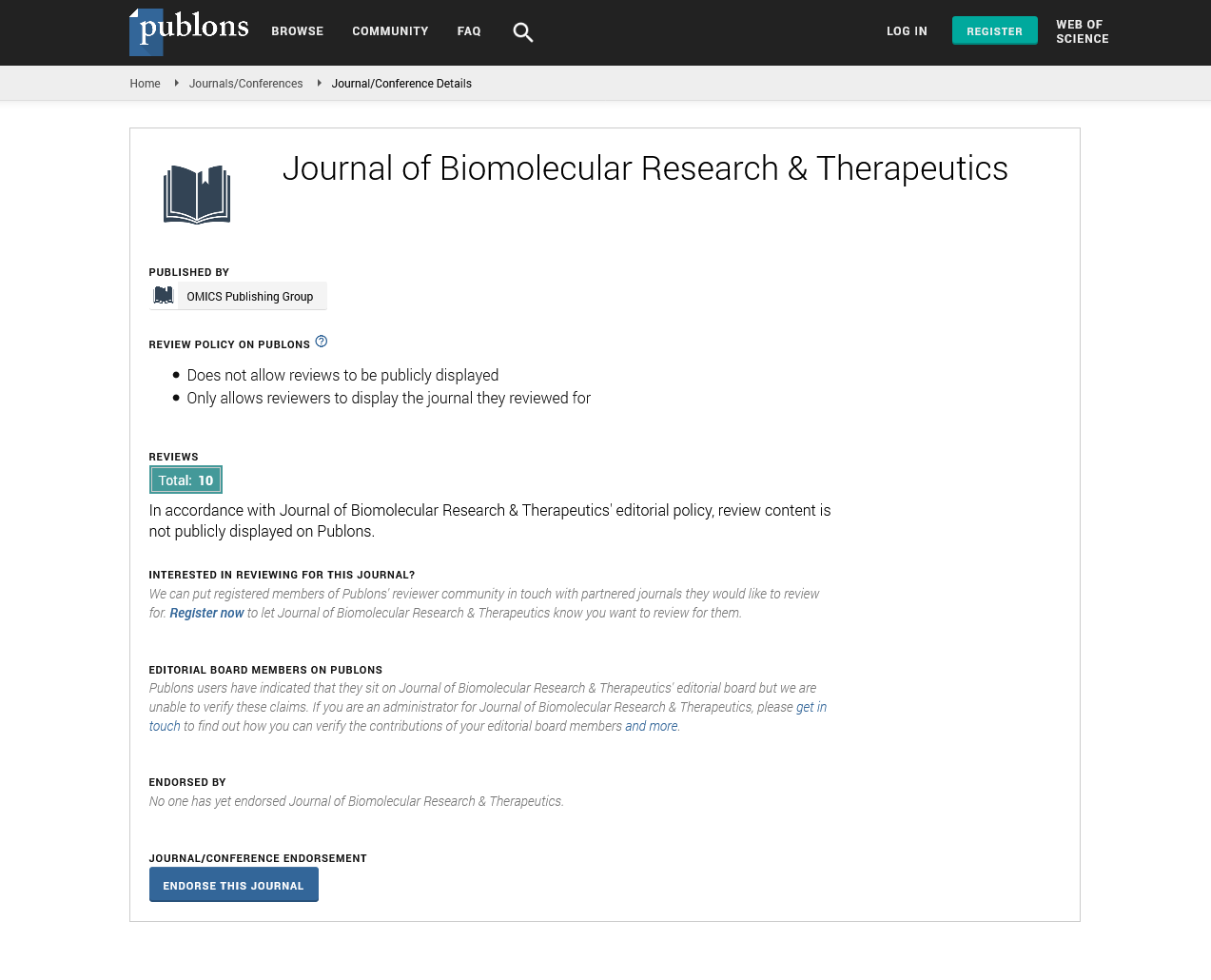
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2022) Volume 11, Issue 12
Mechanisms and Treatment of Cutaneous Squamous Cell Carcinoma
Sancho Cohol*Received: 25-Nov-2022, Manuscript No. BOM-22-19266; Editor assigned: 28-Nov-2022, Pre QC No. BOM-22-19266 (PQ); Reviewed: 15-Dec-2022, QC No. BOM-22-19266; Revised: 22-Dec-2022, Manuscript No. BOM-22-19266 (R); Published: 29-Dec-2022, DOI: 10.35248/2167-7956.22.11.247
Description
Cutaneous Squamous Cell Carcinoma (CSCC) is the second most common cancer in humans and its prevalence is increasing. Although CSCC is usually benign clinically it can be both locally invasive and metastatic. In recent decades, the signaling pathways involved in CSCC formation have given rise to targetable molecules. Furthermore the high mutational burden and higher risk of CSCC in Immunocompromised individuals were part of the rational for developing the immunotherapy for CSCC that has altered the therapeutic landscape. The molecular underpinnings of CSCC and current biology-based techniques of targeted treatments and immune checkpoint inhibitors Cutaneous Squamous Cell Carcinoma (CSCC) is the second most common type of cancer in humans with an estimated 1 million cases per year.
The malignant growth of epidermal keratinocytes causes CSCC. Its development is threatened by environmental and constitutional risks. In terms of the former, older age, male fair skin, immunosuppression and a history of Actinic keratosis (AK) are all known risk factors. The most important and well-known environmental component associated with CSCC is chronic sun exposure. Surgery is the mainstay of CSCC treatment while radiotherapy is frequently used as well. However, systemic therapies may benefit a fraction of patients with locally progressed and metastatic CSCC. Current cancer therapy efforts point to the disruption of signaling pathways involved in its etiology. Inhibitors were among the first systemic treatments investigated for the treatment of CSCC. Some studies suggested that it could be involved in the formation of CSCC and given the limited efficacy of CSCC medications this seemed like a natural and attractive avenue to pursue. Other malignancies were explored with inhibitors. Tumor cells produce neoantigens, which the immune system recognizes and targets. When a T-cell detects an antigen produced by the Human Leukocyte Antigen (HLA) complex in a tumor cell, co-receptors operate as immune activators and inhibitors. Several medications have been developed to treat CSCC although the condition may also be caused by drugs. Pharmacologically induced CSCC is caused by molecular pathways and understanding them can help physicians better treat this malignancy. Finally the tumor microenvironment is significant in the carcinogenesis of CSCC and its importance in tumor formation has grown in recent years. Inflammation is a major component of the tumor microenvironment and may operate as a tumor promoter. The absence of an inflammatory response is important in tumor growth. Recent research indicates that the Cancer-Associated Fibroblasts (CAFs) and Tumor-Associated Macrophages (TAMs) are over represented in the CSCC tumor microenvironment.
Tumor stromal cells are involved in tumor invasion, metastasis, tumor progression and treatment response. Tumor cells produce neoantigens, which the immune system recognizes and targets. Co-receptors operate as activators and inhibitors of the immune response. "Immune checkpoint" receptors include inhibitory receptors such as programmed cell death 1 protein and Cytotoxic T-Lymphocyte Antigen 4 (CTLA4). T-cells, B-cells, monocytes, natural killer cells and dendritic cells all express PD-1 an inhibitor co-receptor. Targeting immunological checkpoint proteins with monoclonal antibodies has resulted in a therapeutic advantage in cancer and has radically improved the prospects for the treatment of several cancers, such as melanoma. A tumor is made up of both neoplastic cells and the tumor microenvironment. The tumor microenvironment not just the neoplastic cells can also be manipulated to kill them.
Citation: Cohol S (2022) Mechanisms and Treatment of Cutaneous Squamous Cell Carcinoma. J Biol Res Ther. 11:247.
Copyright: © 2022 Cohol S. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.