Indexed In
- The Global Impact Factor (GIF)
- CiteFactor
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Virtual Library of Biology (vifabio)
- International committee of medical journals editors (ICMJE)
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2022) Volume 21, Issue 2
Maxillary Obturator in Hemi Maxillectomy Patient: A Case Report
Ishita Dureja*, Ripul Pahwa, Akshay Pahwa and Ritika Satija2Department of Endodontics, SantoshDental College, Ghaziabad, India
Received: 28-Jan-2022, Manuscript No. OHDM-22-15559; Editor assigned: 31-Jan-2022, Pre QC No. OHDM-22-15559 (PQ); Reviewed: 14-Feb-2022, QC No. OHDM-22-15559; Revised: 18-Feb-2022, Manuscript No. OHDM-22-15559 (R); Published: 25-Feb-2022, DOI: 10.35248/2247-2452.22.21.980
Abstract
Defects in the maxillary jaw can be congenital, developmental, acquired, traumatic or surgical involving the oral cavity and related anatomic structure. Absence or loss of some or all of the soft palate and/or hard palate results in insufficient structure or altered function of the remaining tissues. Defects can cause disruption of articulation and airflow during speech production and also nasal reflux during deglutition. Patients after surgical resection have altered anatomy due to scaring, tissue contracture, lack of bony support and tissue edema. These patients have problem of regurgitation of water and food through nose and difficulty in speech. These changes require the fabrication of prosthesis and also sometimes repeated prosthesis adjustments to confirm to the soft tissue changes. To prevent this and to help the patient in deglutition and speech defects must be restored with prosthesis. In such situation an obturator is designed to close the opening between the residual hard and/or soft palate and the pharynx. The prosthesis provided for these patients are called as obturators. An obturator is a prosthesis which is fabricated for the patients with the palatal defects in the form of cleft lip and palate, oroantral fistula or surgical resection after removable of pathology like tumor or cancer. This case report will highlight on the Prosthetic Rehabilitation of the maxillary defects and the types of obturators and technique followed in fabrication of an obturator in hemimaxillectomy patient.
Keywords
Definitive prosthesis, Interim prosthesis, Maxillary defects, Maxillary obturator, Speech prosthesis, Surgical obturator.
Introduction
Most common intraoral defects in the maxilla are in the form of an opening into the antrum and nasopharynx. Maxillary defects can be congenital, developmental, acquired, traumatic, or surgical involving the oral cavity an related anatomic structure.
Absence or loss of some or all of the soft palate and/or hard palate results in insufficient structure or altered function of the remaining structure. Defects can cause disruption of articulation and airflow during speech production and nasal reflux during deglutition. Nasal sounds such as “n,” “m,” and “ng” is seen due to the absence of closure of the pharyngeal wall. Patients after surgical resection have altered anatomy due to scaring, tissue contracture, lack of bony support, and tissue edema. Surgical resection can lead to the restricted opening of the jaws and altered range of mandibular movements with fibrosis and trismus. These patients have the problem of regurgitation of water and food through nose. There may be difficulty in speech, deglutition, maintaining oral hygiene, and prosthetic treatment.
To prevent this and to help the patient in deglutition and speech, defects must be restored with prosthesis. In such situations, a prosthesis called as an obturator is designed to close the opening between the residual hard and/or soft palate and pharynx. These changes require the fabrication of prosthesis and sometimes repeated prosthesis adjustments to confirm the soft tissue changes. Obturator is derived from the Latin word “obturate” which means to close or shut off.
Prosthesis facilitates speech, and deglutition by replacing those tissues lost due to the disease process and can, as a result, reduce nasal regurgitation and hypernasal speech, improve articulation, deglutition, and mastication.
Followings are the objectives of maxillary obturator:
1. Restoration of esthetics or cosmetic appearance of the patient.
2. Restoration of function.
3. Protection of tissues.
4. Therapeutic or healing effect.
5. Psychological therapy [1-4].
Ideal Requirements for Maxillary Obtur
1. Help the patient to carry out natural functions such as phonation, deglutition, and mastication.
2. Should exhibit life-like appearance to aid function.
3. Design of the prosthesis should be such that it is easily and swiftly placed and held in position both comfortably and securely.
4. Prosthesis should be durable for a reasonable period of time, retain its polish and finish.
5. Should be easy to clean so as to maintain hygiene.
There are various functions of obturator:
1. To close the defect.
2. For feeding purpose.
3. To keep the wound or defective area clean, thus enhance the healing of traumatic or postsurgical defects.
4. As a stent to hold dressings or packs post surgically.
5. To reduce the possibility of postoperative hemorrhage.
6. Help to reshape and reconstruct the palatal contour and/or soft palate.
7. Improve speech or in some instances, makes speech possible.
8. Help in reducing the flow of exudates, saliva, and fluids from the mouth into the nasopharynx.
9. To improve the esthetics and correct lip and cheek contour.
10. To benefit the morale of the patient with maxillary defects.
11. To improve function when deglutition and mastication are impaired.
Indications
1. To act as a framework over which tissues may be shaped by the surgeon.
2. To serve as a temporary prosthesis during the period of surgical correction.
3. When surgical primary closure is contraindicated.
4. When patient’s age contraindicates surgery.
5. When size and extent of the deformity contraindicates surgery.
6. When local avascular condition of the tissues contraindicates surgery.
7. When a patient is susceptible to the recurrence of original lesion that produced the deformity.
Classification
Mohamed Aramany in 1978 classified obturators for maxillectomy patients who are partially edentulous into seven groups [5]:
a. Class I: Resection or defect is performed along the midline of the maxilla; teeth are maintained on one side of the arch. It is the most frequent maxillary defect.
b. Class II: Defect is unilateral, retaining the anterior teeth on the contralateral side.
c. Class III: Palatal defect occurs in the central portion of the hard palate and may involve part of the soft palate. The surgery does not involve the remaining teeth.
d. Class IV: Defect crosses the midline and involves both sides of the maxilla. There are few teeth remaining which lie in a straight line. This may create a unique design problem similar to the unilateral design of conventional removable partial dentures.
e. Class V: Surgical defect is bilateral and lies posterior to the remaining abutment teeth.
f. Class VI: Defect occurs mostly in trauma and the defect lies anterior to the bilaterally standing abutments. Surgical intervention of anterior midpalatal pathology can cause such type of defects.
g. Class VII: This situation is similar to Kennedy Class II, but the defect is small unilaterally posterior to the standing abutments. This situation usually arises as a result of minor surgery for removal of pathology or can occur as squeal of multiple extractions in the posterior regions (Figure 1).
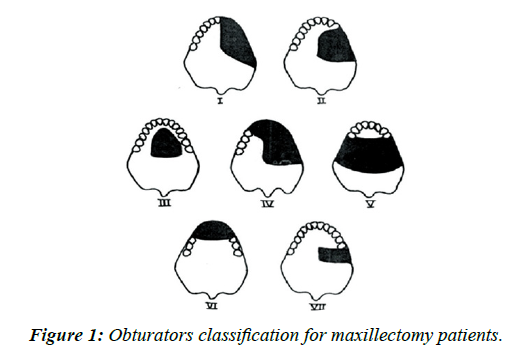
Figure 1: Obturators classification for maxillectomy patients.
Case Presentation
A 36 year old male patient presented to the outdoor of Prosthodontics department, IndraprasthaDental College, Sahibabad, Ghaziabad. The patient had a history of Ameloblastoma in the right maxilla for which he had undergone a hemimaxillectomy type of surgical resection ten years ago.
The patient had an Aramany Class IV defect and was using obturator prosthesis for the last ten years. His chief complaints with the previous obturator were its looseness, foul smell and unaesthetic appearance. The patient was a laborer by profession and medically and physically fit.
On extra oral examination there was a tissue contracture visible on the right side of face (Figures 2 and 3).On intra oral exam it was observed that the left maxillary quadrant was intact with all the teeth present except left upper central and lateral incisor. The mandible had a full component of natural teeth and the oral hygiene was fair. The patient had normal mouth opening and jaw movements. A mature maxillary aramany Class IV defect on the right side was present with the loss of all teeth from left upper lateral incisor to right upper third molar. The defect had a communication with the nasal cavity and mild lateral undercuts were present (Figure 4). The previous obturator was an all acrylic ill-fitting removable prosthesis. The support and retention was inadequate but it had stable occlusal contacts with the opposing dentition. The ten years old acrylic denture base showed signs of disintegration such as foul smell, discoloration and staining.
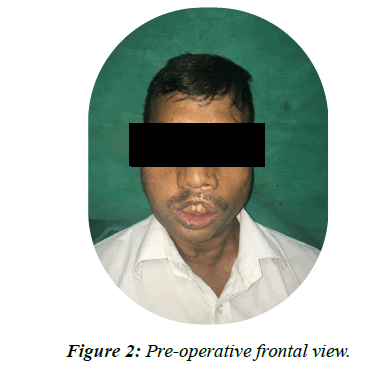
Figure 2: Pre-operative frontal view.
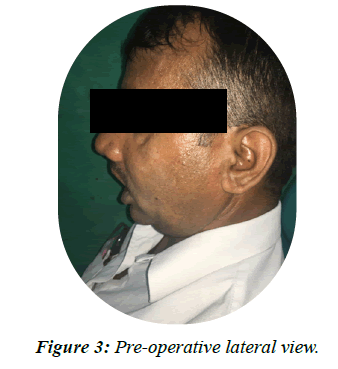
Figure 3: Pre-operative lateral view.

Figure 4: Pre-operative intra oral view.
After thorough evaluation of the patient it was decided that new acrylic obturator prosthesis will be fabricated for him. A cast partial framework and/or implant supported prosthesis were not selected because of financial constraints of the patient.
Technique
Intra oral examination was done. Complete evaluation of soft and hard tissue was done followed by treatment planning [6- 11].
• Stock tray was used for the primary impression. Primary impression was made using irreversible hydrocolloid (alginate) (Figure 5).
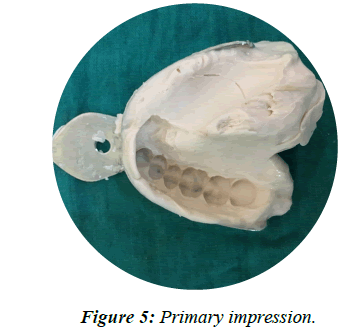
Figure 5: Primary impression.
• Special tray was fabricated on primary cast on the area of defect. The defect was recorded with help of low fusing compound and finalimpression was made with light body addition silicone (Figure 6).
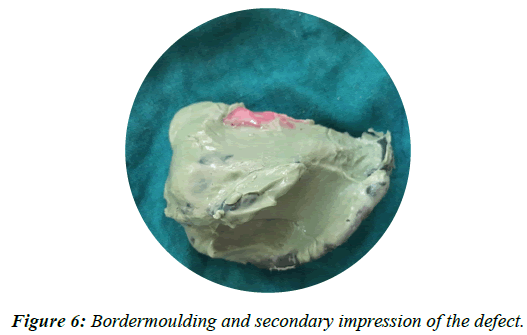
Figure 6: Bordermoulding and secondary impression of the defect.
• Now a pick-up impression of the upper arch with the obturator in situ was taken in a stock tray using irreversible hydrocolloid alginate impression material (Figure 7) and poured in type IV gypsum (Figure 8).
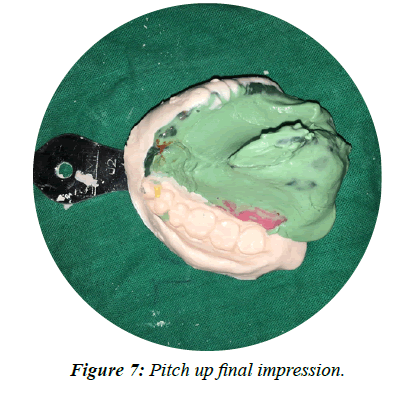
Figure 7: Pitch up final impression.
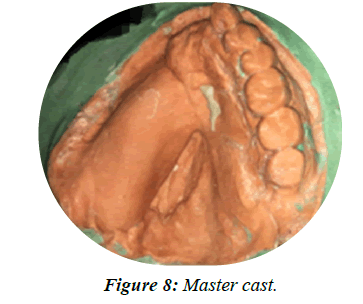
Figure 8: Master cast.
• Lower impression in a stock tray with irreversible hydrocolloid alginate material was taken and poured in type IV gypsum.
• The interocclusal bite record was used to articulate the upper and lower casts.
• Surveying of the upper cast was done on a surveyor to determine the favorable and utilizable tooth and tissue undercuts. A suitable path of insertion was selected for the obturator.
• On the articulated casts, wrought wire clasps on left upper left canine, first and second premolar and second molar were made (Figure 9).

Figure 9: Teeth setting and waxup.
• Anterior teeth must be placed according to smile line but it wasn’t possible in this case because of skipping a separate jaw relation step where smile line is recorded on wax rims so they were placed for denture stability with minimum overjet and overbite. However, incidentally the final outcome was pleasing and the curve of the upper artificial teeth was in harmony with the smile line while the posteriors were placed in maximum intercuspation with the opposing teeth.
• Post dam carving and final wax up with full palatal coverage was done. The palatal contour on the defect side was formed as a continuation of the palatal form on the normal side (Figure 9).
• Laboratory flasking, dewaxing was done (Figure 10).

Figure 10: Flasking and dewaxing.
• Processing, finishing and polishing the new obturator was done, the bulb of the defect was removed and hollowed from inside to reduce the weight of the prosthesis (Figure 11).
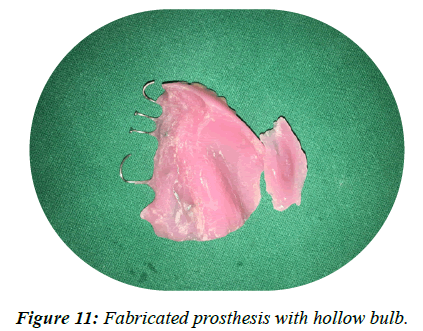
Figure 11: Fabricated prosthesis with hollow bulb.
• During insertion the tissue surface was checked for intimate tissue contact with a pressure indicating paste and occlusal corrections were performed with articulating ribbon. Oral and denture hygiene instructions were given to the patient and called for follow up visit one week after the insertion.
• On the follow up visit the patient presented with no complaints. Oral and denture hygiene instructions were reinforced and the patient was set on a 6 month periodic recall visit for follow up (Figures 12-14).
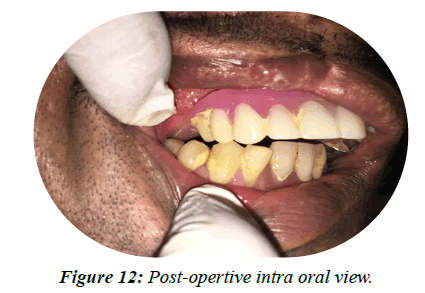
Figure 12: Post-opertive intra oral view.
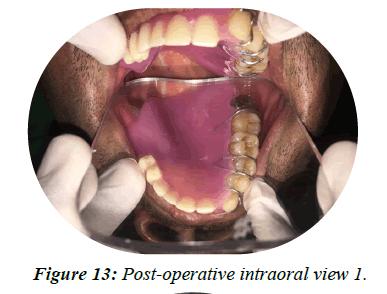
Figure 13: Post-operative intraoral view 1.
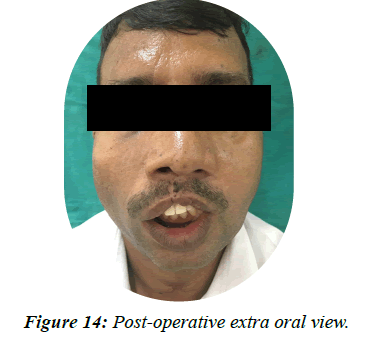
Figure 14: Post-operative extra oral view.
Results and Discussion
Maxillary obturator prosthesis was fabricated for a patient with hemimaxillectomy defect. The patient was a satisfied old obturator wearer but after ten years some tissue changes had occurred making the previous obturator loose. The acrylic had started disintegrating giving foul smell and poor appearance. Financial constraints of the patients limited our treatment options and precluded the selection of cast partial framework or treatment with dental implants so a simple acrylic obturator was planned for the patient.
Conclusion
The pick-up impression was taken in irreversible hydrocolloid alginate impression material in a stock tray which recorded the rest of the arch and the remaining dentition. Bite record in the form on an occlusal wafer was recorded and used for mounting of the casts. These records were sufficient for the construction of a new obturator in the laboratory.
Most of the patients having maxillofacial defects limit their social contact. They also don’t prefer frequent visits to the dentist. Therefore, short and simple procedures should be adopted in treating such patients to save them from multiple unnecessary visits to the clinic as described in this case.
Declaration
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil
Conflict of Interests
There are no conflicts of interest.
REFERENCES
- Omondi BI, Guthua SW, Awange DO, Odhiambo WA. Maxillary obturator prosthesis rehabilitation following maxillectomy for ameloblastoma: Case series of five patients. Int J Prosthodont. 2004; 17(4):464-468.
[Crossref], [GoogleScholar], [Pubmed]
- Mahajan T, Abhishek J, Thanuja R, Jayaprakash K. Prosthetic rehabilitation of maxillectomy patient with immediate and post surgical obturators: A case report. Int J Dent Clin. 2011; 3(1):96-97.
- Irish J, Sandhu N, Simpson C, Wood R, Gilbert R, Gullane P, et al. Quality of life in patirnts with maxillectomy prosthesis. Head Neck. 2009; 1(6): 813-821.
[Crossref], [GoogleScholar], [Pubmed]
- Taira Y, Yanamoto S, Kawasaki G, Yamada S, Atsuta M. A detachable silicone obturator fitted after bilateral maxillectomy: a case report. Int Chin J Dent. 2007; 7:75-77.
- Aramany MA. Basic principles of obturator design for partially edentulous patients. Part I: classification. J Prosthet Dent. 1978; 40(5):554-557.
[Crossref], [GoogleScholar], [Pubmed]
- Dable R. A hollow bulb obturator for maxillary resection in a completely edentulous patient. J Clin Diagn Res. 2011; 5(1):157-162.
- Block MS, Baughman DG. Reconstruction of severe anterior maxillary defects using distraction osteogenesis, bone grafts and implants. J Oral Maxillofac Surg. 2005; 63(3):291-297.
[Crossref], [GoogleScholar], [Pubmed]
- Oh WS, Roumanas E. Dental implant-assisted prosthetic rehabilitation of a patient with a bilateral maxillectomy defect secondary to mucormycosis. J Prosthet Dent. 2006; 96(2):88-95.
[Crossref], [GoogleScholar], [Pubmed]
- Shaker KT. A simplified technique for construction of an interim obturator for a bilateral total maxillectomy defect. Int J Prosthodont. 2000; 13(2):166-168.
[Crossref], [GoogleScholar], [Pubmed]
- Zarb G, Hobkirk J, Eckert S, Jacob R. Prosthodontic treatment for edentulous patients. 13th ed. Canada: Elsevier; 2012.
[GoogleScholar], [Elsevier]
- Raja HZ, Saleem MN. Gaining Retention, support and stability of a maxillary obturator: A case report. J Coll Physicians Surg Pak. 2011; 21:311-314.
[Crossref], [GoogleScholar], [Pubmed]
