Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
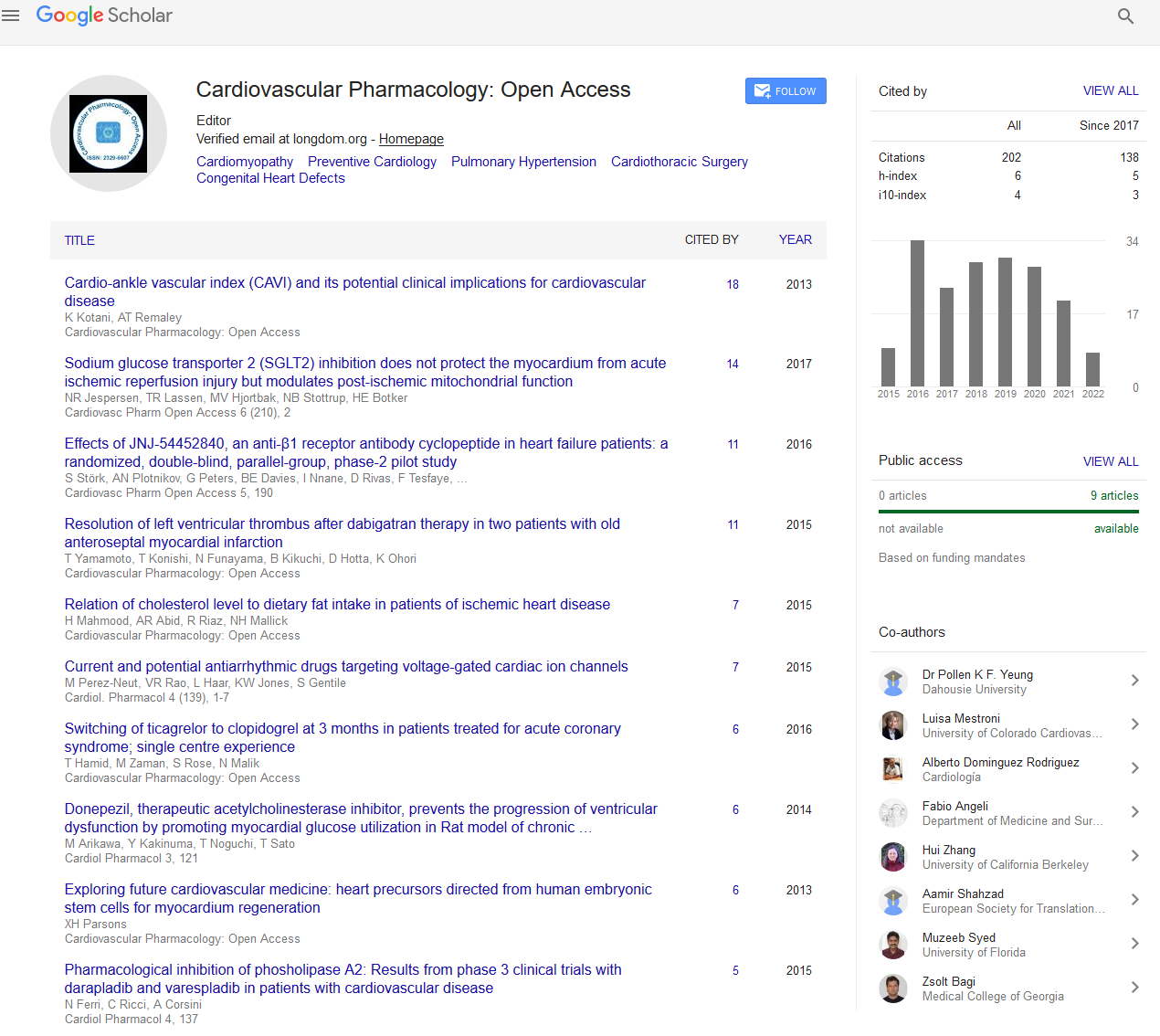
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2023) Volume 12, Issue 1
Maternal Cardiac Arrest and Physiological Changes in Pregnant Woman
Eishin Tanaka*Received: 03-Jan-2023, Manuscript No. CPO-23-20326; Editor assigned: 05-Jan-2023, Pre QC No. CPO-23-20326 (PQ); Reviewed: 19-Jan-2023, QC No. CPO-23-20326; Revised: 27-Jan-2023, Manuscript No. CPO-23-20326 (R); Published: 03-Feb-2023, DOI: 10.35248/2329-6607.23.12.329
Description
The Emergency Department (ED) staff must care for both the mother and the foetus during a maternal cardiac arrest, which is a very difficult and complex duty. Emergency Medical Services (EMS) are a crucial aspect of the treatment procedure since maternal cardiac arrests that occur outside of a hospital have the poorest results. The best care of a maternal cardiac arrest necessitates the involvement of several non-emergency teams and the use of specialist equipment, both of which are beyond the normal emergency department coding protocols.
A perimortem caesarean section team, an aesthetic team, neonatal team, as well as tools for newborn resuscitation. While it is essential, it is sometimes realistically challenging to guarantee that the appropriate personnel and equipment reach the code scene. It is essential, but sometimes realistically challenging, to guarantee that the appropriate personnel and equipment reach at the code scene in a timely way. The management of a maternal cardiac arrest requires education and training; however staff members currently lack the necessary expertise, knowledge, and execution of existing recommendations. Although specialist courses are being developed, they are not yet generally accessible, and current Advanced Cardiovascular Life Support (ACLS) training courses do not typically contain a thorough discussion of maternal resuscitation. According to a United Kingdom database that contains the most population-based information on this particular category, cardiac illness is the leading cause of maternal death. Pregnancy is being postponed until later in life, and more women with complicated health issues are opting to get pregnant. Furthermore, even though these patients are being monitored in high-risk facilities, their homes could be nearer to smaller medical facilities. As a result, any emergency room can care for these individuals when they are dangerously ill.
In the obstetric population, critical incidents can happen at any moment, and emergency medical services may be the first line of defence in such situations. Because any emergency room might possibly receive patients, effective communication between EMS providers and the receiving emergency department is essential.
Maternal physiology: the abcs of cardiac arrest
The physiological changes of pregnancy as they relate to resuscitation must be taken into account for the best management of a cardiac arrest in a pregnant woman. To increase the likelihood of a successful resuscitation, considerable resuscitation alterations must be made to the airway (A), breathing (B).
Airway
All personnel participating in maternal resuscitation should consider pregnant patients to have a difficult airway. Even among pregnant women who are not in custody but are under general anaesthesia, failed intubations happen around 1 in 300 times. Maternal airway-related morbidity and death are a persistent source of worry, which has prompted the creation of specialist maternal airway treatment techniques and guidelines. Hyperemia, hypersecretion, and edema are some of the physiological changes that occur in the upper airway during pregnancy. With repeated airway manipulations, these modifications make the mucosa more brittle and might compromise vision and increase bleeding. Moreover, a smaller endotracheal tube should be used during intubation since a pregnant woman's airway is smaller.
Breathing
Rapid desaturation is riskier when a woman is pregnant. The fundamental physiological cause of the fast desaturation seen during pregnancy is a decreased oxygen reserve. Pregnancy causes an increase in oxygen consumption and a decrease in functional residual capacity, which results in a reduced oxygen reserve. Moreover, there is more intrapulmonary shunting during pregnancy, hence the patient will not tolerate ventilation- perfusion mismatch well. As a result, oxygenation in the pregnant patient during a cardiac arrest should be maximized, especially prior to intubation attempts. However, the resuscitation team should also be aware of the risk of uterine vasoconstriction and foetal hypoxemia that can occur with maternal respiratory alkalosis as a result of excessive ventilation.
Citation: Tanaka E (2023) Maternal Cardiac Arrest and Physiological Changes in Pregnant Woman. Cardiovasc Pharm. 12:329.
Copyright: © 2023 Tanaka E. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.