Indexed In
- The Global Impact Factor (GIF)
- CiteFactor
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Virtual Library of Biology (vifabio)
- International committee of medical journals editors (ICMJE)
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 22, Issue 1
Management of Inadequate Attached Gingiva and Vestibular Depth by Combination of Free Mucosal Graft and Modified Apically Repositioned Flap Surgery: A Case Series with 3 Years Follow Up
Navneet Sheokand1*, Mohinder Panwar1, Manab Kosala1, Oliver Jacob2, Sumidha Bansal3, Vishvnathe Udayshankar4 and Lalit Janjani52Department of Periodontics, Indian Naval Hospital Ship Ashwini, Visakhapatnam, India
3Department of Periodontics, Sudha Rustagi College of Dental Sciences and Research Faridabad, Haryana, India
4Department of Dental Surgery, Madras Regimental Centre Wellington, Tamil Nadu, India
5Department of Dental Surgery, Air Force Dental Centre, New Delhi, India
Received: 05-Dec-2022, Manuscript No. OHDM-22-19006; Editor assigned: 09-Dec-2022, Pre QC No. OHDM-22-19006 (PQ); Reviewed: 29-Dec-2022, QC No. OHDM-22-19006; Revised: 06-Jan-2023, Manuscript No. OHDM-22-19006 (R); Published: 16-Jan-2023, DOI: 10.35248/2247-2452.23.22.1036
Abstract
Introduction: Attached gingiva plays very important role in maintaining long term periodontal health in relation to teeth. Although literature is divided on the issue of minimum requirement of attached gingiva in relation to a tooth, Lang and Loe in 1972 mentioned that 2 mm keratinized gingiva out of which 1 mm is attached is considered adequate. There are various surgical modalities to increase amount of keratinized gingiva with MARF being the latest addition.
Objectives: To evaluate the combined effect of Free Mucosal Graft (FMG) and Modified Apically Repositioned Flap (MARF) Surgery in cases with inadequate keratinized gingiva, gingival recession and shallow vestibule.
Methodology: 10 Patients with Millers Class III and IV recession, inadequate width of keratinized gingiva and shallow vestibule were included in the study. 4 parameters were recorded at baseline and 6 months i.e. Width of keratinized gingiva, Width of attached gingiva, Vestibular depth and gingival recession.
Summary of results: Result showed significant difference in width of keratinized gingiva, vestibular depth and coverage of gingival recession. Study showed mean change of 3.0 ± 0.57 mm (p<0.01) in Width of Attached Gingiva, 3.5 ± 0.67 mm (p<0.01) in Vestibular Depth.
Conclusions: Present study demonstrated successful management of inadequate attached gingiva and shallow vestibule by combining two surgical modalities i.e. FMG and MARF
Keywords
Free mucosal graft, Modified apically repositioned flap surgery, Gingival recession
INTRODUCTION
Attached gingiva is the portion of gingiva that extends between the Mucogingival Junction (MGJ) and free gingival groove [1]. This provides protection for periodontium and helps in maintaining the gingival margin at a stable position. Attached gingiva also minimizes the effect of functional forces which are applied by muscle fibres onto gingival tissues. Therefore, it plays a significant role in preserving the health of gingiva [2].
The Attached Gingiva (AG) is that portion of gingiva that extends from the base of the gingival crevice to mucogingival junction. According to glossary of periodontal terms, AG is firm, resilient and tightly bound to underlying periosteum of alveolar bone through connective tissue. An adequate zone of AG is essential to maintain optimal health of periodontium. An inadequate width of AG might facilitate sub-gingival plaque deposition resulting from movability of marginal gingival pull [3,4]. A variety of surgical techniques has been introduced to increase the width of AG. The most commonly documented techniques are augmentation using free gingival grafts, connective tissue gingival grafts and apically repositioned flap [5-7]. Though these techniques were predictable and successful, they were either technique sensitive or involved a second surgical site for procurement of donor tissue [8]. To overcome this, a modification in apically repositioned flap was given by Carnio and Miller in 1999 [9]. In 2006 Carnio and Camargo, described a variation of Modified Apically Repositioned Flap (MARF). The advantages of the variation of MARF technique is its simplicity as it involves only a single horizontal bevelled incision in the recipient site. Literature search revealed very less published research to evaluate the outcomes of this MARF technique [9-13]. Whereas studies combining MARF and CAF are even less. The present study is done to evaluate whether MARF and FMG predictably increases the width of AG and vestibular depth and whether results achieved are stable over a period of over 3 years.
Materials and Methods
Patients for the study were recruited from a tertiary care hospital and individuals were informed about the purpose of the study, the surgical technique and a written informed consent was obtained. A total of 10 individuals were selected based on inclusion and exclusion criteria. Patients age ranged from 18 to 50 years (6 individuals were males and 4 individuals were female). Satisfactory level of plaque control was achieved thorough oral prophylaxis and oral hygiene instructions. The patients were recalled after 4 weeks to assess their compliance with plaque control. Plaque index was used to measure oral hygiene maintenance. Parameters measured at baseline were: PPD, vestibular depth and width of AG (Figure 1). Surgical technique Local anaesthesia was achieved by infiltration technique using lidocaine 1:200000 solution. Following local anaesthesia, a bevelled horizontal incision was made with a #15 blade, from mucogingival junction as there was no attached gingiva. Carefully a split thickness flap was elevated and was extended in the apical direction needed. The flap was displaced apically and secured to the periosteum with simple interrupted resorbable sutures (Figure 2). FMG was harvested from the palatal donor site and sutured carefully at the prepared recipient site (Figure 3). Gentle digital pressure was applied to the surgical area for 3-5 minutes to maintain the FMG in close contact with the underlying periosteum. The periodontal dressing was applied for 2 weeks. Patients were instructed not to brush or disturb the surgical site till suture removal. They were also advised to use 0.12% chlorhexidine rinse for 4 weeks. The dressing and sutures were removed at 2 weeks postoperatively. The surgical site was thoroughly irrigated with saline and healing was assessed. Follow up was done at 3 months and 1 year month and 3 years postoperatively (Figures 4 and 5) (Table 1). On each follow up visits, the periodontal parameters were measured again and tabulated against the baseline measurements.
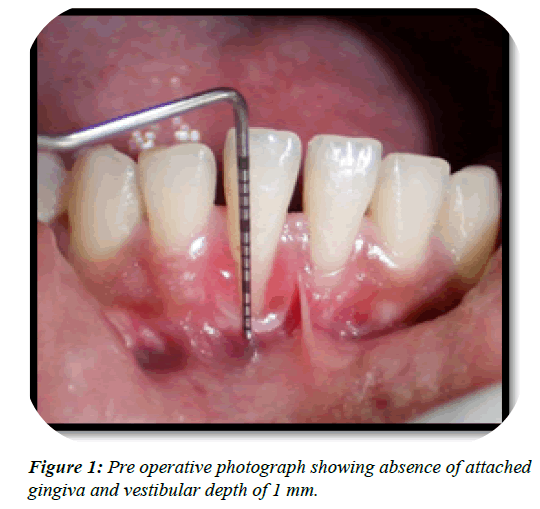
Figure 1: Pre operative photograph showing absence of attached gingiva and vestibular depth of 1 mm.
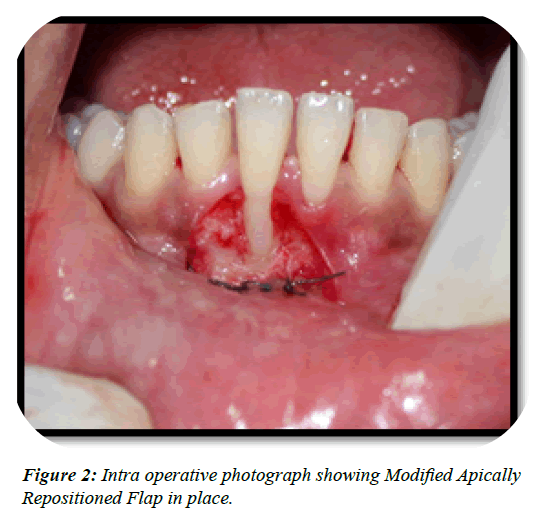
Figure 2: Intra operative photograph showing Modified Apically Repositioned Flap in place.
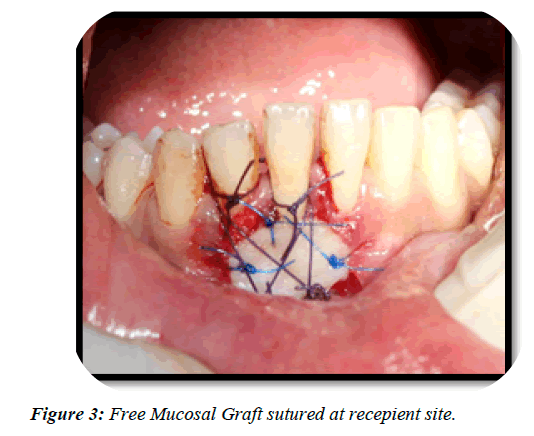
Figure 3: Free Mucosal Graft sutured at recepient site.
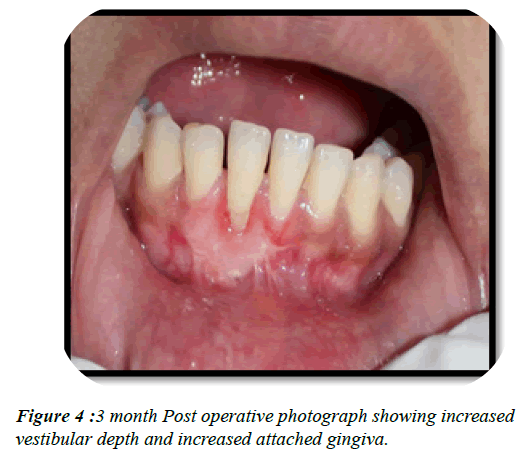
Figure 4: 3 month Post operative photograph showing increased vestibular depth and increased attached gingiva.
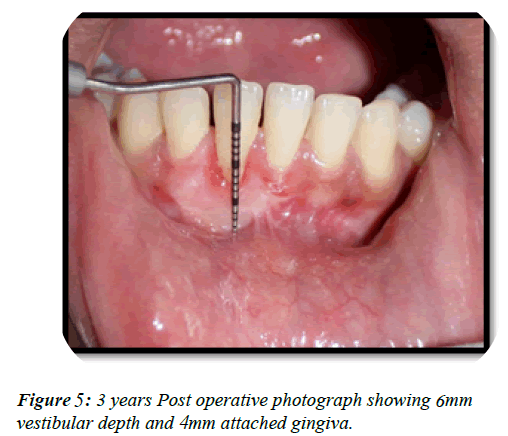
Figure 5: 3 years Post operative photograph showing mm vestibular depth and mm attached gingiva.
| AG | Mean ± SD | Mean difference | P value |
|---|---|---|---|
| Baseline | 0.50 ± 0.000 | ||
| 3 Months | 3.50 ± 0.570 | 3.00 ± 0.570 | <0.001* |
| 3 Years | 3.45 ± 0.570 | 0.05 ± 0.00 | NS |
Note: *Statistically significant using Wilcoxon signed rank test. AG: Attached gingiva; NA: Not available; SD: Standard deviation
Table 1: Comparison of the width of attached gingiva at different time intervals.
Results
The mean PPD measurement of individuals was 1 mm at baseline. At the 3rd month postoperative, the mean pocket depth was 1 mm and the same was maintained at 1 and 3 year postoperatively. Comparing the width of AG at baseline, 3rd month and 3 year (0.50 ± 0, 3.50 ± 0.571 and 3.45 ± 0.571) mm, the mean difference was 3.00 mm and was statistically significant (P<0.001). Comparing the width of AG at 3rd month and 3rd year (3.50 ± 0.571 and 3.45 ± 0.671) mm, the mean difference was 0.05 mm and was not statistically significant (Wilcoxon signed rank test). Comparing the vestibular depth at baseline, 3rd month and 3 year (1.00 ± 0, 4.50 ± 0.671 and 4.50 ± 0.671) mm, the mean difference was 3.50 mm and was statistically significant (P<0.001). Comparing the width of AG at 3rd month and 3rd year (4.50 ± 0.571 and 4.50 ± 0.671) mm, the mean difference was 0.00 mm and was not statistically significant (Wilcoxon signed rank test).
Discussion
As suggested by Bowers in 1963 and Ainamo and Löe in 1996 that the distance between mucogingival junction and projection on the external surface of the bottom of sulcus is the normal width of AG in clinical measurements [1,14]. Lang and Löe in 1972 in an effort to determine the adequate amount of AG studied the relationship between the inflammation and gingival width. Inflammation and exudates were present in 100% of teeth with of gingival health, for the prevention of marginal gingival pull and gingival recession and also to prevent sub- gingival plaque formation. It also aids for the unaltered levels of the connective tissue attachment thereby facilitating good oral hygiene measures [15-18]. Friedman et al. in 1993 stated that sub-gingival plaque formation is facilitated by an inadequate width of AG which is due to the improper pocket closure which results from the movability of the marginal tissue [2]. From this, it is inferred that minimum of 2 mm of KG l tissue is necessary to maintain good gingival health. Increase in width of AG can be accomplished by numerous techniques such as free gingival graft, [5] connective tissue graft, [6] and apically repositioned flap [7]. Though these techniques have been used widely since introduction, they are technique sensitive and requires second surgical site for donor tissue and might be time consuming [8]. To overcome this, Carnio and Miller in 1999 described the MARF. This technique was very similar to apically repositioned flap except the marginal tissue was left intact preventing recession, but the disadvantage was the vertical incision that extended till the vestibular mucosa resulted in excessive bleeding. Since it has to extend to the vestibular depth, it was contraindicated in premolar and molar to prevent damage to the mental foramen [9]. Taking this into consideration, Carnio and Camargo in 2006 described a variation of the MARF. The variant of MARF uses only a single horizontal incision and no vertical releasing incisions to achieve flap mobilization [10]. AG. Carnio et al. in 2015 published the randomized study compared the Free Gingival Graft (FGG) and the MARF in increasing the zone of AG in contralateral sides of 15 patients 1 year post treatment. There was an increase in keratinized tissue and AG in both groups but the MARF surgical time was approximately half as long as that of the FGG. They concluded that both techniques are viable; however, the main advantages of the MARF were decreased surgical time and less postoperative discomfort [13]. According to Karring et al., the origin of the granulation cells that migrate over the wound determines the nature of the new tissues that develop over the exposed periosteum. These cells migrate from the periosteal connective tissue, adjacent gingival and alveolar mucosa and periodontal ligament bone marrow spaces [19,21]. According to Carnio and Camargo, the surgical wound created by MARF is surrounded completely by keratinized tissue. This prevents migration of non-keratinized epithelial cells from the oral mucosa proliferating onto the surgical area [10]. The main advantages of MARF in combination with FMG is that it increases width of attached gingiva as well as vestibular depth. Current study shows long term results of combination of two techniques which are not reported much in literature. Using this combination in Miller’s Class III and Class IV recession can give better and predictable results.
Conclusion
This combination of two techniques offers good results in increasing vestibular depth as well as width of attached gingiva in single attempt. The predictable increase in the apicocoronal gingival dimension by combination of MARF and FMG with stable results over 3 years offers considerable advantage over other mucogingival surgical techniques. Hence this surgical approach should definitely be used for long and sustainable results.
References
- Swarna C, Govada S, Susmitha K, Sowjanya C. Increasing the width of attached gingiva by using modified apically repositioned flap–a case series. J Indian Soc Periodontol. 2019;23(2):172.
[Crossref] [Google Scholar] [PubMed]
- Carnio J, Camargo PM, Passanezi E. Increasing the apico-coronal dimension of attached gingiva using the modified apically repositioned flap technique: A case series with a 6-month follow-up. J Periodontol. 2007;78(9):1825-1830.
[Crossref] [Google Scholar] [PubMed]
- Loe H, Ainamo J. Anatomical characteristics of gingivae-a clinical and microscopic study of free and attached gingivae. J Periodontol. 1966;37:5-13.
[Crossref] [Google Scholar] [PubMed]
- Friedman MT, Barber PM, Mordan NJ, Newman HN. The “plaque-free zone” in health and disease: a scanning electron microscope study. J Periodontol. 1992;63(11):890-896.
[Crossref] [Google Scholar] [PubMed]
- Bjorn H. Free transplantation of gingival propria.Odontol Revy.1963.
- Edel A. Clinical evaluation of free connective tissue grafts used to increase the width of keratinised gingiva. J Clin Periodontol. 1974;1(4):185-196.
- Friedman N. Mucogingival surgery: The apically repositioned flap. J Periodontol.1962;33(4):328-340.
- MILLER Jr PD. Root coverage grafting for regeneration and aesthetics. Periodontol 2000. 1993;1(1):118-127.
[Crossref] [Google Scholar] [PubMed]
- Carnio J, Miller Jr PD. Increasing the amount of attached gingiva using a modified apically repositioned flap. J Periodontol. 1999;70(9):1110-1117.
[Crossref] [Google Scholar] [PubMed]
- Carnio J, Camargo PM. The modified apically repositioned flap to increase the dimensions of attached gingiva: the single incision technique for multiple adjacent teeth. Int J Periodontics Restorative Dent. 2006;26(3):265-269.
[Crossref] [Google Scholar] [PubMed]
- Carnio J, Camargo PM, Passanezi E. Increasing the apico-coronal dimension of attached gingiva using the modified apically repositioned flap technique: A case series with a 6-month follow-up. J Periodontol. 2007;78(9):1825-1830.
[Crossref] [Google Scholar] [PubMed]
- Carnio J. Modified apically repositioned flap technique: a surgical approach to enhance donor sites prior to employing a laterally positioned flap. Int J Periodontics Restorative Dent. 2014 May;34(3):423-428.
[Crossref] [Google Scholar] [PubMed]
- Carnio J, Camargo PM, Pirih PQ. Surgical techniques to increase the apicocoronal dimension of the attached gingiva: a 1-year comparison between the free gingival graft and the modified apically repositioned flap. Int J Periodontics Restorative Dent. 2015;35(4):571-578.
[Crossref] [Google Scholar] [PubMed]
- Bowers GM. A study of the width of attached gingiva. J Periodontol.1963;34(3):201-209.
- Lang NP, Löe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontol.1972;43(10):623-627.
[Crossref] [Google Scholar] [PubMed]
- Miyasato M, Crigger M, Egelberg J. Gingival condition in areas of minimal and appreciable width of keratinized gingival. J Clin Periodontol. 1977;4(3):200-209.
[Crossref] [Google Scholar] [PubMed]
- Gartrell JR, Mathews DP. Gingival recession: The condition, process, and treatment. Dent Clin North Am. 1976;20(1):199-213.
[Crossref] [Google Scholar] [PubMed]
- Schmid MO. The subperiosteal vestibule extension. Literature review, rationale and technique. J West Soc Periodontol Periodontal Abstr 1976;24(3):89-99.
[Google Scholar] [PubMed]
- Karring T, Cumming BR, Oliver RC, Löe H. The origin of granulation tissue and its impact on postoperative results of mucogingival surgery. J Periodontol.1975;46(10):577-585.
[Crossref] [Google Scholar] [PubMed]
- Karring T, Lang NP, Löe H. The role of gingival connective tissue in determining epithelial differentiation. J Periodontal Res. 1975;10(1):1-11.
[Crossref] [Google Scholar] [PubMed]
- Karring T, Östergaard E, Löe H. Conservation of tissue specifically after heterotopic transplantation of gingiva and alveolar mucosa J Periodontal Res 1971;6(4):282-293.
[Crossref] [Google Scholar] [PubMed]
