Indexed In
- Open J Gate
- Academic Keys
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- CABI full text
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Study - (2024) Volume 12, Issue 3
Malaria Control in Angul District: Case Study of a District in Odisha towards Elimination
Nirupama Das*Received: 24-Dec-2020, Manuscript No. JTD-24-7698; Editor assigned: 29-Dec-2020, Pre QC No. JTD-24-7698 (PQ); Reviewed: 12-Jan-2021, QC No. JTD-24-7698; Revised: 16-Aug-2024, Manuscript No. JTD-24-7698 (R); Published: 13-Sep-2024, DOI: 10.35241/2329-891X.24.12.443
Abstract
Background: Angul district of Odisha has achieved a major reduction in malaria incidence and multiple challenges. This case study is an example of malaria control over last 10years.
Methods: An analysis and review of the malaria epidemiology, control strategies adopted in NVBDCP and state and district specific interventions. The regular surveillance data in Govt. health system was used to identify trends in malaria epidemiology. The challenging factors were identified through analysis of socio-economic and health indicators.
Findings: The confirmed malaria cases in Angul declined by 99.71% during the year 2019 as compared to year 2015 which was reported 29853 highest malaria cases over 10 years (2010-2019). The majority of indigenous cases were due to Plasmodium falciparum. Strategies implemented by NVBDCP and state govt. of Odisha initiative DAMaN and Angul district specific policy are likely to be related to the decline in cases over the last 10 years. The malaria diagnosis through microscopy and RDK and treatment given by age wise ACT combipack and radical treatment with Primaquine in Plasmodium falciparum cases and chloroquine treatment to Plasmodium vivax cases with radical treatment according national drug policy 2010 and 2013 on malaria. For vector control, IRS partially, full saturation of LLIN and for parasite control DAMaN and mass screening and case follow up in community as well as tribal residential school are likely to have contributed to the decline of malaria cases.
Conclusion: Angul district has made significant efforts towards elimination and has adopted a goal of elimination. Major challenges in the future will be the tracking of private malaria screening, prevention and management of anemia and improvement of socioeconomic status of community for malaria control.
Keywords
Angul; Anemia; Control; Diagnosis; Elimination; Treatment; Surveillance; Vectors
Introduction
Background
In recent years, there is a progress in malaria reduction in Odisha. Angul district of Odisha has achieved remarkable success in bringing down malaria transmission since 2015.
The progress made in Angul in last 5 years (2015-2019) is remarkable given the major challenges.
The district is placed in some of the most difficult hilly, terrain, forest fringe area; inaccessible villages 4 km walk from nearest road. In addition, large numbers of migrant workers enter from nearby district which is also high malaria transmission pockets.
Given these other challenges, the recent success in reducing malaria incidence may contain lessons for other district and also states [1].
Case Presentation
Geography, population and climate
Angul district of Odisha is like a bridge between western and coastal halves of Odisha. Rich cultural heritage, cosmopolitan approach, different temples, natural beauty, dense forest, availability of raw materials. Geographical area is 6375.00 Sq. Km area under forest is 2716.82 Sq. Km. Population density is 200 (per Sq. km). Population is 12,73,821 according to census 2011 with rural population 10,67,275 (83.78%). It is surrounded by 9 districts of Odisha, Keonjhar, Sambalpur, Subarnapur, Deogarh, Nayagarh, Cuttack, Boudh, Sundergarh. The last few years has witnessed a step rise in the economy of Angul district with the setting up of the various public sector undertakings like NALCO (National Aluminum Company), Mahanadi Coal Fields Limited (MCL), National Thermal Power Station (NTPC) and Talcher Thermal Power Station (TTPS). Apart from this, many private sectors also established. Angul district economy is based on agriculture, forestry and industrial exports to other states of India as well as other countries [2].
Angul district has seasonal rainfall with monsoon rains occurring from July-Sept. A winter season from December- January. Malaria risk areas are mainly forest and forest fringe human settlements. 5 (five) blocks out of 8 blocks contribute 90% of malaria of district (Figure 1).
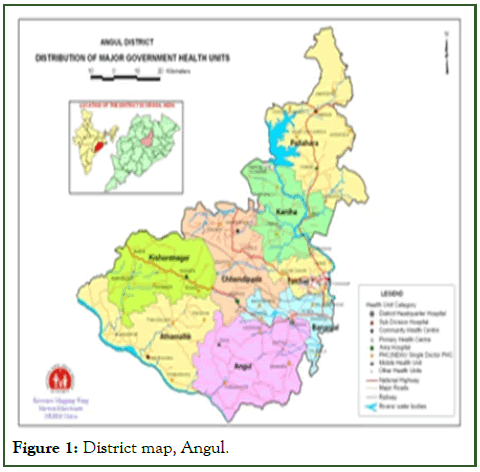
Figure 1: District map, Angul.
Programme data
A literature review was conducted through Google, Google scholar. Routine govt. health facility data was collected and reviewed by Angul district vector borne disease consultant (Nirupama Das). The reported cases described in the study were confirmed by microscopy and RDK in regular surveillance and other data collected time to time in Govt. health facility according to programme conducted like distribution and coverage of LLIN, IRS, mass survey and DAMaN [3].
Data analysis
Surveillance and vector control data were plotted using microsoft excel and trends were observed. The data compared with those described in the literature.
Programme structure
NVBDCP of Angul is integrated with Govt. health facility and ensures the implementation of control and prevention of malaria and other vector borne diseases, namely dengue, filariasis, chikungunya, kalazar and Japanese encephalitis. Out 6 VBDs of NVBDCP, malaria is dominated over all followed by dengue and filariasis in Angul district. Other three VBDs chikunguniya, Japanese encephalitis and kala-azar were not reported in Angul. The regular surveillance of malaria relies upon ASHA, primary health centers, community health centers, sub divisional hospitals and district head quarter hospital.
The service delivery structure of NVBDCP is based on ASHA, Multipurpose Health workers (MPW), Multipurpose Health Supervisors (MPHS), Laboratory Technician (LT), Vector Borne Disease Technical Supervisors (VBDTS), Sentinel Site Malaria Technical and Coordinators (SSMTC), pharmacists and doctors. Only VBDTSs and SSMTCs are getting salary from NVBDCP, Angul, others are from Govt. health system. At district level NVBDCP wing, there is a Vector Borne Diseases Consultant (VBDC) conduct all planning, monitoring, data analysis along with other activities of Vector Borne Diseases guided by additional district public health officer (VBD) of Govt. of Odisha set up. The VBDTS at block level provide a wide range services including planning, implementation, case reporting, follow up of malaria cases along with other VBDs. They also support IRS and LLIN distribution, mass screening, Information Education and Communication (IEC) and also support to ASHA, MPW, Pharmacists.
The SSMTC at SDH and DHH screen malaria and also check the parasitaemia count after administration of antimalarial. The Govt. of Odisha has provided funding to all activities of NVBDCP, Angul with support from Govt. of India [4].
Epidemiology of malaria
In Angul district, during the year 2010, total 18894 malaria positive detected by both microscopy and RDT. In the year 2011, total 10316 malaria positive cases were reported by both microscopy and RDK. Out of 10316 malaria cases, 9102 (88.23%) were Plasmodium falciparum and 1214 (11.7%) were due to Plasmodium vivax. At the mid-year of 2012, in some villages 110000 LLIN were distributed and malaria case reduction was also seen in 2012 as compared to 2011. During 2011 and 2012, monovalent RDK was used which was not adequate amount to screen malaria and microscopy was the great challenges in Angul district. From 2013 onwards, bivalent RDK supply from Govt. of India was adequate and screening also increased as compared to 2011 and 2012. In 2013, a project named Comprehensive Case Management (CCM) in collaboration with Govt. of India, NIMR, MMV and Govt. of Odisha was implemented in one of the highest malaria cases reporting block.
The theme of CCM project was Test, Treat and Track (TTT). Key gaps in access to malaria services were identified through household surveys and a detailed situation analysis. The interventions included ensuring adequate stocks of rapid diagnostic tests and antimalarial drugs at the village level, the capacity building of health workers and ASHAs, setting up microscopy centres at the primary health care level and conducting mass screening and treatment in poorly accessible areas. The programme strengthened the routine health system and improved malaria surveillance as well as the access to and quality of care. Initially, the programme led to increased case reporting due to improved detection, followed by a decline in malaria incidence. As more screening was going on, in 2015, highest number of malaria cases i.e., 29853 reported. Out of these 21372 (71.59%) of Plasmodium falciparum and 8481 (28.41%) of Plasmodium vivax cases were reported. From the year 2016, malaria cases started reduction from CCM block which was highest contributing malaria cases block of Angul district. In 2017, during monsoon season, 735350 numbers LLIN distributed fully in Angul district irrespective of all households in support of GFATM funding. At that time, Odisha state Govt. initiative programme DAMaN (Durgam Anchalre Malaria Nirakaran) was conducted. The main theme of DAMaN was mass screening of malaria by RDK in whole population in all selected forest fringe area along with hemoglobin estimation, blood pressure check in pregnant women and adolescent girl, Mid Upper Arm Circumference (MUAC) in under five children for nutritional status. In the year 2018, a huge reduction of malaria cases were reported after combined intervention and vector control through LLIN distribution, IRS and parasitemia control through DAMaN and also anaemia control by giving iron tablets during DAMaN camps. In the year 2018, 647 malaria cases reported in regular surveillance in Angul district. 496 (76.6%) of Plasmodium falciparum cases and 151 (23.4%) of Plasmodium vivax cases were reported. In the year 2019, two round DAMaN camp was also conducted along with IEC activities of LLIN use. A massive reduction of malaria cases was seen in the year 2019. Total 86 malaria cases were reported in regular surveillance. Out of these 60 (69.76%) of Plasmodium falciparum cases and 26 (30.24%) of Plasmodium vivax cases reported (Figure 2) [5].
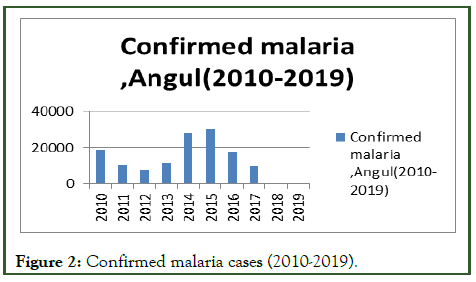
Figure 2: Confirmed malaria cases (2010-2019).
Vectors
The co-existence of potential vector sibling species of An. culicifacies (A, C and D) and An. fluviatilis S (>50%) was responsible for the high endemicity of malaria in forested area of Angul. No systematic study has been carried out on the characterization, distribution and vectorial capacity of the species complexes. An.culicifacies s.l. and An. fluviatilis s.l. were prevalent throughout the year in some areas, especially from July- November, whereas very negligible densities were recorded in the month of April and rose to maximums during the irrigation season. The marked upward trend in July and August was entirely due to a significant increase in the number of available breeding places and has been shown to have a positive correlation with malaria incidence. Malaria transmission by Anopheles subpictus Grassi and Anopheles culicifacies Giles, was studied from March 2004 to February 2007 in Angul district, Orissa, India, which is highly endemic for malaria. The anthropophilic index for the An. subpictus was higher than An. culicifacies and was highest during the summer season. Malaria sporozoite rates of 0.52% and 1.82% were detected for An. subpictus and An. culicifacies, respectively. Sporozoites were detected during the summer in An. subpictus and during the rainy season and winter in An. culicifacies. The Slide Positivity Rate (SPR) was high during the summer. An. culicifacies, An. fluviatilis, An. annularis, An. varuna, An. aconitus, An. Subpictus was predominant, suggesting that all of these species may play an important role in the epidemiology of malaria in Angul district.
Surveillance
The malaria cases reported on daily basis by either microscopy or RDK. After one day of notification, a mass screening also conducted in that village by VBDTS and MPW followed by treatment compliance. There is a functionary in quality control of RDK and microscopy. All RDK screened by ASHA, return back to CHCs to avoid duplication and false reporting of malaria positive cases. Monthly blood slides cross checking is conducted at the laboratory of ROH and FW, Govt. of India and central laboratory of NVBDCP, state headquarter. 50% of malaria positive cases by blood slides are cross checked by the laboratory of ROH and FW, Govt. of India and other 50% of malaria positive cases by blood slides are cross checked by the central laboratory of NVBDCP state headquarter. 3.5% of all negative blood slides are cross checked by central laboratory and 1.5% of negative blood slides are cross checked by laboratory of ROH and FW. Malaria training is ordered if there are false positive or negative rates beyond the acceptable limit [6].
Apart from regular passive surveillance, active surveillance was also conducted like mass screening in tribal residential school twice in year i.e., during two peak transmission season of Malaria and DAMaN twice a year since 2017. In 2017 1st round of DAMaN, 60530 RDK screened and 2387 both symptomatic and asymptomatic malaria detected. In 2nd round of 2017 DAMaN, 22544 RDK screened and 313 positive malaria detected. In 2018 1st round DAMaN, 71625 RDK screened and 812 positive both symptomatic and asymptomatic malaria cases detected. In 2018 2nd round DAMaN, 54090 RDK screened and 191 positive detected. The surprise result come during 2019 both the round DAMaN screening. In 1st round 2019, 49699 RDK screened and 54 positive detected. In 2nd round DAMaN, 35618 RDK screened with zero positive case.
Reporting is supervised on site data verification during monitoring and supervision visits to the health centers by district NVBDCP wing. In addition, checks with individual centers over phone if there are missing or incomplete reports. At district level, monthly malaria screening and positives are analyzed and respective health centers are alerted. Case surveillance investigation and IEC activities are carried out to locate the source transmission and implement containment strategies including IRS [7].
Prevention and vector control
The major prevention and vector control of malaria in Angul district were IRS, ITN and LLIN. IRS was targeted according to API (Annual Parasite Incidence) above 10 cases per 1,000 populations in block and API above 5 cases per 1000 population in subcentre due to cost effective of logistics and non-availability of spray workers in Angul district. The population coverage of IRS measured by the number of households sprayed out of the number of household targeted. However, population coverage estimated by the number of persons covered by IRS out of the estimated population at risk by the district. An average of 83.46% of the population at risk received IRS from 2010-2019. In 2014, highest coverage per person at risk was 99.4%. Synthetic pyrethroid 5% was used as insecticide from 2010-2015. Since 2016 onwards DDT 50% was used as insecticide for IRS in Angul district. IRS was the main method of vector control during (2013-2016) and very low acceptance in some areas reported, leading to difficulty in reaching the coverage required by the programme. In the meanwhile in some endemic area, ITN was also impregnated with deltamethrine. Total 32716 number of ITN impregnated from (2014-2016) as it is cost effective. In 2017, full saturation of LLIN were distributed in each household irrespective of low to high API subcentres. Total 735350 number of LLIN distributed supported by GFATM in 2017.
Treatment
Plasmodium falciparum and Plasmodium vivax malaria cases were treated according to national drug policy on malaria 2010 and 2013 of directorate of national vector borne diseases control programme, ministry of health and family welfare. All fever cases were screened for confirmation by microscopy at laboratory set up and by RDK at ASHA, PHC level. Plasmodium vivax cases were treated with chloroquine for three days. The chloroquine dose is 25 mg/kg body weight divided over three days. 10 mg/kg in day-1, 10 mg/kg body weight in day-2 and 5 mg/kg body weight in day-3. Primaquine 0.25 mg/kg body weight for 14 days. The Primaquine is contraindicated in pregnant women, infants less than one year. In uncomplicated Plasmodium falciparum malaria cases were treated with ACT (Artesunate (4 mg/kg body weight daily for three days+Sulphadoxine 0.25 mg/kg+Pyrimethamine 1.25 mg/kg body weight for 1 day) and accompanied by single dose of Primaquine (0.75 mg/Kg body weight on day 2). The pregnant women with uncomplicated Plasmodium falciparum was treated with Quinine (10 mg/Kg body weight three times daily for 7 days in 1st trimester and ACT in 2nd and 3rd trimester. For severe complicated malaria cases were admitted in hospital and treated with inj. artesunate 2.4 mg/kg i.v or i.m on admission, then 12 hrs, 24 hrs, then once a day. Three days compulsory admittance to hospital was applied to all complicated malaria cases. After that full oral dose of tab ACTSP for three days and primaquine single dose was given when able to tolerate oral dose. Each day at hospital, blood slides were collected by SSMTC deployed in district hospital and sub divisional hospitals to check parasitaemia. Then case follow up mandatory for all Malaria cases by MPW and VBDTS. They were all provided with a case follow up format from district NVBDCP wing [8].
Contribution of socioeconomic development to malaria control in Angul district
In addition to the national programme strategies and intervention provided by both national and state Govt. of Odisha for malaria control, there were also environmental and socioeconomic factors that can directly impact malaria transmission. Govt. of Odisha has been implemented many economic development programme in the last decade. So many programmes and schemes implemented through District Rural Development Agency (DRDA), Angul. The schemes were as follows.
• Mahatma Gandhi National Rural Employment Scheme
(MGNREGS)
• Pradhan Mantri-Awas Yojana (PMAY-G)
• Biju Pucca Ghar Yojana (BPGY)
• National Rural Livelohood Mission (NRLM)
• Gopabandhu Grameen Yojana (GGY)
• Pradhan Mantri Gramya Sadak Yojana (PMGSY)
So that the connectivity to unconnected rural habitation in rural areas increased. The delay of treatment have been associated with remoteness and cost of transportation to health facility was reduced. Per capita income also increased by MGNREGS and NRLM and also rapid industrialization in Angul district. The kuccha houses converted into pucca house by PMAY-G and BPGY. Meanwhile improvement health care delivery system also increased by national health mission, Odisha Govt. The socioeconomic condition also gave direct impact on malaria transmission.
Challenging factors
Remote, hard to reach population creates challenges in health care facilities. The majority of population lives in rural areas (83.78%) and population were difficult to access. In that population, extra community health volunteers engaged in 2015 for passive case detection where ASHAs were not deployed. They had provided with RDK and other anti-malarial as ASHA with registers for monthly reporting tagged to Angul Govt. health facilities [9].
Elimination strategies
Recent target malaria elimination of Angul district eliminate malaria from all SC (category 1) and moderate (category 2) transmission subcentres by 2022. Reduce the incidence of malaria to less than 1 case per 1000 population per year in all villages and by 2024. Interrupt indigenous transmission of malaria throughout the entire district, including all high transmission villages (category 3) by 2027 and Prevent the reestablishment of local transmission of malaria in areas where it has been eliminated and maintain national malaria-free status by 2030 and beyond.
Results and Discussion
Angul district has achieved a 99.71% decline in malaria cases in 2019 as compared to 2015. The evidence strategies implemented by the NVBDCP and district specific plan are likely the root of Angul district malaria success and target to eliminate malaria in the national goal of elimination 2030. The programme implemented from ASHA at village level to district hospital level with availability of RDK and other antimalarials. As a result of this improvement, of timely diagnosis and treatment through passive as well as active malaria case detection. The annual parasite incidence decrease to 0.06% in 2019. The 10 years API in Angul district is as follows (Figure 3).
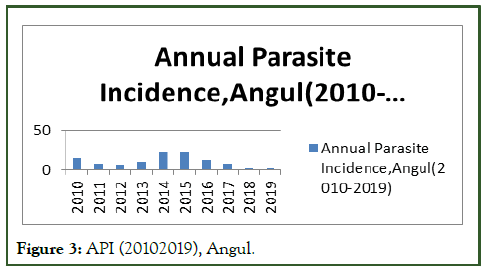
Figure 3: API (20102019), Angul.
The implementation of IRS, LLIN, mass screening through DAMaN, school sensitisation, IEC, capacity building of health personal resulted in high coverage of targeted population most at risk, contribution to the downward trend in incidence of Malaria. In order to maintain the progress of elimination of malaria in Angul district, regular passive surveillance through health facilities, mass screening through DAMaN, prevention of malaria by vector control, deployment of insecticide-treated bed nets, prompt and accurate diagnosis of illness and appropriate use of effective anti-malarial drugs substantially reduces the burden of anaemia. Surveillance is at the heart of the malaria elimination programme, not only for assessing the transmission intensity in each district and thereby stratifying it for interventions but also continuing to monitor impact of interventions. In this context, defining a malaria case or death is an important issue. At present, malaria can only be labelled if a positive blood smear is documented (based upon the WHO definition of malaria). Therefore, patients who live in a malarious area who though reporting with all the signs and symptoms of malaria and/or have positive Rapid Diagnostic Test (RDT) cannot be labelled as malaria unless a positive blood smear is documented. Moreover, the patients who do not go to the designated health centre or prefer other health system or facilities in public or private sector cannot be captured by the surveillance system. In view of this, it may be considered worthwhile to designate malaria as a notifiable disease, thereby making reporting of malaria cases mandatory for all private and public health facilities in the country. More work is needed in entomological survey and vector binomics in order to formulate more specific intervention strategies. Data capturing from private facilities have to gear up. Engagement of more number of MPWs and VBDTS require to ensure vigilance and timely response [10].
Conclusion
As per vision of national framework for malaria elimination in India 2016-2030, Angul district has made a great success towards malaria elimination. The great challenges to this goal is capturing malaria data from private facility, improvement of health indicator like anemia and socioeconomic condition.
Acknowledgment
The author would likely to thank to all VBDTS and SSMTC of district vector borne disease programme wing, Angul and health and family welfare department, Govt. of Odisha for support.
Authors’ Contributions
The author contributed the idea, shaping and drafting of paper and review and final approval.
References
- Yangzom T, Gueye CS, Namgay R, Galappaththy GN, Thimasarn K, Gosling R, et al. Malaria control in Bhutan: Case study of a country embarking on elimination. Malar J. 2012;11:1-2.
[Crossref] [Google Scholar] [PubMed]
- Xu J, Liu H. The challenges of malaria elimination in Yunnan province, people’s republic of China. Southeast Asian J Trop Med Public Health. 2012;43(4):819-824.
[Google Scholar] [PubMed]
- Lal AA, Rajvanshi H, Jayswar H, Das A, Bharti PK. Malaria elimination: Using past and present experience to make malaria-free India by 2030. J Vector Borne Dis. 2019;56(1):60-65.
[Crossref] [Google Scholar] [PubMed]
- Tripathy A, Samanta L, Das S, Parida SK, Marai N, Hazra RK, et al. Distribution of sibling species of Anopheles culicifacies sl and Anopheles fluviatilis sl and their vectorial capacity in eight different malaria endemic districts of Orissa, India. Mem Inst Oswaldo Cruz. 2010;105:981-987.
[Crossref] [Google Scholar] [PubMed]
- Kumari S, Parida SK, Marai N, Tripathy A, Hazra RK, Kar SK, et al. Vectorial role of Anopheles subpictus Grassi and Anopheles culicifacies Giles in Angul District, Orissa, India. Southeast Asian J Trop Med Public Health. 2009;40(4):713.
[Google Scholar] [PubMed]
- Rao MR, Padhy RN, Das MK. Surveillance on malaria and dengue vectors fauna across in Angul district of Odisha, India: An approach to determine their diversity and abundance, correlation with the ecosystem. J Entomol Zool Stud. 2015;3:459-469.
- Pradhan MM, Anvikar AR, Daumerie PG, Pradhan S, Dutta A, Shah NK, et al. Comprehensive case management of malaria: Operational research informing policy. J Vector Borne Dis. 2019;56(1):56-59.
[Crossref] [Google Scholar] [PubMed]
- Bal M, Das A, Ghosal J, Pradhan MM, Khuntia HK, Pati S, et al. Assessment of effectiveness of DAMaN: A malaria intervention program initiated by Government of Odisha, India. PLoS One. 2020;15(9):e0238323.
[Crossref] [Google Scholar] [PubMed]
- Pradhan MM, Meherda PK. Malaria elimination drive in Odisha: Hope for halting the transmission. J Vector Borne Dis. 2019;56(1):53-55.
[Crossref] [Google Scholar] [PubMed]
- Pradhan S, Pradhan MM, Dutta A, Shah NK, Joshi PL, Pradhan K, et al. Improved access to early diagnosis and complete treatment of malaria in Odisha, India. PLoS One. 2019;14(1):e0208943.
[Crossref] [Google Scholar] [PubMed]
Citation: Das N (2024) Malaria Control in Angul District: Case Study of a District in Odisha towards Elimination. J Trop Dis. 12:443.
Copyright: © 2024 Das N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

