Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2019) Volume 16, Issue 2
Magnitude, Characteristics, Maternal and Feto-neonatal Outcomes of Obstetric Emergencies in Western Ethiopia, Nekemte, Ethiopia, 2017
Ashenafi Habte Woyessa1*, Jote Markos Cafo2 and Thanasekaran P32Department of Nursing, Wollega University, Institute of Health Sciences, School of Nursing and Midwifery, Nekemte, Ethiopia
3Department of Psychiatric Nursing, Wollega University, Institute of Health Sciences, School of Nursing, Nekemte, Ethiopia
Received: 21-Mar-2019 Published: 02-Apr-2019
Abstract
Aim: In Ethiopia very little or probably nothing is known about significance of obstetric emergencies. This study was therefore aimed at assessing magnitude, characteristics, and outcomes of obstetric emergencies in western Ethiopia. Methods: Institution based prospective study was employed from January to June, 2017. To select the hospitals, area sampling technique was used. Total of 567 pregnant women with obstetric emergencies presented and treated in respective hospitals during the study periods and meet the inclusion criteria were consecutively included. Result: Majority (91.7%) of the identified obstetric emergencies have led to termination of pregnancy. Significant proportions (11%) of pregnant women who reached health facility were died of obstetric emergencies. Pregnant women with obstetric emergencies travelled to facility carried by people r were found to die about 8 times more likely as compared to those who transported by ambulance. While 29.21% were normal life births, still birth and neonatal death were 8.02% and 7.4% respectively. Higher number of neonatal death was also observed among mothers in whom final mode of delivery was cesarean section (AOR: 0.19(0.05, 0.62) compared to spontaneous vaginal delivery. Conclusion: This study revealed that obstetric emergencies are responsible for significant number of maternal and perinatal death. If the women have been accessed early and received optimum emergency care, many cases of the occurred death would have been prevented. Better outcome can be achieved through maximum utilization of quality and comprehensive antenatal care and organized pre-hospital obstetric emergency services.
Keywords
Obstetric emergencies; Maternal; Feto-neonatal outcome; Western EthiopiaIntroduction
Obstetric emergencies are one of the leading causes of maternal mortality in our globe. World Health Organization estimates that maternal mortality varies up to 100-fold, from 10 in wealthier countries to about 1,000 in under developed nations. Despite tremendous efforts made to reduce death that could arise in relation to pregnancy and childbirth, maternal death still remains a significant problem in many developing countries [1].
Sub Saharan African countries share the highest maternal death rate in the world. Annually about 500 maternal deaths per 100,000 live births representing over half of the total world maternal deaths occur [2]. In Ethiopia maternal and neonatal mortality rates are extremely in the highest in the world. The 2011 Ethiopian Demographic Health Survey revealed that the maternal death rate was 676 deaths per 100,000 live births and neonatal mortality was 37 deaths per 1,000 live births. In other words, for every 1,000 live births, about seven women died during pregnancy, child birth, or within two months of child birth [3,4].
Lack of organized pre hospital services, inadequate health infrastructures, financial constraints, illiteracy, and low health seeking behaviors worsen the problem in developing countries [5]. Evidence indicate that the high maternal, neonatal and child mortality rates are associated with inadequate and poor quality maternal health care [6]. A great deal of studies indicate that an estimated 74% of maternal deaths due to obstetric emergencies could have been averted if all women had access to the interventions for preventing and/ or treating all pregnancy related emergencies [7-10].
Primary prevention where possible and/or effective management of obstetric emergencies plays key role in the effort made to reduce an ever increasing maternal mortality [5]. In many third world countries obstetric emergencies like bleeding, prolonged labor, sepsis, toxemia of pregnancy, ruptured uterus, abortion and its complications are the commonly encountering obstetric emergencies [6,11]. Information of obstetric emergencies in terms of types, magnitude, and characteristic are crucial especially in countries like Ethiopia where the MMR is not yet satisfactorily reduced. Nevertheless, in Ethiopia, very little or probably nothing is known about significance of obstetric emergencies in causing maternal and neonatal morbidity and mortality.
This study was therefore undertaken to indicate the significance of obstetric emergencies in causing maternal and neonatal mortality as end clinical outcomes. The findings of this study are very much helpful for all agents including policy makers and other stakeholders who mainly work on maternal health care.
Material and Methods
Study setting
This study was conducted in three administrative zones of Wollega, Western Ethiopia. Five hospitals were selected (one from each zone). Namely, Nekemte referral hospital from East Wollega Zone, Nedjo, Mendi and Gimbi hospitals from West Wollega Zone, and Shambu Hospital from Horo Guduru Wollega Zone. The study was carried out from January 1st to June 30, 2017 among pregnant women who visited the selected hospitals for obstetric emergencies.
Study design, sampling procedure and techniques
Hospital based prospective cross sectional study was conducted the study among pregnant women presented to selected hospitals in western Ethiopia, from January to June 2017. To select the hospitals, area sampling technique was used. All pregnant women with obstetric emergencies presented and treated in respective hospitals during the study periods and meet the inclusion criteria were consecutively included.
Research tools, data processing and analysis
Data was collected by using structured and pre tested interviewer administered tool for the study purpose. The questionnaire was comprised of four parts (socio demographic characteristics, obstetric history, Types of obstetric emergencies, and maternal and perinatal outcomes). Data was initially entered in to Epi-data version 7 and later the exported to SPSS program Version 20 for data analysis. Descriptive statistics were generated and possible associations among independent variables and outcome variables were examined in bivariate analysis. Odds ratio and 95% CI was used as a measure of association.
Results
The study explored the patterns and clinical outcomes of obstetric emergencies on mothers, fetus and newborn among pregnant women who visited four hospitals in western Ethiopia the last six month duration. A total of 567 pregnant women with various obstetric emergencies were included in the study. Of which, 530 were successfully interviewed and the analyzed yielding a response rate of 93.47 percent.
Socio demographic characteristics
This section looks at the socio demographic characteristics distribution including age, ethnicity, level of education, occupation, and decision making authority on reproductive issues. The mean age of the women in this study was 25.83 and more than half (52.6%) were between the age of 25-34 years. As depicted in table below, majority (86.2%) of the respondents were Oromo in their ethnicity followed by Amhara (6.8%). Of prime concern, this study identified that the decision making authority on fertility issues was 20.8%, 44.0% and 34.3% herself, her husband and both of the couples respectively (Table 1).
| No | Variables | Category | Frequency | Percent |
|---|---|---|---|---|
| 1 | Age of the mother | 15-24 | 213 | 40.2 |
| 25-34 | 279 | 52.6 | ||
| >35 | 38 | 7.2 | ||
| 15-24 | 213 | 40.2 | ||
| 2 | Ethnicity | Oromo | 457 | 86.2 |
| Amhara | 36 | 6.8 | ||
| Tigre | 11 | 2.1 | ||
| Gurage | 8 | 1.5 | ||
| Other | 18 | 3.4 | ||
| 3 | Marital status | Single | 71 | 13.4 |
| Married | 441 | 83.2 | ||
| Divorced | 9 | 1.7 | ||
| Widowed | 9 | 1.7 | ||
| 4 | Level of education attained | No schooling | 160 | 30.2 |
| Primary school | 185 | 34.9 | ||
| Secondary school | 120 | 22.6 | ||
| College diploma | 38 | 7.2 | ||
| Degree and above | 27 | 5.1 | ||
| 5 | Occupation of mother | Government employee | 47 | 8.9 |
| Private business | 85 | 16 | ||
| Servant | 14 | 2.6 | ||
| House wife | 247 | 46.6 | ||
| Farmer | 94 | 17.7 | ||
| Other | 43 | 8.1 | ||
| 6 | Occupation of husband/partner | Government employee | 61 | 11.5 |
| Private business | 165 | 29.5 | ||
| Farmer | 259 | 48.9 | ||
| other | 54 | 10.2 | ||
| 7 | Residence | Town | 229 | 43.2 |
| Rural | 301 | 56.8 |
Table 1: Distribution of respondents by their socio demographic characteristics, western Ethiopia, Nekemte, 2017.
Findings related to base line information and obstetric history
The decision making authority on fertility issues was found to be 20.8%, 44.0% and 34.3% respectively for the mother, husband and both of the couples. Most importantly, this study revealed that more than half (55.1%) pregnant mothers who visited the hospitals for obstetric emergencies had no emergency fund (Table 2).
| No | Base line information | Category | Frequency | Percent |
|---|---|---|---|---|
| 1 | Mode of arrival | Being carried by people | 10 | 1.9 |
| Public car | 114 | 21.5 | ||
| Ambulance | 345 | 65.1 | ||
| On foot | 56 | 10.6 | ||
| Other | 5 | 0.9 | ||
| 2 | Treatment given in ambulance | Yes | 276 | 52.1 |
| No | 254 | 47.9 | ||
| 3 | Forms of treatment given in ambulance(N=276) | Positioning | 161 | 58.3 |
| Resuscitation withy fluid given | 68 | 24.6 | ||
| Supplemental oxygen | 20 | 7.2 | ||
| Other | 27 | 9.7 | ||
| 4 | Decision making on fertility issues | Her self | 110 | 20.8 |
| Her husband/partner | 233 | 44 | ||
| Both couples | 182 | 34.3 | ||
| His/her family | 5 | 0.9 | ||
| 5 | Presence of emergency fund | Yes | 238 | 44.9 |
| No | 292 | 55.1 | ||
| 6 | Arrival time | Day time | 290 | 54.7 |
| Night time | 146 | 27.5 | ||
| On weekend | 91 | 17.7 | ||
| 7 | Time elapsed between arrival and initiation of treatment in minutes | <15 | 456 | 86 |
| 15-30 | 38 | 7.2 | ||
| 30-60 | 21 | 4 | ||
| >60 | 15 | 2.8 | ||
| 8 | Mothers’ habit | Alcohol intake | 64 | 12.1 |
| Smoking | 8 | 1.5 | ||
| Fasting | 37 | 7 | ||
| Chew chat | 5 | 0.9 | ||
| Have no history of habits | 416 | 78.5 | ||
| 9 | Distance from home to nearest health facility in kilometer | <5 | 114 | 21.5 |
| May-15 | 120 | 22.6 | ||
| 15-30 | 205 | 38.7 | ||
| >30 | 91 | 17.2 | ||
| 10 | Women’s knowledge and readiness for emergencies | knows some of obstetric danger signs | 182 | 34.33 |
| Knows nearby ambulance Number | 242 | 45.7 | ||
| Knows selection of place of delivery | 443 | 83.6 |
Table 2: Distribution of respondents by their base line information in western Ethiopia, Nekemte, Ethiopia, 2017.
This study has explored pregnant mothers’ relevant obstetric history. About 21.9% have not attended ANC. Among the women who have been attended ANC, only 29.9% of them attended four times. Common types of preexisting medical conditions identified during ANC were chronic hypertension (55%) followed by ‘other’ (16%) problems like anemia and respiratory tract infections. Even though ambulance was means of arrival for majority (65.1%) of respondents, nearly half (47.1%) of them did not receive any form of treatment before arrival. The study also revealed that more than half (55.1%) had no emergency fund. Time elapsed between arrival and initiation of treatment in minutes for majority (86.0%) of them was <15 minutes (Table 3).
| No | Obstetric history | Category | Frequency | Percent |
|---|---|---|---|---|
| 1 | Type of pregnancy | Wanted/planned | 450 | 84.9 |
| Unwanted/unplanned | 80 | 15.1 | ||
| 2 | Parity | Primi | 181 | 34.2 |
| Para 2-4 | 276 | 52.1 | ||
| Para 5 and above | 73 | 13.8 | ||
| 3 | ANC follow up | Yes | 414 | 78.1 |
| No | 116 | 21.9 | ||
| 4 | Time of the first ANC visit | First trimester | 206 | 38.9 |
| Second trimester | 196 | 37 | ||
| Third trimester | 21 | 4 | ||
| 5 | Number of ANC visit(N= 414) | Once | 38 | 9.1 |
| Twice | 111 | 26.8 | ||
| Three times | 152 | 36.7 | ||
| Four times and above | 124 | 29.9 | ||
| 6 | History of violence | Beating | 24 | 4.5 |
| Stabbing | 4 | 0.8 | ||
| Throwing | 10 | 1.9 | ||
| Kicking | 7 | 1.5 | ||
| Rape | 33 | 6.2 | ||
| Control of finance | 33 | 6.2 | ||
| Other | 7 | 1.5 | ||
| No history of abuse | 412 | 77.7 | ||
| 7 | Presence of preexisting diseases | Yes | 41 | 7.7 |
| No | 471 | 88.9 | ||
| Unknown | 18 | 3.4 |
Table 3: Distribution of respondents by their obstetric history in western Ethiopia, Nekemte, Ethiopia, 2017.
Chronic hypertension (55%) followed by ‘other’ (16%) problems like anemia and respiratory tract infections were among the identified preexisting medical or surgical problems during ANC visit. Out of all respondents, 88 (16.6%) of respondents have found to have some disorders during ANC visit (Table 4).
| Preexisting disease | Frequency(N= 88) | Percent |
|---|---|---|
| Hypertension | 44 | 50 |
| Anemia | 28 | 31.88 |
| Bleeding | 7 | 7.95 |
| Hyperemesis gravidrum | 1 | 1.14 |
| Weight loss | 3 | 3.41 |
| others | 5 | 5.68 |
| Total | 88 | 100 |
Table 4: Types of newly diagnosed disorders during ANC visit in western Ethiopia, Nekemte, Ethiopia, 2017.
Findings related to diagnosed obstetric emergencies
One of the aims of this study was identifying magnitude and commonly encountering obstetric emergencies in the study area. The most common diagnosed obstetric emergencies were obstructed labor (17.9%) followed by abortion (12.5%). Antepartum hemorrhage (11.3%) and preterm labor (7.9%) were also common diagnoses (Table 5).
| Patterns of obstetric emergency | Age of respondents | Total | |||
|---|---|---|---|---|---|
| 15-24 | 25-34 | >35 | |||
| Frequency | Percent | ||||
| Retained placenta | 4 | 23 | 0 | 27 | 5.1 |
| Preterm labor | 15 | 27 | 0 | 42 | 7.9 |
| Premature rupture of membrane | 15 | 23 | 0 | 38 | 7.2 |
| Ante partum hemorrhage | 25 | 33 | 2 | 60 | 11.3 |
| Postpartum hemorrhage | 4 | 17 | 2 | 23 | 4.3 |
| Severe anemia | 1 | 6 | 0 | 7 | 1.3 |
| Retained second baby | 3 | 1 | 0 | 4 | 0.8 |
| Ectopic pregnancy | 0 | 2 | 1 | 3 | 0.6 |
| Disseminated intravascular coagulation | 0 | 0 | 5 | 5 | 0.9 |
| Cord prolapse | 0 | 7 | 1 | 8 | 1.5 |
| Puerperal sepsis | 0 | 1 | 1 | 5 | 0.6 |
| Obstructed labor | 40 | 51 | 4 | 95 | 17.9 |
| Mal presentation | 10 | 19 | 3 | 32 | 6 |
| Abortion | 49 | 8 | 9 | 66 | 12.5 |
| Severe pre eclampsia | 15 | 17 | 2 | 34 | 6.4 |
| Eclampsia | 13 | 2 | 3 | 18 | 3.4 |
| Uterine rupture | 1 | 14 | 3 | 18 | 3.4 |
| Fetal distress | 7 | 18 | 0 | 25 | 4.7 |
| Intra uterine fetal death | 7 | 3 | 2 | 12 | 2.3 |
| Uterine inversion | 0 | 2 | 0 | 2 | 0.4 |
| Others | 3 | 5 | 0 | 8 | 1.5 |
| Total | 213 | 279 | 38 | 530 | 100 |
Table 5: Distribution of diagnosed of obstetric emergency by age of respondents in western Ethiopia, Nekemte, Ethiopia, 2017.
Majority (91.7%) of identified cases of obstetric emergencies in this study have led to termination of pregnancy. As to the place of delivery, out of hospital delivery i.e. home delivery and on street delivery were 9 (1.79%) and 16 (3.03%) respectively. Delivery conducted outside of health facility, the delivery was assisted by untrained birth attendants (8%), health extension workers (56%), Emergency Medical and technicians (20%) and family members (16%). Among pregnant women in whom obstetric emergencies have led to termination of pregnancy, the final mode of delivery was identified. While emergency caesarian section was final mode of delivery form most mothers (36.62%), about 3.49% of the women have undergone laparotomy for ectopic pregnancy and ruptured uterus (Figure 1).

Figure 1: Final mode of delivery due to obstetric emergencies in western Ethiopia, Nekemte, Ethiopia, 2017.
Maternal outcomes of obstetric emergencies
The study identified the consequences of obstetric emergencies on mothers’ health and life. Nearly two third (57.07%) of the women were peacefully discharged after termination of pregnancy. A significant proportion (11%) of maternal death due to obstetric emergencies was recorded (Figure 2).
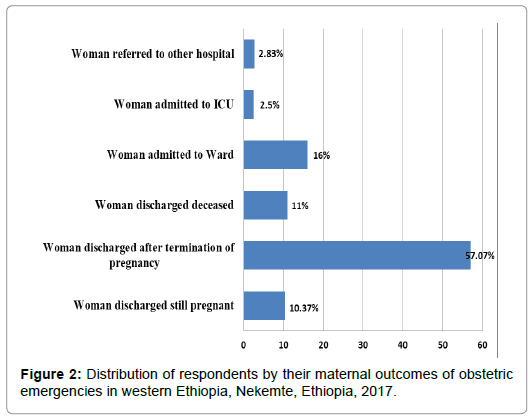
Figure 2: Distribution of respondents by their maternal outcomes of obstetric emergencies in western Ethiopia, Nekemte, Ethiopia, 2017.
The study also explored the underlying causes of maternal death. The main contributing factors for death were obstetric hemorrhage (31.9%) followed pregnancy related infections (21.27%). In about 15%, the underlying cause of death was unknown (Figure 3).
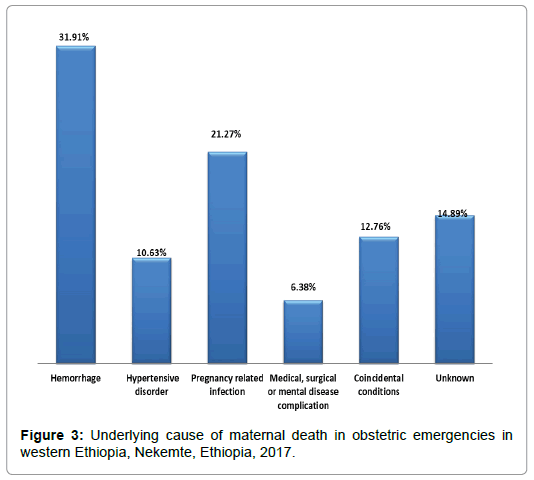
Figure 3: Underlying cause of maternal death in obstetric emergencies in western Ethiopia, Nekemte, Ethiopia, 2017.
The main contributing factors for maternal death were obstetric hemorrhage (31.9%) followed pregnancy related infections (21.27%). Mothers who did not attend ANC were more likely to die of obstetrics emergencies as compared to mothers who received ANC service (p-value=0.00). Mothers who travel longer than 15 kilometer to reach health facility were about 10 times more likely to die of obstetrics emergencies as compared to mothers who travel less than 5 kilometer (p-value=0.00). Pregnant women with obstetric emergencies travelled to facility carried by people should were found to die about 8 times more likely as compared to those who transported by ambulance (Table 6).
| Variables | Category | Crude OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value |
|---|---|---|---|---|---|
| Age of the Women | 15-24 | 4.89 (1.82,13.15) | 0 | 3.68 (0.76,17.87) | 0.1 |
| 25-34 | 2.39 (0.99,5.71) | 0.05 | 1.21 (0.28,5.14) | 0.78 | |
| 35 and above | R | R | R | R | |
| Mode of facility arrival | By people/foot | 1.42 (0.53,3.76) | 0.48 | 7.92 (1.76,35.70) | 0.00* |
| Public car | 2.19 (0.90,5.34) | 0.08 | 5.30 (1.18,23.81) | 0.02* | |
| Ambulance | R | R | R | R | |
| Presence of emergency fund Marital status |
Yes | R | R | R | R |
| No | 0.67 (0.36,1.25) | 0.21 | 1.29 (0.400,4.19) | 0.666 | |
| Single | 0.93 (0.37,2.30) | 0.88 | 0.28 (0.05,1.57) | 0.15 | |
| Divorced | 0.04 (0.01,0.18) | 0 | 0.008 (0.00,0.11) | 0.00* | |
| Married | R | R | R | R | |
| Distance from facility in kilometer | <5 | 1.05 (0.46,2.39) | 0.89 | 1.24 (0.40,3.83) | 0.7 |
| Jun-15 | 1.52 (0.70,3.28) | 0.28 | 10.08 (2.90,34.97) | 0.00* | |
| 16-30 | 2.21 (0.75,6.45) | 0.14 | 16.79 (3.46,81.28 ) | 0.00* | |
| >31 | R | R | R | R | |
| Time of treatment initiation | <15 minute | R | R | R | R |
| 16-30 minutes | 4.05 (0.54,30.23) | 0.173 | 2.613 (0.243,28.137) | 0.428 | |
| >30 minutes | 1.53 (0.19,11.9) | 0.68 | 0.274 (0.022,3.473) | 0.318 | |
| Pre-existing illness | No | R | R | R | R |
| Yes | 0.24 (0.109,0.53) | 0 | 0.24 (0.08,0.72) | 0.01* | |
| Unknown | 0.36 (0.09,1.32) | 0.12 | 0.52 (0.10,2.65) | 0.43 | |
| Type of pregnancy | Wanted/planned | R | R | R | R |
| Unwanted | 0.45 (0.22,0.92) | 0.03 | 2.27 (0.204,25.33) | 0.5 | |
| Arrival times | Day time | R | R | R | R |
| Night time | 0.51 (0.27,0.97) | 0.043 | 0.918 (0.377, 2.237) | 0.85 | |
| On weekend | 1.43 (0.52,3.91) | 0.47 | 2.60 (0.60,11.31) | 0.2 | |
| ANC attendance | Yes | R | R | R | R |
| No | 0.41 (0.21,0.76) | 0 | 0.15 (0.05,0.45) | 0.00* | |
| Decision making role on sexuality | Both Couples | R | R | R | R |
| Husband alone | 0.37 (020, 0.709) | 0.002 | 0.09 (0.02,0.31) | 0.00* | |
| *: Marital status | |||||
Table 6: Binary logistic regression of maternal obstetric emergency outcomes with selected study variable, Nekemte, Ethiopia, 2017.
Duration of hospital stay following the diagnosed obstetric emergency or related problem was considered as possible outcome. Among admitted cases, while majority (83%) of them stayed in hospital less than of 10 days, the hospital duration of stay for significant proportion (10%) of women was 15 days and above. Among commonly identified underlying causes of ward admission, pregnancy related infection accounted contributed 28.23% followed by obstetric hemorrhage (25.8%) (Table 7).
| Cause of ward/ICU admission | Frequency (N=8) | Percent |
|---|---|---|
| Complications of Abortion | 6 | 7.05 |
| Obstetric hemorrhage | 22 | 25.88 |
| Hypertensive disorders | 12 | 14.11 |
| Pregnancy related infection | 24 | 28.23 |
| Medical, surgical/mental disease complications | 8 | 9.41 |
| Suboptimal management | 11 | 12.94 |
| coincidental conditions | 2 | 2.35 |
| Total | 85 | 100 |
Table 7: Binary logistic regression of maternal obstetric emergency outcomes with selected study variable, Nekemte, Ethiopia, 2017.
Feto-neonatal outcomes of obstetric emergencies
This research has looked the fate of infants and neonates with a mother diagnosed of obstetric emergency. About 29.21% of women gave normal life birth. Still birth and neonatal death were 8.02% and 7.4% respectively (Figure 4).
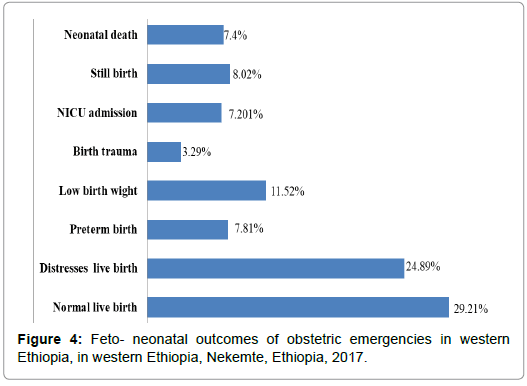
Figure 4: Feto- neonatal outcomes of obstetric emergencies in western Ethiopia, in western Ethiopia, Nekemte, Ethiopia, 2017.
The most common underlying cause of neonatal death was noticed to be distress/asphyxia (39%) followed by neonatal sepsis (33%). The remaining death was contributed by hypothermia (11%) and other causes (17%). Infants born from mothers arriving hospitals on weekend days carried higher chance of death (p-value=0.01). Higher number of neonatal death was also observed among mothers in whom final mode of delivery was cesarean section (AOR: 0.19(0.05, 0.62) compared to spontaneous vaginal deliver (Table 8).
| Variables | Category | Crude OR(95%CI) | p-value | Adjusted OR (95%CI) | p-value |
|---|---|---|---|---|---|
| Mode of facility arrival | People/on foot | 1.20 (0.45,3.23) | 0.7 | 0.53 (0.14,1.98) | 0.35 |
| Public car | 3.76 (1.12,12.55) | 0.03 | 3.62 (0.85,15.31) | 0.08 | |
| Ambulance | R | R | R | R | |
| Residence | Urban | R | R | R | R |
| Rural | 0.63 (0.31,1.25) | 0.18 | 0.50 (0.18,1.40) | 0.19 | |
| Marital status | Divorced | 0.32 (0.06,1.61) | 0.16 | 0.02 (0.00,0.28) | 0.01* |
| Married | R | R | R | R | |
| Distance from facility in kilometer | <5 | R | R | R | |
| Jun-15 | 0.42 (0.15,1.13) | 0.08 | 046 (0.14,1.55) | 0.21 | |
| 16-30 | 1.54 (0.50,4.72) | 0.44 | 2.05 (0.48,8.80) | 0.33 | |
| >31 | 0.36 (0.13,1.01) | 0.05 | 0.47 (0.10,2.11) | 0.32 | |
| Time of treatment initiation | <15 minute | R | R | R | R |
| 16- 30 minutes | 3.38 (0.45,25.3) | 0.23 | 2.80 (0.30,26.26) | 0.36 | |
| Type of pregnancy | Wanted | R | R | R | R |
| Unwanted | 3.38 (0.79,14.34) | 0.09 | 0.50 (0.02,8.87) | 0.63 | |
| Arrival times | Day time | R | R | R | R |
| Night time | 0.44 (0.21,0.92) | 0.03 | 0.63 (0.26,1.52) | 0.3 | |
| On weekend | 057 (0.23,1.40) | 0.22 | 0.20 (0.05,0.71) | 0.01* | |
| ANC attendance | Yes | R | R | R | R |
| No | 11.71 (1.59,86.27) | 0.01 | 3.60 (0.39,33.07) | 0.25 | |
| Decision making role on sexuality matter | Both Couples | R | R | R | R |
| Husband alone | 0.65 (0.34,1.25) | 0.2 | 0.96 (0.39,2.35) | 0.94 | |
| Mother’s substance use | No | R | R | R | R |
| Yes | 2.11 (0.63,7.03) | 0.22 | 25.19 (1.89,334.3) | 0.01* | |
| Final mode of delivery | SVD | R | R | R | R |
| MVA | 2.31 (0.26,20.22) | 0.44 | 0.07 (0.00,1.12 | 0.06 | |
| Cesarean section | 0.19 (0.07,051) | 0 | 0.19 (0.05,0.62) | 0.00* | |
| Instrumental Delivery | 2.53 (0.29,22.15) | 0.4 | 4.00 (0.38,41.30) | 0.24 |
*: Marital status
Table 8: Underlying cause of ward admission after obstetric emergencies in western.
Discussion
Globally, obstetric emergencies take the top rank in causing of maternal mortality. Literacy, poverty, lacks of quality antenatal care, low transportation facilities and insufficient equipment and providers amplify the problem in underdeveloped nations [3-8]. Ethiopia is one of the countries blamed to have the highest maternal death in the world. It has been reported that the country is one of the six countries that contribute about over 50% of the deaths [12,13]. Poor health care seeking habit lesser coverage of health services, unavailability of sufficient transport facilities, deep rooted poverty and wrong beliefs are among the few factors known to worsen the end outcomes obstetric emergency in developing countries [14,15].
Very socio-economic status a community certainly contributes to negative outcomes of obstetric emergency. In present study, while in higher proportion (44.0%) husband or partners were mandated for decision making on fertility issues, only 110 (20.8%) women have authority for decision making. Women of higher socio-economic status usually receive better pregnancy outcomes. Because they are relatively better informed, likely to develop better choices, more likely to develop and implement birth readiness and are more empowered to make decisions in case of they come across with obstetric emergencies [16-18].
In this study, 414 (78.1%) of pregnant women who have visited the selected hospitals for obstetric emergencies had received ANC at least once. Study done in Kenya to assess feto maternal outcome of obstetric emergencies reported that 93.4% of women attended an antenatal clinic at least once. The difference could be due to better awareness and service of ANC as a result of the difference of socio economic status between the two countries [19].
When faced with obstetric emergency that might needs referral, arranging a private car consume time and. Delays to reach facilities and misdiagnosis of cases are directly related to near miss mortality. In this study, 345 (65.1%) patients have used ambulance to reach the hospital which is higher as compared with the finding from India study [20-22].
Nearly two third (57.07%) of the women were peacefully discharged from hospitals after termination of pregnancy. Significant number, 47(11%) of pregnant women who reached health facility were died of their obstetric emergencies. This is in line with a study done in south west Nigeria which reported were 17 maternal deaths out of 262 obstetric emergencies and greater than 4% of Indian study [19,23]. It is also noticed that fetal and neonatal death were noticed to be 8.02% and 7.4% respectively As reported, in this study there were 11.52% low birth weight and 7.8% pre term babies while the remaining 7.2% were admitted to the neonatal intensive care units.
Conclusion
This study has shown that obstetric emergencies do occur and found to be responsible for significant number of the maternal and perinatal mortality. If the women have been accessed early and received optimum emergency help both during transportation and in health facilities, many of the occurred death would have been avoided. Better outcome can therefore be achieved through maximum utilization of quality and comprehensive antenatal care and organized pre-hospital and in hospital obstetric emergency services.
Declarations
Ethics approval and consent to participate: The research was approved by Wollega University (Reference Number፡ W/R 100, 617/W/C፡ 1-26). Formal letter of permission and support was written to the respective health facilities. Prior to collecting the required data both verbal consent and written consent were taken from all of the study subjects.
Availability of data and materials: the raw data supporting our findings are available from authors on a reasonable request.
Consent for publication: Consent to publish this work has been taken from the approving committee
Authors’ Contribution
AH designed and developed the research proposal, involved in supervision of data collection process, statistical analysis and preparation of the final document. JM helped with research tool preparations, supervising data collection, and involved in revision of the final manuscript.
Acknowledgement
We would like to acknowledge Wollega University for funding this research. We would also like to extend our heartfelt gratitude to our study participants for their cooperation in responding to the questions whilst they were in physical and emotional sufferings.
REFERENCES
- Buekens P. Is estimating maternal mortality useful? Bull world health organ. 2001;79:179.
- UN and African union commission: Report on progress in achieving the millennium development goals in Africa.2013
- Chukwudebelu WO, Okonofua A, Odunsi K. Preventing maternal mortality in developing countries. In contemporary obstetrics and gynaecology for developing countries. 2013;644.
- Federal democratic republic of ethiopia central statistical agency om 2015: edhs 2015. Addis Ababa, Ethiopia.
- Haines A, Cassels A. Can the millennium development goals be attained. British Medical J. 2004;329:394-397.
- The millennium development goals 2012.
- Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: Analysis of the 2011 Ethiopian demo graphic and health survey. BMC Pregnancy and Child birth.2014;14:161.
- World Health Organization: WHO maternal and child health fact sheet,2012.
- Federal democratic republic of Ethiopia central statistical agency OM: EDHS. Addis Ababa, Ethiopia.2015.
- WHO, UNFPA, UNICEF and World bank 2012: Trends in maternal mortality: 1990-2010.
- Drife J, Lueslay DM, Baker PN (2004) “ Maternal mortality” in obstetrics and gynecology and evidence-based text for MRCOG, pp: 196-204.
- Birmeta K, Dibaba Y, Woldeyohannes D (2013) Determinants of maternal health care utilization in Holeta town, central Ethiopia, birmetaet al. BMC health services research 13:256.
- Hogan CH, Foreman KJ, Naghavi M, Ahn SY, Wang M, et al. (2010) Maternal mortality for 181 countries. 1980 – 2008: A systematic analysis of progress towards millennium development goal 5. Lancet 376: 1389-1390.
- Najam R, Gupta S, Chowdhury H (2015) Pattern of obstetrical emergencies and fetal outcomes in a tertiary care center. Acta Med Int 2: 105-110.
- Catherin N, Anushila SR, Ramakrishna B (2014) Goud 3 obstetric emergencies presenting to a rural community maternity hospital 2: 264-269.
- Bhandari TR, Dangal G (2014) Emergency obstetric care: strategy for reducing maternal mortality in developing countries. NJOG 17: 8-16.
- Nwobodo EL (2006) Obstetric emergencies as seen in a tertiary health institution in North-Western Nigeria: Maternal and fetal outcome. Nigerian Medical Practitioner 49: 54-55.
- Drife J, Lueslay DM, Baker PN (2004) Maternal mortality in obstetrics and gynecology and evidence-based text for MRCOG. pp: 196-204.
- Najam R, Gupta S, Chowdhury H (2015) Pattern of obstetrical emergencies and fetal outcomes in a tertiary care center. Acta Med Int 2: 105-110.
- Maryland R (2016) Ethiopia sy. Central statistical agency (CSA).
- Elzabeth W (2011) Maternal and fetal outcomes among women with obstetric emergencies referred to Kenyata national hospital, Kenya. pp: 32- 38.
- Shivani B (2017) Pattern of term obstetric emergencies referred from health centers to Rims. Emir 4: 376-382.
- Zhang WH, Alexander S, Bouvier-Colle MH, Macfarlane A (2015) Incidence of severe pre-eclampsia, postpartum hemorrhage and sepsis as surrogate marker for severe maternal morbidity in a European-based study: MOMS survey. BJOG 112: 89-96.
Citation: Woyessa AH, Cafo JM, Thanasekaran P. Magnitude, characteristics, maternal and feto-neonatal outcomes of obstetric emergencies in western Ethiopia, Nekemte, Ethiopia, 2017. Clinics Mother Child Health. 2019;16:319.
Copyright: © 2019 Woyessa, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

