Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Mini Review - (2020) Volume 4, Issue 2
Long-term Smoking Cessation of Preoperative Cessation Programs: A Mini-Review
Joseph D Phillips*Received: 31-Aug-2020 Published: 22-Sep-2020, DOI: 10.35248/2684-1606.2020.4.133
Abstract
Smoking increases the perioperative risks of surgery and millions of smokers undergo major operations each year. Few studies in the literature related to preoperative smoking cessation programs have data regarding long-term rates of abstinence. This article reviews the long-term (≥ 12 months) quit rates of preoperative smoking cessation programs.
Keywords
Long-term outcomes; Smoking cessation; Perioperative; Preoperative; Surgery
Introduction
Smoking remains a significant worldwide public health issue. Over 8 million people die each year from the effects of tobacco. Approximately 7 million of these deaths are from direct tobacco use and an estimated 1.2 million occur in non-smokers being exposed to second-hand smoke [1]. An estimated 60 million smokers worldwide undergo major surgical procedures each year and it is well known that smoking increases the risks of perioperative complications in this population [2]. While one of the first reports of pulmonary complications after surgery related to smoking was published in 1944 [3], the first randomized trial related to preoperative smoking cessation and its effects on postoperative complications wasn’t published until 2002 [4]. Several additional randomized trials evaluating short-term smoking cessation outcomes were published over the next decade, a few of which included perioperative and long-term outcomes up to 12 months after surgery [5]. When compiled, these initial studies suggested improved rates of cessation at 12 months after surgery with intensive smoking cessation programs that lasted 4-8 weeks preoperatively. It has been proposed that surgical patients who are current smokers may benefit the most from intensive preoperative smoking cessation interventions including counseling and nicotine replacement therapy [6]. The perioperative period has been noted to be a “teachable moment” for patients when they are more likely to quit [7-20]. Consequently, this period is ripe for success. While numerous studies focus on short-term quit rates in the perioperative period, this article reviews the long-term (≥12 months) rates of smoking cessation of preoperative smoking cessation programs (Table 1).
| Characteristics of Included Studies | ||||
|---|---|---|---|---|
| First Author (year) | Design | Sample Size & Population | Post-operative Follow-up | % Cessation (control vs. intervention) |
| Aldrete (1987) [8] | Cohort | N=25; single private hospital; United States | 12 months | 11.1 vs. 56.3* |
| Ratner (2004) [10] | RCT | N=237; single academic hospital; Canada | 12 months | 19.7 vs. 19.8 |
| Villebro (2008) [12] | RCT | N=120; multiple academic hospitals; Denmark | 12 months | 3.3 vs. 21.7* |
| Sadr Azodi (2009) [13] | RCT | N=117; multiple academic hospitals; Sweden | 12 months | 14.5 vs. 32.7* |
| Thomsen (2010) [14] | RCT | N=130; multiple academic hospitals; Denmark | 12 months | 9 vs. 13 |
| Lee (2015) [15] | RCT | N=168; single academic hospital; Canada | 12 months | 8.3 vs. 25.4* |
| Wong (2012) [19] | RCT | N=286; multiple academic hospitals; Canada | 12 months | 25.2 vs. 36.4* |
| Wong (2017) [20] | RCT | N=296; multiple academic hospitals; Canada | 12 months | 26.2 vs. 42.4* |
| Fay (2020) [30] | Retrospective cohort | N=82; single academic hospital; United States | 12 months | 42.6a |
| Phillips (2020) [31] | Retrospective cohort | N=82; single academic hospital; United States | 24 months | 51.7a |
| Balmer (2020) [32] | Prospective cohort | N=27; single academic hospital; United States | ~ 40 monthsb | 47.6 |
| Van Slyke (2017) [33] | Retrospective cohort | N=85; single academic hospital; Canada | >21 monthsc | 23.8a |
| Taylor (2017) [34] | Prospective cohort | N=50 ; single academic hospital; Australia | 12 months | 28.0a |
*p<0.05, (a) No control group, (b) Average time from surgery to completion of survey reported as 3.7 years, (c) Range of follow-up 21 to 159 months. RCT: Randomized Controlled Trial.
Table 1: Lists the characteristics of studies with at least 12 months of follow-up included in this review.
Counseling and Nicotine Replacement Therapy
One of the first studies to suggest the long-term efficacy of preoperative cessation efforts was published in 1987 [8]. This was a small, single institution study of 25 patients with a brief educational intervention. The 12 month self-reported cessation rate in the intervention group was 56.3% vs. 11.1% in the control group (p<0.05) [9]. While this suggested perioperative interventions could be successful, the first randomized controlled trial (RCT) to evaluate the long-term effects of smoking cessation demonstrated no difference in quit rates between patients who received counseling and nicotine replacement therapy (NRT) vs. no intervention 12 months after a variety of surgical procedures (approximately 20% in both groups) [10].
NRT can be provided in sustained form via transdermal patches of varying doses or short acting forms including gum, sublingual tablets, lozenges, inhalation and oral/nasal sprays. A Cochrane review concluded that “high-quality evidence” exists for all licensed forms of NRT to aide in smoking cessation efforts [11]. Regardless of setting, NRT increases the rate of stopping smoking by 50%-60% over patients who do not receive any NRT while trying to quit.
Three additional preoperative cessation program RCTs with at least 12 months of follow-up were published between 2008 and 2010 involving counseling and NRT compared to no intervention or inconsistent advice regarding the risks of smoking related to surgery [12-14]. Villebro et al. evaluated the 12 month cessation rates of smokers undergoing elective hip and knee replacements who were randomized to receive counseling and NRT or no intervention. At 12 months, the intervention group had a significantly higher rate of smoking abstinence (21.7% vs. 3.3%, p<0.01). In this study, low nicotine dependence and having a non-smoking partner had the highest predictive value of being smoke-free at 1 year. Similarly, Sadr Azodi et al. randomized elective orthopedic and general surgery patients to weekly telephone or in person meetings and NRT vs. brief or no cessation information related to surgery. This trial demonstrated a significantly higher rate of patients in the intervention group self-reporting that they were not smoking at 1 year (32.7% vs. 14.5%, p<0.05). In this study, low nicotine dependence and BMI >30 were significantly associated with smoking cessation 1 year after surgery. Interestingly, Thomsen et al. found no difference in the 12-month quit rate of breast cancer surgery patients randomized to a brief course of motivational interviewing (1 interview of 45 to 90 minutes) and NRT compared to standard of care (13% vs. 9%). A systematic review and meta-analysis that primarily included the above 4 RCTs noted that the literature is supportive that preoperative interventions likely lead to more successful cessation rates ≥ 12 months after surgery [9].
More recently, a RCT evaluated the combination of counseling and NRT, similar to previous studies. This Canadian study, published in 2015, randomized 168 smokers undergoing a variety of elective surgeries identified in the preoperative clinic as smokers to receive brief counseling, smoking cessation brochures, referral to a Quitline and free NRT for 6 weeks to standard care, which included inconsistent perioperative cessation advice [15]. Seventy-six percent of patients were available for 12 month telephone follow-up and the self-reported rate of 7-day point prevalence (PP) of abstinence from smoking was 25.4% in the intervention group versus 8.3% in the control group (p<0.05). Being in the intervention group and a lower nicotine dependence (Fagerstrom [16] score <4) at the time of surgery were significant predictors of successful cessation at 12 months.
Varenicline
Separate from NRT, varenicline has also been investigated as a preoperative long-term cessation aide. Varenicline acts on the α4β2 nicotinic acetylcholine receptor as both a partial agonist and antagonist [17]. These actions reduce the rewarding effect of nicotine and also help reduce withdrawal symptoms [18]. The first preoperative RCT to study the benefits of varenicline in improving smoking cessation rates was a multi-center, double- blind placebo-controlled trial of elective ambulatory or inpatients scheduled for a variety of surgeries [19]. In this study, all patients received two 15-minute standardized counseling sessions and the target quit date was 24 hours prior to surgery. Patients were followed for 1 year via telephone calls and the primary outcome was 7-day PP abstinence from smoking at 12 months. They found a significant increase in the likelihood of 7-day PP of being smoke free in the varenicline group (36.4% vs. 25.2%, p<0.05). Unlike many of the previous studies, abstinence was correlated with mailed urinary cotinine tests. This group also reported the results of a RCT comparing varenicline, counseling and a fax referral to a telephone Quitline to brief advice and self-referral to a Quitline in patients undergoing elective, non-cardiac surgery [20]. The primary outcome measure was the 7-day PP abstinence from smoking at 12 months and the secondary outcome was continuous abstinence (defined as being smoke free for the preceding 4 weeks) at 3, 6, and 12 months. The 7-day PP rate at 12 months was significantly higher with the more intensive interventions (42.4% vs. 26.2%, p<0.01). The 4-week continuous abstinence rate was higher in this group as well at all time points measured: 3 months (34% vs. 19%, p<0.01), 6 months (34% vs. 19%, p<0.01) and 12 months (32% vs. 17%, p<0.01). Participating in the more intensive smoking cessation program was significantly associated with smoking abstinence 12 months after surgery (Relative Risk 1.58, 95% Confidence Interval 1.12- 2.21; p<0.01).
Other Adjunct Therapies
Pamphlets, brochures, e-learning modules, and web-based education programs have been utilized for smoking cessation but have not been specifically studied alone with long-term outcomes. Quitlines, where patients may call for information and support, have been included as part of programs with long-term outcomes and may be a practical way to provide additional follow-up, especially in more rural populations [21]. Text messaging related to smoking cessation has been shown to be effective overall in a meta-analysis of 20 published studies encompassing 15,593 patients [22]. However, many of these studies included other components, were not preoperative, and did not have 12-month outcomes.
Bupropion is a nicotinic acetylcholine receptor antagonist and also inhibits dopamine and norepinephrine uptake in the synaptic cleft [23]. These actions likely mitigate the stimulatory effects of nicotine on the postsynaptic membrane and reduce withdrawal symptoms and cravings, similar to varenicline. Based on RCT data with at least 12 weeks of therapy, an approximate overall smoking abstinence rate of 17% at 52 weeks with bupropion was noted [24]. Interestingly, of the 26% of patients who had quit by the end of bupropion therapy, 62.5% were still abstinent at 52 weeks. However, these studies were not limited to preoperative patients. One RCT of preoperative patients randomized to bupropion (n=24) or placebo (n=23) did not demonstrate a significant difference at 6 weeks after starting treatment, at the time of surgery, or at 6 months postoperatively between the two groups [25]. Based on available data, The Society for Perioperative Assessment and Quality Improvement (SPAQI) notes that there is insufficient evidence that bupropion should be provided to perioperative patients to assist with smoking cessation [21].
Electronic cigarettes (ECs) were intended to be a smoking cessation aide. While these devices may carry less carcinogenic material into the lungs than traditional smoking, data demonstrating their efficacy for smoking cessation are highly variable. A recent systematic review and meta-analysis concluded that due to limitations of the available studies, “it is impossible to make strong inferences regarding whether e-cigarette use promotes, has no effect or hinders smoking cessation” [26]. Based on available data, many experts would not recommend the use of ECs for cessation in the perioperative period and recommend the use of more proven pharmacotherapy [21,27].
Implementation
Issues with perioperative smoking cessation are not related to a lack of efficacious interventions, but rather a lack of implementation and adoption of these interventions into routine clinical practice [2]. A lack of time, appropriate training and cessation resources have all been identified as barriers to effective preoperative tobacco cessation programs [28]. Physicians, in particular, can be reluctant to engage patients in busy clinics or around the time of sensitive diagnoses, such as cancer. These concerns highlight the importance of collaborative, multi-disciplinary teams to facilitate smoking cessation [29].
We have recently reported the implementation and long-term outcomes (6, 12, and 24 months postoperatively) of an intensive, multi-dimensional preoperative smoking cessation program for patients undergoing lung resection (Figure 1) [30,31]. Through this program all smokers are identified and strongly encouraged by the surgeons to quit and informed their surgery may be cancelled or delayed if they continue to smoke. Smokers were also highly encouraged to meet with a certified tobacco treatment specialist (TTS) for at least a 1-hour counseling session involving motivational interviewing (an opt-out approach), and personalized pharmacotherapy. Carbon monoxide breath testing was administered at preoperative visits and on the day of surgery to verify smoking status. Patients were also given a moderate exercise regimen to follow and could have additional in-person or telephone sessions with the TTS as needed. Interventions were provided free of charge to all patients. Seventy-three percent of patients who met with a TTS used some form of NRT. Rates of cessation were 55.6% at 12 months and 51.7% at 2 years. Eighty- three percent of patients with 2 years of follow-up reported at least one successful cessation attempt. Impressively, 62% of patients who quit prior to surgery never returned to smoking, compared to just 18% who were able to quit following their operation, which was statistically significant (p<0.001).
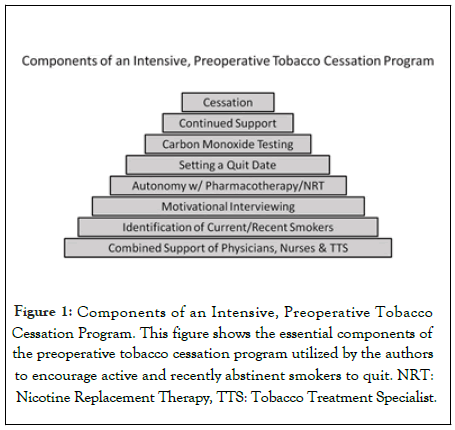
Figure 1: Components of an Intensive, Preoperative Tobacco Cessation Program. This figure shows the essential components of the preoperative tobacco cessation program utilized by the authors to encourage active and recently abstinent smokers to quit. NRT: Nicotine Replacement Therapy, TTS: Tobacco Treatment Specialist.
A recently published small study (n=27) demonstrated a self- reported continued smoke-free rate of 47.6% for those patients able to quit prior to total joint arthroplasty, with an average time from operation to survey of 3.7 years [32]. Similarly, of 47 patients who underwent elective cosmetic surgery with an average follow up of 63 months, 23.8% self-reported they had not smoked since surgery [33]. A recent Australian study of 50 consecutive smokers attending an outpatient pre-admission clinic prior to elective surgery who received brief (15 minute) counseling sessions, brochures, referral to a Quitline and 2 weeks of NRT noted the 7-day PP of self-reported smoking abstinence at 12 months was 28.0% [34].
Summary
Strong data exists that the preoperative and perioperative period are opportune times to assist patients with smoking cessation. No one method has proven to be optimal in helping patients quit. Thus, it is likely that multi-factorial, personalized and multi- dimensional programs will have the highest rates of success. Regardless, one of the most important aspects of any program is conveying the importance of cessation to the patient and offering your assistance. Focusing on identifying current and recently quit smokers who are at risk of relapse and integrating cessation efforts into everyday clinical practices is also fundamental to successful implementation. In addition to the short-term benefits of decreased perioperative complications, many of these programs have a demonstrated rate of long-term successful smoking abstinence extending to at least 12 months postoperatively.
REFERENCES
- Tobacco. World Health Organization 2020.
- Nolan MB, Warner DO. Perioperative tobacco use treatments: Putting them into practice. BMJ. 2017; 358.
- Morton HJV. Tobacco smoking and pulmonary complications after operation. Lancet. 1944; 1:368-70.
- Møller AM, Villebro N, Pedersen T, Tønnesen H. Effect of preoperative smoking intervention on postoperative complications: A randomised clinical trial. Lancet. 2002; 359(9301):114-117.
- Tønnesen H, Thomsen T. Review: Long-term effect of perioperative smoking cessation programmes. Clin Heal Promot. 2011; 1(1): 22-26.
- Thomsen T, Tønnesen H, Møller AM. Effect of preoperative smoking cessation interventions on postoperative complications and smoking cessation. Br J Surg. 2009; 96(5): 451-461.
- Shi Y, Warner DO. Surgery as a teachable moment for smoking cessation. Anesthesiology. 2010; 112(1): 102-107.
- Aldrete JA. Cessation of cigarette smoking by suggestion in the perianesthetic period. Anesthesiol Rev. 1987; 14(4): 22-24.
- Berlin NL, Cutter C, Battaglia C. Will preoperative smoking cessation programs generate long-term cessation? A systematic review and meta-analysis. Am J Manag Care. 2015; 21(11): e623-e631.
- Ratner PA, Johnson JL, Richardson CG. Efficacy of a smoking-cessation intervention for elective-surgical patients. Res Nurs Heal. 2004; 27(3): 148-161.
- Hartmann-Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst Rev. 2018; 2018(5): 1-194.
- Villebro NM, Pedersen T, Møller AM, Tønnesen H. Long-term effects of a preoperative smoking cessation programme. Clin Respir J. 2008; 2(3): 175-182.
- Sadr Azodi O, Lindström D, Adami J. The efficacy of a smoking cessation programme in patients undergoing elective surgery-A randomised clinical trial. Anaesthesia. 2009; 64(3): 259-265.
- Thomsen T, Tønnesen H, Okholm M. Brief smoking cessation intervention in relation to breast cancer surgery: A randomized controlled trial. Nicotine Tob Res. 2010; 12(11): 1118-1124.
- Lee SM, Landry J, Jones PM, Buhrmann O, Morley-Forster P. Long-term quit rates after a perioperative smoking cessation randomized controlled trial. Anesth Analg. 2015; 120(3): 582-587.
- Fagerstrom K-O, Schneider NG. Measuring Nicotine Dependence: A Review of the Fagerstrom Tolerance Questionnaire. Journal of Behavioral Medicine.1989; 12(2): 159-182.
- Tapper AR, Mckinney SL, Nashmi R, et al. Nicotine Activation of A4* Receptors: Sufficient for Reward, Tolerance, and Sensitization.Science. 2004; 306: 1029-1032.
- Henningfield JE, Fant R V, Buchhalter R, Stitzer ML. Pharmacotherapy for Nicotine Dependence. CA Cancer J Clin. 2005; 55: 281-299.
- Wong J, Abrishami A, Yang Y. A Perioperative Smoking Cessation Intervention with Varenicline A Double-Blind, Randomized, Placebo-Controlled Trial. Anesthesiology. 2012; 117(4): 755-764.
- Wong J, Abrishami A, Riazi S. A Perioperative Smoking Cessation Intervention with Varenicline, Counseling, and Fax Referral to a Telephone Quitline Versus a Brief Intervention: A Randomized Controlled Trial. Anesth Analg. 2017; 125(2): 571-579.
- Wong J, An D, Urman RD. Society for Perioperative Assessment and Quality Improvement (SPAQI) Consensus Statement on Perioperative Smoking Cessation. Anesth Analg. 2020; 131(3): 955-968.
- Scott-Sheldon LAJ, Lantini R, Bock BC. Text Messaging-Based Interventions for Smoking Cessation: A Systematic Review and Meta-Analysis. JMIR Mhelath Uhealth. 2016; 4(2).
- Wilkes S. The Use of Bupropion SR in Cigarette Smoking Cessation. International Journal of COPD. 2008; 3(1) :45-53.
- Jackson SE, McGowan JA, Ubhi HK. Modelling continuous abstinence rates over time from clinical trials of pharmacological interventions for smoking cessation. Addiction. 2019; 114(5): 787-797.
- Myles PS, Leslie K, Angliss M, Mezzavia P, Lee L. Effectiveness of Bupropion as an Aid to Stopping Smoking before Elective Surgery: A Randomised Controlled Trial.Anaesthesia. 2004; 59: 1053-1058.
- El Dib R, Suzumura EA, Akl EA. Electronic nicotine delivery systems and/or electronic non-nicotine delivery systems for tobacco smoking cessation or reduction: A systematic review and meta-analysis. BMJ Open. 2017; 7(2).
- Steliga MA. Smoking Cessation in Clinical Practice: How to Get Patients to Stop. Semin Thorac Cardiovasc Surg. 2018; 30(1): 87-91.
- Warren GW, Dibaj S, Hutson A, Cummings KM, Dresler C, Marshall JR. Identifying targeted strategies to improve smoking cessation support for cancer patients. J Thorac Oncol. 2015; 10(11): 1532-1537.
- Luxton NA, MacKenzie R, Shih P. Smoking Cessation Care in Cardiothoracic Surgery: A Qualitative Study Exploring the Views of Australian Clinicians. Hear Lung Circ. 2019; 28(8): 1246-1252.
- Fay KA, Phillips JD, Hasson RM, Fannin A, Millington TM, Finley DJ. Outcomes of an Intensive, Preoperative Smoking Cessation Program. In: Annals of Thoracic Surgery. Vol 109. Elsevier USA; 2020: e137-e139.
- Phillips JD, Fay KA, Ramkumar N. Long-term Outcomes of a Preoperative Lung Resection Smoking Cessation Program. J Surg Res. 2020; 254: 110-117.
- Balmer JC, Anderson AB, Barfield WR, Pellegrini VD, Demos HA. Preoperative Smoking Cessation as a Durable Form of Long-Term Smoking Cessation. J Surg Orthop Adv. 2020; 29(2): 103-105.
- Van Slyke AC, Carr M, Knox ADC, Genoway K, Carr NJ. Perioperative and long-term smoking behaviors in cosmetic surgery patients. Plast Reconstr Surg. 2017; 140(3): 503-509.
- Taylor H, Karahalios A, Bramley D. Long-term effectiveness of the preoperative smoking cessation programme at Western Health. ANZ J Surg. 2017; 87(9): 677-681.
Citation: Phillips JD, Fay KA, Finley DJ (2020) Long-term Smoking Cessation of Preoperative Cessation Programs: A Mini-Review. J Surg Anesth. 4:133.
Copyright: © 2020 Phillips JD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
