Indexed In
- Open J Gate
- Academic Keys
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- CABI full text
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research - (2020) Volume 8, Issue 5
Irrational use of Antibiotics and Associated Health Risks in District Charsadda, Pakistan
Muhammad Taj Akbar1, Hamidullah Shah2*, Shah Faisal3, Abdullah1, Faheem Jan4, Sharif Zada5, Rahma Amrani6 and Asma Qudrat12Department of Pathology, Lady Reading Hospital, Peshawar, KPK, Pakistan
3Department of Biotechnology, Bacha Khan University Charsadda, KPK, Pakistan
4Programmatic Management of Drug Resistance, TB Unit Abbottabad, KPK, Pakistan
5Department of Microbiology, Hazara University, Mansehra, KPK, Pakistan
6Department of Biotechnology, National Higher School of Biotechnology, Taoufik Khaznadar, Constantine, Algeria
Received: 11-Jul-2020 Published: 27-Jul-2020, DOI: 10.35248/2329-891X.20.8.353
Abstract
Antibiotics are drugs used for the treatment most of the bacterial infections. The rapid and irrational use of antibiotics presents a high risk of developing health complications and also leads to antibiotic resistance. The current study is designed to know about the ratio of irrational use of antibiotics and associated risks with it. Antibiotics remain an integral part of the prescriptions at DHQ Hospital Charsadda. Our study was based mainly on antibiotic prescriptions. A total of 500 prescriptions were examined in which 62% of the prescriptions were examined thoroughly and found rational whereas 38% were irrational. 26.98% of these irrational prescriptions were due to inaccurate doses. Additionally, 25.39% of them were prescribed for incorrect durations, indicating basic misconceptions in the prescriptions. Among the total irrational prescriptions, the frequency of antibiotics-drug interactions, drug-food interactions, and contraindications were 18.51%, 14.5%, and 14.81% respectively. Irrational use of antibiotics is a serious health threat and its consequences lead to the development of antibiotic resistance in different bacterial species. There is a need for intervention of studies in different hospitals of Pakistan to avoid irrational use and encourage rational use of antibiotics.
Keywords
Irrational use; Antibiotics; Prescription; Antibiotic resistance; Pakistan
Introduction
In 1928, Alexander Fleming has discovered the first antibiotic by accident and has dramatically changed infectious disease treatment, thus it was life-saving for millions of people especially during WWII. The absence of the bacterial resistance mechanisms, the limited availability of antibiotics along with their high cost was believed to be the major reasons for their attentive consumption [1]. A few years later, the industry of antibiotics has witnessed increasing production of antibiotics which led to decreasing their cost, and thereby the consumption of antibiotics has become more and more irresponsible. Reduced costs of production along with fast-growing global market especially in economically developing nations and the approval of antibiotics among health professionals have encouraged pharmaceutical companies to take advantage and started introducing new antibiotics to the market every week making it difficult for doctors to stay up to date and providing microorganisms the chance to develop different types of resistance mechanisms that guarantee their survival. Rational use of drugs is basically achieved by appropriately receiving drugs that suit the patients’ clinical needs, in doses that meet their individual demands, for an appropriate duration, and at the lowest cost to them and the community.
Irrational antibiotics prescription across the globe was reported in many studies [2]. Even though the majority of upper respiratory infections are viral and can be neutralized by the immune system, a significantly high percentage of unnecessary use of antibiotics (50% to almost 100%) was reported by the World Health Organization (WHO). Another study conducted by the WHO has revealed that, from 1992 to 1996, about 30% of Upper Respiratory Tract Infections (URTI) have been exposed to irrational antibiotic prescriptions in 13 low-middle and high-income countries. On average, statistics have shown that the number of prescribed drugs is 3.5 per the recommendation in Pakistan, 76% of which are antibiotics, and a great percentage of them are given by injection. Moreover, 78% of patients had antibiotics in their prescriptions, 74% of them received antibiotics in the parenteral mode of administration. For children from 1 year to age 14, the antibiotic prescription was considerably high (84%) [3]. Sales of antibiotics have eventually exceeded the rate of infectious diseases that are expected to be treated (WHO, 1995). Antibiotics are the most frequently prescribed drugs worldwide. It is of great importance to rationally use them, considering that ill-advised use can negatively impact the patient ’ s health, causing antibiotic resistance and increasing healthcare costs. Antibiotic prescription goes through several phases:
• Perception of need-is an antibiotic necessary?
• Choice of antibiotic-what is the most appropriate antibiotic?
• Choice of schedule-what dose, administration route, frequency, and duration are adequate?
• Monitoring efficacy-is the treatment effective?
Since the ’ 80s, the number of newly-discovered molecules decreased and the funding into antimicrobial research is on the decline. Now, deaths caused by resistant infections are slowly increasing. In the U.S., nosocomial infections are causing mortality 4 times more than road traffic accidents [4]. Worldwide, more than 50% of the totality of drugs are prescribed, dispensed, or sold inappropriately and 50% of patients fail to use them correctly (WHO, 1985). Contrarily, nearly one-third of the world ’ s population suffers from a shortage of essential medicines supply. One of the most costeffective medical interventions known is the treatment with medicines, considering that between 20% and 40% of the national health budgets are spent on pharmaceuticals in developing countries, and 10% to 20% in developed ones (WHO, 2002). Hence, the inappropriate and irrational use of a large number of medicines is a serious problem.
The present study focuses on estimating the dimensions of irrational use of antibiotics and suggests recommendations for the healthcare community in order to limit these practices by restricting the prescription of antibiotics with wrong doses, duration, and frequency in addition to paying more attention to contraindications and different types of antibiotic interaction.
Materials and Methods
Study region and population
The descriptive study was carried out at the Division of Healthcare Quality (DHQ) Charsadda from October 2019 to February 2020. The Charsadda district regarded as an important region in Khyber Pakhtunkhwa Province, Pakistan. It occupies an area of 996 Km2 and inhabited by 1.6 million individuals.
Respondents and the hospital
The respondents are a group of 500 OPDs (Out Patient Departments) individuals visiting the pharmacy and having antibiotics in their prescriptions. The DHQ Charsadda has a well-equipped pharmacy having at least 150 elements of drugs in considerable amounts. Different groups of prescribed antibiotics are included in these drugs. Both local and multinational brands can be found in these antibiotics. Local medicines are given by the government under the Medicine Coordination Cell (MCC) program while multinational drugs are provided by WHO and other health associations. Many antibiotics are available in the pharmacy, such as penicillin, macrolides, fluoroquinolones, chloramphenicol, sulphonamides, tetracyclines, and aminoglycosides, with only a limited amount of antibiotics in the form of syrup. The Tuberculosis (TB) control program unit in DHQ Hospital Charsadda is in charge of giving anti-tubercular drugs to patients. More than one antibiotic can be contained in some prescriptions. However, such prescriptions are not significant and, thus, are excluded from this investigation.
Generation of data
Special permissions were taken from the medical superintendent of the DHQ for the audit of antibiotics prescribing to 80 to 100 patients visiting the pharmacy every day. Patients were surveyed using standardized questionnaires with pre-designed answer options and space for open answers that were filled by all of the patients (Appendix-1). The questionnaire comprised sociodemographic data such as age, gender, level of education, and social status. The collected information includes the diagnosis of the patients, lab results, and the antibiotics prescribed in each case with the relevant data (a type of antibiotic, doses, duration, and frequency of the treatment). The evaluation of the prescriptions was based on whether the choice of antimicrobial agent, pharmacokinetic parameters, and the indications for use are appropriate.
The following questions were designed to assess the irrational use of antibiotics:
• Was the chosen antibiotic appropriate?
• Is the dose prescribed correctly?
• Does the duration of the treatment fit the needs of the patient?
• And finally, was the choice of the drug administration route correct?
The questions were simplified and easy to understand by patients. Forms of recommendations to improve prescriptions that include proper dose, treatment duration, drug interactions, and more were issued to every medical staff in the hospital; medical staffs were also requested to decide whether the clinical cases were particularly influenced by the antibiotic treatment. Overall, the importance of prescribing only recognized forms of antibiotics was weighted. Finally, attentiveness is required during the prescription of the treatment of a particular disease including spending sufficient time with the patients. During the open meetings, health professionals of the hospital discussed patients individually and shared recommendations. These are the most important definitions in this study.
Rational use of antibiotics
Strict conditions are to be followed to appropriately prescribe antibiotics. They have to meet the clinical needs of the patients, respect appropriate doses, not exceed the appropriate given period of time and finally be available for a low price to both patients and the community (WHO, 1985). An example of such a situation is treating typhoid using Ciprofloxacin in a dose of 1500 mg per day for 2 weeks.
Irrational use
Inappropriate use of antibiotics is confirmed if at least one of the rational use conditions is not respected (WHO, 1985). For instance, using Ciprofloxacin for typhoid treatment with no less than 1500 mg per day for less than 2 weeks.
Correct treatment duration
Despite the fact that medical textbooks generally recommend different antibiotic treatment durations depending on the nature of the infection, the treatment duration optimizations continue to create a great deal of debate. The treatment can take only 7 days to cure of pharyngitis or up to 9 months for the antibiotic treatment of Tuberculosis (TB) [5,6].
Drug-drug interaction
Drug interactions occur when a certain substance affects a consumed drug by increasing, decreasing its activity, or even producing a new effect. An example of drug-drug interaction would be the decreased effectiveness of oral contraception pills when interfering with antibiotics [7].
Drug-Food interaction
Taken together with certain types of food or beverage, the activity of the drug can be affected. For instance, the clearance of some drugs by the Gastrointestinal Tract (GIT) can be blocked when consuming them at the same time with grapefruit juice. In this case, the total concentration of the drug is absorbed from the GIT to reach toxic levels in the plasma [8].
Contraindications
Contraindication is a situation when taking a drug or carrying out a medical operation can cause potential undesirable or threatening reactions in patients with allergies or during pregnancy. For example, the previous hypersensitivity to penicillin is considered as a contraindication that imposes its use in the future.
Drug-Disease interaction
Drug-disease interaction is defined by unwanted or dangerous effects resulting from potential interference of the drug in people previously suffering from certain health conditions. As an illustration, taking erythromycin in patients with cardiac arrhythmia will worsen their tachycardia.
Correct medicine frequency
It describes how often the drug should be taken and the specified intervals. For example, doxycycline is required once per day for 4 weeks to 2 months in acne treatments.
Results
Interviews were conducted with a total number of 500 patients who take antibiotics in their prescriptions. The age of the interviewers was 50.53 ± 22.18 years on average (median age, 56.0 years), 46.2% of them were females, and 53.8% males, 73% had primary, secondary, or college education levels and 79% were married. Rational and irrational prescriptions of antibiotics were respectively recorded at 62.2% and 37.8% respectively, while many important data was lacking from the analyzed antibiotics prescriptions of patients such as name, age, and sex of the patient in addition to some details about the given antibiotics like dosage form, prescribed dose, dose frequency, drug contraindication, drug interactions, and duration of the treatment. Prescribed antibiotics and the number of patients for each antibiotic are detailed in Table 1.
| Antibiotic prescribed | No. of Patients |
|---|---|
| Tetracycline (doxycycline) | 71 |
| Quinolones (ciprofloxacin) | 88 |
| Macrolides (erythromycin) | 61 |
| Chloramphenicol | 15 |
| Penicillin (amoxicillin, ampicillin) | 182 |
| Aminoglycosides (neomycin, gentamycin) | 51 |
| Sulfonamide | 32 |
| Total | 500 |
Table 1: Number of patients by the type of antibiotics prescribed at the DHQ Charsadda from October 2019 to February 2020.
According to Table 1, the most prescribed antibiotic in the DHQ is Penicillin. Moreover, rational and irrational prescriptions rates for all the mentioned antibiotics in all patients are listed in Table 2.
| Type of prescription | Frequency | Age percentage |
|---|---|---|
| Rational prescription | 311 | 62.2 |
| Irrational prescription | 189 | 37.8 |
| Total prescription | 500 | 100 |
Table 2: Distribution rate of rational and irrational prescriptions of antibiotics.
Table 2 illustrate the frequency distribution of rational and irrational prescriptions of antibiotics in the DHQ Charsadda. Information is presented in the form of a doughnut chart (Figure 1).
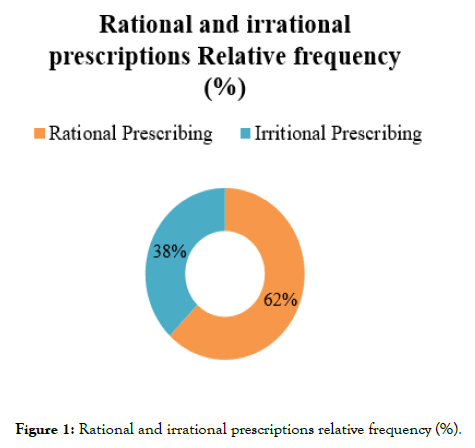
Figure 1. Rational and irrational prescriptions relative frequency (%).
In Table 2 rational prescriptions number is observed at 311 patients (62%) in total against 189 patients for irrational prescriptions (38%). Conditions including correct duration, frequency, doses, and duration, not containing possible drugdrug, drug-food, drug-disease interactions or contraindication should be respected. Lab findings, present, and history of the patient’s health should also be taken into consideration. All these parameters provide evidence that the medical staff has properly consulted the patient.
Irrational prescriptions have shown substandard patient counselling which resulted in various inaccuracies such as incorrect dose, inadequate frequency of antibiotics, etc. Table 3 indicates different categories of observed irrational prescriptions and shows their shortcomings frequency and percentage. These shortcomings may be very dangerous for patients’ health and may result in the development of potential antibiotic resistance.
| Type of irrational prescribing | Frequency | Percentage |
|---|---|---|
| Wrong dose frequencies | 51 | 26.98 |
| Incorrect durations | 48 | 25.39 |
| Antibiotic-food interactions | 27 | 14.28 |
| Antibiotic-drug interactions | 35 | 18.51 |
| Contraindicated prescriptions | 28 | 14.81 |
| Total | 189 | 100 |
Table 3: Types of observed irrational prescriptions and their frequency.
Table 3 indicates different categories of observed irrational prescriptions and shows their shortcomings frequency and percentage. These shortcomings may be very dangerous for patients’ health and may result in the development of potential antibiotic resistance.
Table 3 lists different categories of irrational prescriptions along with their distribution frequency. Impropriate antibiotic dose frequencies were counted at 51 prescriptions (26.98%) and the evidence was the wrong choice of tetracycline (doxycycline) dose frequency which was given twice per day while the proper dose frequency for the treatment of cholera and acne is 100 mg per day and the reason for that is the fact that tetracycline has a relatively long half-life (from 18 to 22 hours), excessive consumption of this antibiotic will consequently generate severe side effects and toxicity. More details about wrong dose frequency prescriptions are shown in Table 4.
| Antibiotic | Dose | Frequency |
|---|---|---|
| Tetracycline (doxycycline) | Twice a day 100 mg tablet | 17 |
| Amoxicillin | 250 mg tablet twice a day | 11 |
| Ampicillin | 500 mg tablet daily | 8 |
| Erythromycin | 250 mg tablet twice a day | 9 |
| Ciprofloxacin | 250 mg tablet twice a day | 6 |
| Total | ------ | 51 |
Table 4: Antibiotics prescribed with inaccurate dose frequency and distribution.
Generally, the appropriate dose of penicillin is 500 mg per 6 hours in the treatment of typhoid fever and the one for Amoxicillin to treat otitis media (inflammation of the middle ear) is recommended at 150 mg per day. However, Table 3 shows an incorrect choice of doses in treating Urinary Tract Infections (UTI) using Amoxicillin were the recommended dose is 250 mg (missing duration) while the majority of analyzed prescriptions show different treatment durations such as 500 mg per day or 250 mg three times a day. In other cases, recommended doses of Erythromycin in treating severe Respiratory Tract Infection (RTI) is 250 mg to 500 mg every 6 hour and the one for the treatment of typhoid fever with ciprofloxacin is 1500 mg a day [9]. Still many prescriptions contain irrational indications.
A total of wrong treatment duration was observed in irrational prescriptions at 25.39% (48 prescriptions). Table 5 reveals data about the antibiotics prescriptions’ frequency with wrong durations.
| Antibiotics | Duration | No. of prescriptions |
|---|---|---|
| Amoxicillin | 4 days | 10 |
| Ampicillin | 5 days | 12 |
| Ciprofloxacin | 7 days | 13 |
| Chloramphenicol | 5 days | 4 |
| Doxycycline | 5 days | 9 |
| Total | ------- | 48 |
Table 5: Antibiotics prescribed with incorrect durations.
Pharyngitis correct treatment duration is one week while the observed duration was only 4 days. Furthermore, the adequate duration for using Amoxicillin is 1 g twice per day for 5 to 7 days instead of 4 days. Treating Lower Respiratory Tract Infections (LRTE) requires taking 2 g of Ampicillin per day for 4 to 7 days. Doxycycline is prescribed for patients with acne for a duration of 3 months and Ciprofloxacin for the treatment of acute or chronic Prostatitis (inflammation of prostate glands) in a dose of 500 mg twice per day for 28 days. Finally, Chloramphenicol is given for patients with septicaemia with the recommended dose and duration of 12.5 mg/Kg every 6 hours for 7 days.
27 cases of drug-food interactions were observed at the hospital (18.28%) and one of the common cases is taking antibiotics especially tetracycline and quinolones along with milk or its derivatives which results in reducing the antibiotic bioavailability. Another situation of drug-food interaction is taking fiber-rich foods along with penicillin that results in slowing the medication absorption rate due to the effect of fibers that delays gastric emptying. Prescribing theophylline (bronchodilator) along with erythromycin which may lead to potential toxicity is an example of 35 (18.51%) observed antibiotic-drug interaction cases. In Table 6, different combinations of antibiotic-drug that may produce negative effects on patients and the observed frequency of these combinations at the hospital [10].
| Antibiotic | Drug | Resulting effect | No. of prescriptions |
|---|---|---|---|
| Erythromycin | Theophylline (bronchodilator) | Possible toxicity of theophylline | 9 |
| Doxycycline | Antacids (reduced acidity in the stomach) | Reduce the bioavailability of doxycycline | 15 |
| Erythromycin | Analgesics (reduce pain) | Increase the plasma conc. of analgesic effect | 6 |
| Quinolones | Antihistamines (reduce allergy etc) Antipsychotics (for anxiety) | Ventricular arrhythmias | 5 |
Table 6: Possible antibiotic-drug interactions detected in prescriptions.
Table 6 shows that taking Erythromycin along with Theophylline reduces the renal clearance of Theophylline and induces potential toxicity while a complex form by doxycycline taken along with antacids reducing by that the bioavailability of doxycycline. Additionally, Quinolones consumption along with antipsychotics and antihistamines medicines causes ventricular arrhythmias.
Prescriptions containing contraindications were counted at 14.81% (28 cases). Table 7 illustrates the rate of antibiotics prescribed in contraindication cases.
| Antibiotics | Frequency |
|---|---|
| Doxycycline’s | 13 |
| Erythromycin | 9 |
| Ciprofloxacin | 6 |
| Total | 28 |
Table 7: Frequency of antibiotic prescription in contraindication situations.
Quinolones increase cardiac arrhythmias that can be seen in electrocardiogram (increased QT interval) it can also cause weight-bearing joints cartilage damage in children. Quinolones are therefore contraindicated in people suffering from epilepsy, QT prolongation, and children less than 8 years old. Moreover, these types of contraindications were observed in 6 cases.
Tetracycline should also be avoided in pregnant women and children due to its effect on skeleton development. Tetracycline causes the discoloration of new-borns teeth when the breastfeeding mother takes it.
Figure 2 summarizes the relative frequencies of various types of irrational prescriptions observed during this study.
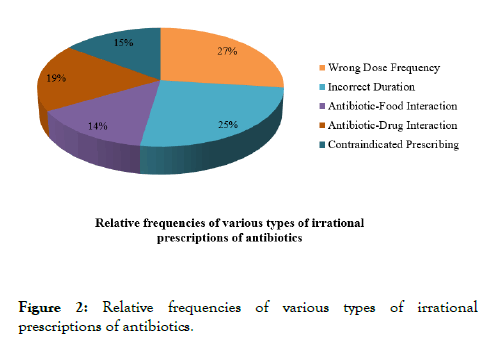
Figure 2. Relative frequencies of various types of irrational prescriptions of antibiotics.
Discussion
Antibiotics remain an integral part of the prescriptions at DHQ Hospital Charsadda. Our study was based mainly on antibiotic prescriptions. Only 62% of prescriptions were rational whereas the remaining 38% were not 26.98% of these irrational prescriptions were at inaccurate dose frequency and therefore were extremely dangerous to the patients. Additionally, 25.39% of them were prescribed for incorrect durations, indicating basic misconceptions in the prescriptions. Among the total irrational prescriptions, 18.51% were for antibiotics-drug interactions, 14.5% for drug-food interactions, and 14.81% for contraindications. The estimate of rational prescriptions from this study was 62% which is higher than those from other developing countries such as India with 43%, Nigeria with 48%, Yemen with 46%, Lebanon with 17.5% and Zimbabwe with 29% [11-13] and in Ottoman empire with 60.9%. On the other hand, the estimate of irrational prescription from this study which was at 38% is better than the one from Turkey with 53% of irrational prescriptions [14]. In the United Kingdom hospitals, errors are made in only 1.5% of prescriptions. Often, Doxycycline has been inappropriately given to 28.57% patients. Members of the same class, tetracycline, may have very specific spectra of activity. Great attention should be paid to dose, duration, frequency, etc. for any antibiotic prescriptions [15,16]. This could be done by making it mandatory for the prescribers to attend the Continuing Medical Education (CME) as regular training, in order to enhance their knowledge and introduce good prescribing practices. Moreover, the influence of pharmaceutical industries and their delegates needs to be checked continuously in health organizations in order to increase the transparency in drug prescription far away from their influence. All these considerations would go a long way in providing optimal, low cost, and effective drugs to the patients. Nurses and hospital pharmacists will become more responsible for prescriptions for acute conditions. Some national control programs should be developed by the Ministry of Health in order to limit and forbid irrational prescription of antibiotics. However, programs such as postgraduate training are difficult to apply to and need to run over a long period. Easier control programs including methods for controlling the use of antibiotics should be developed and implemented in hospitals where antibiotics are used regularly. The combination of training and implementation strategies with the distribution of national treatment guidelines is also recommended in the future.
Like any investigation, the present study had some limitations examples are:
• Sampling was limited to one hospital so it cannot be generalized
• The severity of prescribing mistakes could not be assessed and confirmed
In the hospital, clinicians prescribe antibiotics without baseline protocols or guidance regarding the antibiotic prescription. There is no system to check the irrational use of antibiotics. The hospital does not have an antibiotic sensitivity reporting system, there are no baseline protocols guiding clinicians for antibiotic prescription, neither an antibiotic sensitivity reporting system nor a system to check the irrational use of antibiotics.
Conclusion
Irrational use of antibiotics is a serious health threat and its consequences lead to the development of antibiotic resistance in different bacterial species. There is a need for intervention of studies in different hospitals of Pakistan to avoid irrational use and encourage rational use of antibiotics. Multicentre investigations are recommended to compare the types as well as the frequencies of prescriptions’ errors made at DHQ and other hospitals throughout Pakistan in order to get a clear understanding of the epidemiology of antibiotic prescribing errors in our health institutions.
Acknowledgment
We are grateful to DHQ Hospital Charsadda, KPK, Pakistan for providing research facilities.
Funding Source
None
Conflict of Interest
The authors declare no conflict of interest.
REFERENCES
- Babaley M. Pharmaceutical policy: Challenges in the supply of drugs and other health products in Africa: A mapping to sensitize funders and stakeholders. Reseau Médicaments Develop. 2009;41:10-18.
- Barber N, Rawlins M, Dean Franklin B. Reducing prescribing error: Competence, control and culture. Qual Safet Healt Care. 2003;12:29-32.
- Bavestrello L, Cabello A, Casanova D. Impact of regulatory measures in the trends of community consumption of antibiotics in Chile. Rev Med Chil. 2002;130:1265-1272.
- Calva J, Bojalil R. Antibiotic use in a peri-urban community in Mexico: A household and drug store survey. Soc Sci Med. 1996;42:1121-1128.
- Colgan R, Powers JH. Appropriate antimicrobial prescribing approaches that limit antibiotic resistance. Am Fam Physician. 2001;64:999-1004.
- Dawadi S, Rao BS, Khan GM. Pattern of antimicrobial prescription and its cost analysis in respiratory tract infection. Kathmandu Uni J Sci Engg Tech. 2005;1:1-9.
- Dean B, Schachter M, Vincent C. Prescribing errors in hospital inpatients: Their incidence and clinical significance. Qual Safe Health Care. 2002;11:340-344.
- DiMatteo MR. Variations in patients' adherence to medical recommendations: A quantitative review of 50 years of research. Med Care. 2004;42:200-209.
- Ferech M, Coenen S, Malhotra KS, Dvorakova K, Hendrickx E, Suetens C, et al. European surveillance of antibiotic consumption (ESAC): Outpatient antibiotic use in Europe. J Antimicrob Chemother. 2006;58:401-407.
- Gallagher P, Barry P, Mahoney D. Inappropriate prescribing in the elderly. J Clin Pharm Ther. 2007;32:113-121.
- Garfield S, Barber N, Walley P, Willson A, Eliasson L. Quality of medication use in primary care-mapping the problem, working to a solution: A systematic review of the literature. BMC Med.2009;7:50.
- Goossens H, Ferech M, Coenen S, Stephens P. Comparison of outpatient systemic antibacterial use in 2004 in the United States and 27 European countries. Clin Infect Dis. 2007;44:1091-1095.
- Grigoryan L, Haaijer-Rysjamp FM, Burgerhof JG, Mechtler R, Deschepper R, Tambic-Andrasevic A, et al. Self-medication with antimicrobial drugs in Europe. Emerg Infect Dis. 2006;12:452-459.
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003;362:1225-1230.
- Gwaltney JM, Bisna AL. Pharyngitis In: Mandell GL, Bennett JE and Dolin R: Principles and Practice of Infectious Diseases. Philadelphia: Churchill Livingstone. 2000;5th Edition:656-663.
- Hamadeh GN, Dickerson LM, Saab BR, Major SC. Common prescriptions in ambulatory care in Lebanon. Ann Pharmacother. 2001;35:636-640.
Citation: Akbar MT, Shah H, Faisal S, Abdulla, Shah SA, Jan F, et al. (2020) Irrational use of Antibiotics and Associated Health Risks in District Charsadda, Pakistan. J Trop Dis 8:357. doi: 10.35248/2329-891X.20.8.357.
Copyright: © 2020 Akbar MT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.