Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
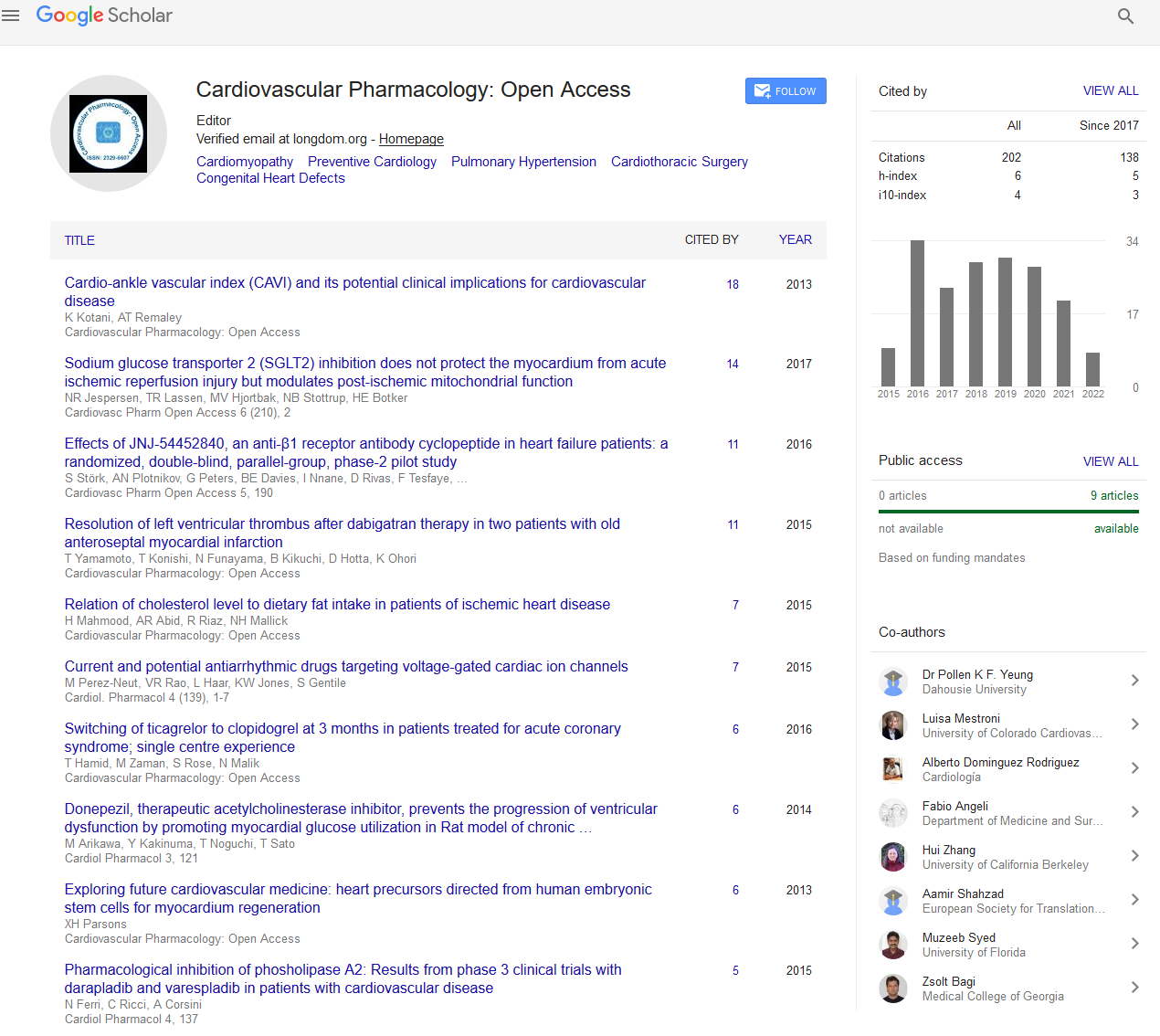
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion - (2024) Volume 13, Issue 2
Investigating the Pharmacokinetics and Pharmacodynamics of Beta-Blockers in Heart Failure Management
Xin Jiang*Received: 24-May-2024, Manuscript No. CPO-24-27316; Editor assigned: 27-May-2024, Pre QC No. CPO-24-27316 (PQ); Reviewed: 10-Jun-2024, QC No. CPO-24-27316; Revised: 18-Jun-2024, Manuscript No. CPO-24-27316 (R); Published: 26-Jun-2024, DOI: 10.35248/2329-6607.24.13.396
Description
Heart Failure (HF) is a complex, progressive condition where the heart's ability to pump blood effectively is compromised, resulting in symptoms like shortness of breath, fatigue and fluid retention. One of the fundamentals of HF management is the use of beta-blockers, which have been shown to reduce morbidity and mortality by improving cardiac function, reducing arrhythmias and enhancing overall cardiovascular stability. Understanding the Pharmacokinetics (PK) and Pharmacodynamics (PD) of beta-blockers in heart failure management is important for optimizing their therapeutic benefits while minimizing side effects.
Overview of beta-blockers in heart failure
Beta-blockers are a class of medications that inhibit the action of endogenous catecholamines, particularly norepinephrine and epinephrine, on beta-adrenergic receptors. By blocking these receptors, beta-blockers decrease heart rate, reduce myocardial oxygen demand and mitigate Sympathetic Nervous System (SNS) activation, which is often elevated in HF patients and contributes to disease progression.
In HF, chronic SNS activation leads to increased heart rate and contractility, which can eventually worsen myocardial damage and lead to further functional decline. Beta-blockers help counteract these effects by slowing the heart rate, decreasing blood pressure and reducing myocardial oxygen consumption, thus allowing the heart to function more efficiently. Key beta- blockers used in HF include carvedilol, metoprolol succinate and bisoprolol, each with unique PK and PD profiles that impact their clinical application.
Pharmacokinetics of beta-blockers in heart failure
The pharmacokinetics of beta-blockers in HF include the processes of absorption, distribution, metabolism and excretion. Each of these processes can vary between beta-blockers and is influenced by factors such as drug formulation, patient age, liver and kidney function and genetic polymorphisms.
Absorption: Oral beta-blockers are generally well-absorbed, but their bioavailability can vary widely. For instance, metoprolol has a bioavailability of about 50% due to extensive first-pass metabolism in the liver, while bisoprolol has a higher bioavailability (around 80%-90%). Carvedilol is also subject to significant first-pass metabolism, with bioavailability around 25%-35%.
Distribution: Once absorbed, beta-blockers are distributed throughout the body and cross cell membranes, affecting tissues with high beta-receptor concentrations, including the heart, lungs, kidneys and liver. The Volume of distribution (Vd) of beta-blockers varies; for example, carvedilol has a larger Vd due to its lipid solubility, allowing it to penetrate cell membranes more easily, which might contribute to its effects on peripheral vascular resistance.
Metabolism: Beta-blockers undergo extensive hepatic metabolism, primarily via Cytochrome P450 (CYP) enzymes. Metoprolol is metabolized primarily by CYP2D6, while carvedilol is metabolized by both CYP2D6 and CYP2C9. Genetic polymorphisms in these enzymes can lead to substantial interindividual variability in drug metabolism. For example, poor metabolizers of CYP2D6 may have higher plasma levels of metoprolol, increasing the risk of adverse effects, while ultra- rapid metabolizers may experience reduced efficacy.
Excretion: Most beta-blockers are excreted by the kidneys, either unchanged or as metabolites. Renal impairment, common in HF patients, can lead to drug accumulation and heightened side effects. For instance, atenolol, which is predominantly renally excreted, may require dose adjustments in patients with renal dysfunction. In contrast, carvedilol is primarily metabolized by the liver, making it more suitable for patients with renal impairment.
Pharmacodynamics of beta-blockers in heart failure
The pharmacodynamics of beta-blockers in HF are influenced by the specific receptor targets, the drug’s selectivity and its additional pharmacological properties..
Receptor Selectivity: Beta-blockers are classified based on their selectivity for beta-1 and beta-2 adrenergic receptors. Beta-1 receptors are primarily found in the heart, while beta-2 receptors are located in the lungs, blood vessels and other tissues. Cardioselective beta-blockers, such as metoprolol and bisoprolol, primarily block beta-1 receptors, minimizing adverse effects on the lungs, which is advantageous in patients with comorbid conditions like asthma or Chronic Obstructive Pulmonary Disease (COPD).
Intrinsic Sympathomimetic Activity (ISA): Some beta-blockers have Intrinsic Sympathomimetic Activity (ISA), meaning they partially activate beta receptors while blocking the effects of catecholamines. However, beta-blockers with ISA are typically avoided in HF management, as the residual beta receptor activation may counteract the benefits of sympathetic blockade.
Additional effects: Beyond beta-adrenergic blockade, certain beta-blockers exert antioxidant and anti-inflammatory effects. For instance, carvedilol has antioxidant properties that may further protect against the oxidative stress associated with HF. These additional properties may contribute to carvedilol’s superior efficacy in reducing mortality in HF compared to other beta-blockers.
Clinical implications for beta-blocker use in heart failure
The PK and PD profiles of beta-blockers underscore the need for individualized therapy in HF. Dose titration is particularly important, as beta-blockers can initially worsen HF symptoms due to their negative inotropic effect, or the tendency to decrease cardiac contractility. Starting with a low dose and gradually increasing allows the heart to adjust and avoids acute decompensation.
Monitoring for side effects such as bradycardia, hypotension and worsening fatigue is necessary, especially in the early phases of beta-blocker therapy. For patients with severe renal impairment, non-renally excreted beta-blockers like carvedilol may be preferable.
Conclusion
Beta-blockers play a vital role in the management of heart failure, helping to improve survival, reduce hospitalizations and enhance quality of life. Their effectiveness is influenced by pharmacokinetic factors like absorption, metabolism and excretion, as well as pharmacodynamic properties such as receptor selectivity and additional vasodilatory or antioxidant effects. As our understanding of genetic variability and other patient-specific factors grows, beta-blocker therapy in HF management is likely to become even more personalized, enhancing outcomes for this challenging population.
Citation: Jiang X (2024). Investigating the Pharmacokinetics and Pharmacodynamics of Beta-Blockers in Heart Failure Management. Cardiovasc Pharm. 13:396.
Copyright: © 2024 Jiang X. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.