Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2024) Volume 10, Issue 2
Integrated Palliative Care Model for Comprehensive Patient Care
Samson Rebecca*Received: 31-Jul-2020, Manuscript No. JPC-20-5776; Editor assigned: 05-Aug-2020, Pre QC No. JPC-20-5776 (PQ); Reviewed: 19-Aug-2020, QC No. JPC-20-5776; Revised: 01-Aug-2024, Manuscript No. JPC-20-5776 (R); Published: 29-Aug-2024, DOI: 10.35248/2573-4598.24.10.278
Abstract
Death is one of the harsh realities of life. It can occur in a variety of ways. Palliative care is given to patients experiencing a life limiting condition due to disease. Such people experience extreme symptoms that include physical, spiritual and psychosocial suffering. Palliative care aims to prevent and manage these symptoms while optimizing the quality of life throughout the dying process. Physical pain, psychological distress and lack of support that are faced by end of life patients require the services of a multidisciplinary team working in a variety of settings. An integrated model of palliative care delivery can help to achieve holistic palliation, peaceful death, retention of family stability and support through bereavement.
Keywords
Palliative care; Integrated model; Quality of life; Bereavement
Introduction
Improving patient care has become a priority for all health care providers with the overall objective of achieving a high degree of patient satisfaction. Greater awareness among the public, increasing demand for better care, keener competition, more health care regulation, the rise in medical malpractice litigation and concern about poor outcomes are factors that contribute to this change.
Literature Review
According to WHO, palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification, impeccable assessment and treatment of pain and other problems: Physical, psychosocial and spiritual. It does not cure but serves to mitigate the sufferings [1-3] (Figure 1).
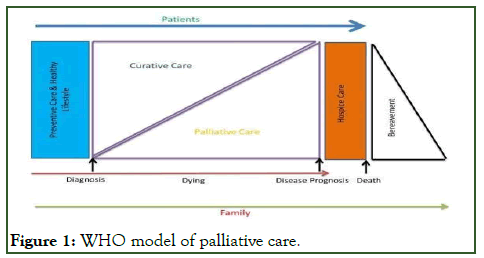
Figure 1: WHO model of palliative care.
The National Council of Palliative Care (NCPC), UK affirms life and dying as a normal process and asserts that palliative care aims to provide relief from pain and other symptoms, integrates the psychological and spiritual aspects of patient care, offers a support system to help patients live as actively as possible until death and help the family cope during the patient’s illness and in their own environment.
Myths and misconceptions
Certain myths and misconceptions surround palliative care, some of them being that it is meant only for those who are dying and have no chance for cure, that it is just meant to give us hope and enables faster death and that the pain relief measures adopted in palliative care tend to create addiction. The responsibility of allaying these misconceptions is also a role that rests with the health care staff [4].
Goals of palliative care
The essential goals of palliative care in patients with an active, progressive and far advanced disease is to maximize the quality of life, provide psychosocial and spiritual care, prevent unwanted hospital stay and to reduce financial burden to the family. Hospice care which is also a similar comfort providing service serves to differ from palliative care in that it is not initiated at the time of diagnosis and treatment of the patient but at its cessation and when it is clear that the person is not going to survive the illness [5,6].
Palliative care team
It is essential to have a multidisciplinary team with a palliative specialist at the helm to coordinate in order to provide effective service. The team comprises of physicians, nurses (for both inpatient and community care), social workers, physiotherapists, occupational therapists and chaplains or pastoral care workers.
Concept of integrated model of palliative care delivery
Since the problems faced by patient needing palliative care is diverse, requiring the services of a team and for a period of time, an integrated model of delivery is essential that would be comprehensive in nature. This model covers end-of-life patients across various settings like hospital, community and hospice. It also addresses the physical, psychological, social and spiritual components of the patient [7,8] (Figure 2).
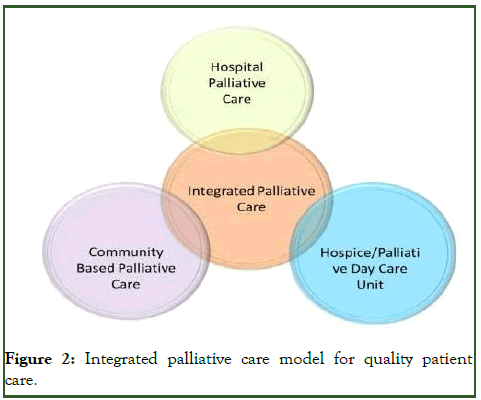
Figure 2: Integrated palliative care model for quality patient care.
Settings of palliative care delivery
In the hospital, the patient can avail consultation services from other specialties, tertiary or acute palliative care and have access to imaging, radiotherapy and lab services and also to various other pain relieving and comfort oriented modalities (Figure 3).

Figure 3: Integrated hospital palliative care services.
At the hospice/palliative day care unit, the patient can remain at home as long as possible in addition to receiving attention to all aspects of their illness and suffering i.e., to receive physiotherapy and occupational/music/art therapy; to meet with others in similar situations to themselves in a friendly social/non-clinical environment with review once in every 12 weeks.
In the community mode of palliative care service, the patient can avail services in his/her own home, at the homes of their relatives, in care homes or old age homes. The services are advisory, practical(hands-on) and multi-disciplinary team services including confirmation of diagnosis, investigations at home level, prescription of medications, involvement of home nurses in care, organization of family support and even performance of procedures such as blood transfusion, chemotherapy and physiotherapy. There are also regular visits from chaplain, physiotherapist, occupational therapist and social workers to help the clients and family to cope with the illness.
Characteristics of integrated palliative care model
The integrated palliative care model is characterized by certain features. They are as follows:
Caring attitude: It involves sensitivity, empathy, compassion and demonstrates concern for the individual. There is also a concern for all aspects of a patient’s suffering with not just the medical, nursing or social work problems.
Consideration of individuality: It is the practice of categorizing patients by their underlying disease based on the similarity of the medical problems encountered and recognizes the psychosocial features and problems that make every patient a unique individual.
Cultural considerations: It is ethnic, racial and religious and other cultural factors may have a profound effect on a patient’s suffering. The cultural differences are to be respected and treatment planned in a culturally sensitive manner.
Consent: It is the consent of a patient or those to whom the responsibility is delegated, is necessary before any treatment is given or withdrawn.
Choice of site of care: Here the patient and family need to be included in any discussion about the site of care (Hospitalized, day care center or community palliative care services).
Communication: Good communication between all the health care professionals, patients and families involved in a patient’s care is essential and is fundamental to many aspects of palliative care. There is strong evidence that such communications are less than optimal.
Clinical context: All palliative treatment should be appropriate to the stage of the patient’s disease and prognosis.
Comprehensive inter professional care: It is the provision of total or comprehensive care for all aspects of a patient’s suffering requires an interdisciplinary team.
Care excellence: It means that palliative care should deliver the best possible medical, nursing and allied health care that is available and appropriate.
Consistent medical care: consistent medical management requires that an overall plan of care to be established and regularly reviewed, for each patient. This will reduce the likelihood of sudden or unexpected alterations, which can be distressing for the patient and family. It may lessen the chance of crises or medical emergencies which can frighten the patient and relatives.
Coordinated care: It involves the effective organization of the work of the members of the inter-professional team, to provide maximal support and care to the patient and family. It also includes care planning meetings, to which all members of the team can contribute and at which the views of the patient and the family are presented, are essential to develop a plan of care for each individual patient.
Continuity of care: It is the provision of continuous symptomatic and supportive care from the time the patient is referred until death. Problems most frequently arise when patients are moved from one place of care to another and ensuring continuity of all aspects of care is most important.
Caregiver support: The relatives of patients with advanced disease are subject to considerable emotional and physical distress, especially if the patient is being managed at home. Particular attention must be paid to their needs as the success or failure of palliative care may depend on the caregivers’ ability to cope.
Continued reassessment: It is a necessity for all patients with advanced disease for whom increasing and new clinical problems are to be expected. This applies as much to psychosocial issues as it does to pain and other physical symptoms.
Discussion
An end-of-life patient faces physical, psychological, social and spiritual problems. It is usual to first alleviate the physical problems first, mainly pain, restlessness, dyspnoea and death rattle. Once the physical problems are addressed, attention shifts to the broad integrated response to tackle the other issues which are an inherent part of the dying process. It becomes more distressful when the care is fragmented and dealt in pieces and this is where the integrated model comes in handy when a coordinated and concerted effort ultimately results in greater patient satisfaction and thereby a good quality of life. Since integrated care extends beyond death to support bereavement and maintenance of family stability, this model can be proposed to be used in all settings. The expertise of the specialized health care team helps to explore how to keep up patient dignity which is true and compassionate palliation. On knowing and accepting that death is imminent, last minute acts like settling financial issues, closing relationships, saying goodbye to family and friends and forgiving are all tasks associated with a dignified death and integrated palliation aims to achieve exactly that [9-12].
Conclusion
Evidence based standards of palliative care services, focusing on improving clinical and organizational knowledge and practice are needed in all settings. Integrated palliative model for comprehensive health care guarantees a simple and low cost approach to palliation and can be implemented to reach the majority of the target population, particularly in low resource settings, where the majority of cases are diagnosed in late stages.
References
- Hospice P, Worldwide PC, Doyle D, Woodruff R. International association for hospice and palliative care.
- Payne S, Eastham R, Hughes S, Varey S, Hasselaar J, Preston N. Enhancing integrated palliative care: What models are appropriate? A cross-case analysis. BMC Palliat Care. 2017;16(1):1-0.
[Crossref] [Google Scholar] [PubMed]
- Hui D, Bruera E. Models of integration of oncology and palliative care. Ann Palliat Med. 2015;4(3):89-98.
[Crossref] [Google Scholar] [PubMed]
- Hui D, Bruera E. Integrating palliative care into the trajectory of cancer care. Nat Rev Clin Oncol. 2016;13(3):159-171.
[Crossref] [Google Scholar] [PubMed]
- Bainbridge D, Brazil K, Krueger P, Ploeg J, Taniguchi A. A proposed systems approach to the evaluation of integrated palliative care. BMC Palliat Care. 2010;9:1-2.
[Crossref] [Google Scholar] [PubMed]
- Bruera E, Hui D. Conceptual models for integrating palliative care at cancer centers. J. Palliat Med. 2012;15(11):1261-1269.
[Crossref] [Google Scholar] [PubMed]
- Muir JC, Daly F, Davis MS, Weinberg R, Heintz JS, Paivanas TA, et al. Integrating palliative care into the outpatient, private practice oncology setting. J Pain Symptom Manag. 2010;40(1):126-135.
[Crossref] [Google Scholar] [PubMed]
- Gelfman LP, Bakitas M, Warner Stevenson L, Kirkpatrick JN, Goldstein NE. Improving palliative care for patients with heart failure and their families (impact-hf2) working group. The state of the science on integrating palliative care in heart failure. J Palliat Med. 2017;20(6):592-603.
[Crossref] [Google Scholar] [PubMed]
- Hsu-Kim C, Friedman T, Gracely E, Gasperino J. Integrating palliative care into critical care: A quality improvement study. J Intensive Care Med. 2015;30(6):358-364.
[Crossref] [Google Scholar] [PubMed]
- Colombet I, Montheil V, Durand JP, Gillaizeau F, Niarra R, Jaeger C, et al. Effect of integrated palliative care on the quality of end-of-life care: Retrospective analysis of 521 cancer patients. BMJ Support Palliat Care. 2012;2(3):239-247.
[Crossref] [Google Scholar] [PubMed]
- Nelson JE, Cortez TB, Curtis JR, Lustbader DR, Mosenthal AC, Mulkerin C, et al. Integrating palliative care in the ICU: The nurse in a leading role. J Hosp Palliat Care. 2011;13(2):89-94.
[Crossref] [Google Scholar] [PubMed]
- Boss R, Nelson J, Weissman D, Campbell M, Curtis R, Frontera J, et al. Integrating palliative care into the PICU: A report from the improving palliative care in the ICU advisory board. Pediatr Crit Care Med. 2014;15(8):762-767.
[Crossref] [Google Scholar] [PubMed]
Citation: Rebecca S (2024) Integrated Palliative Care Model for Quality Patient Care. J Pat Care. 10:278.
Copyright: © 2024 Rebecca S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
