Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
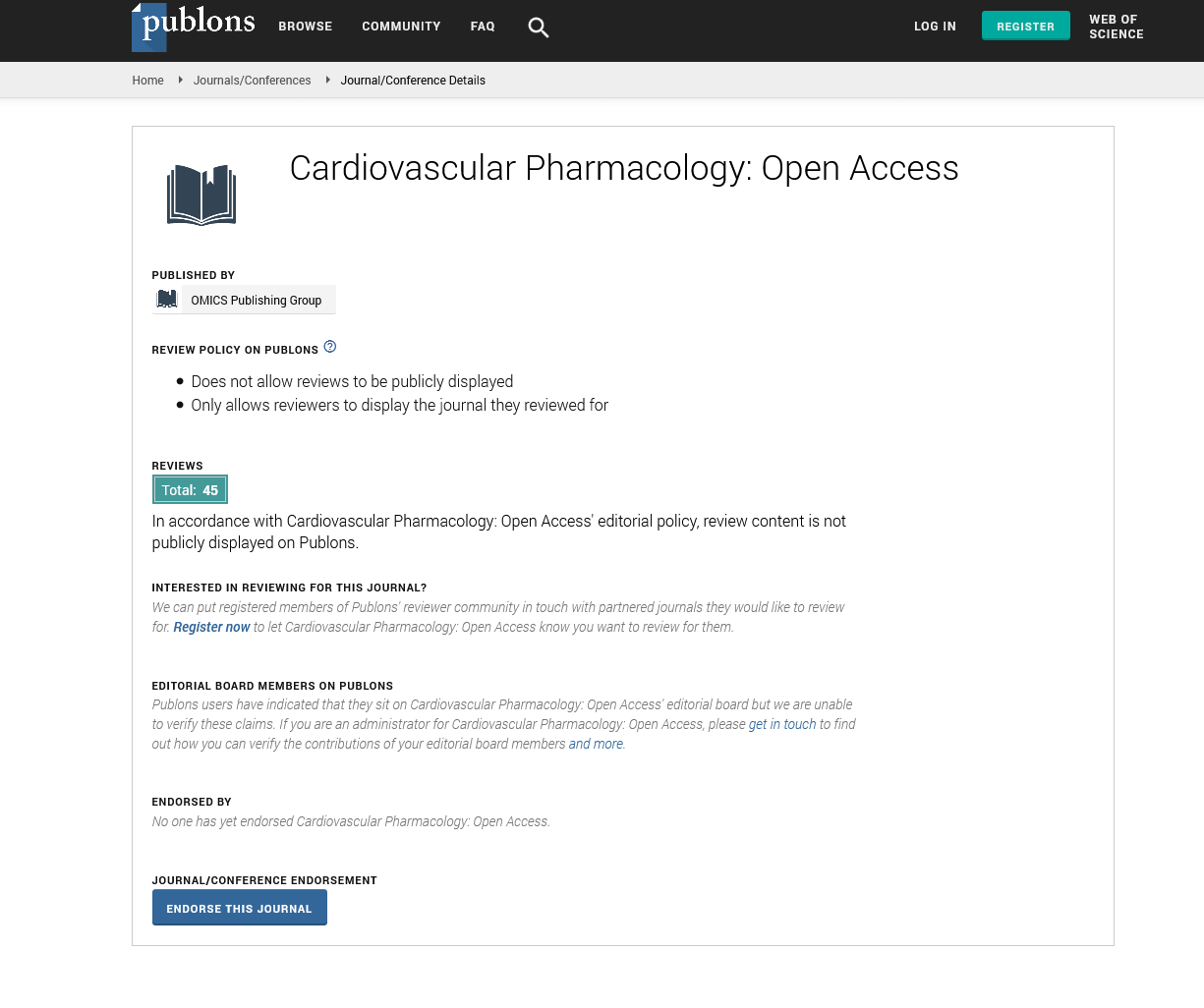
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
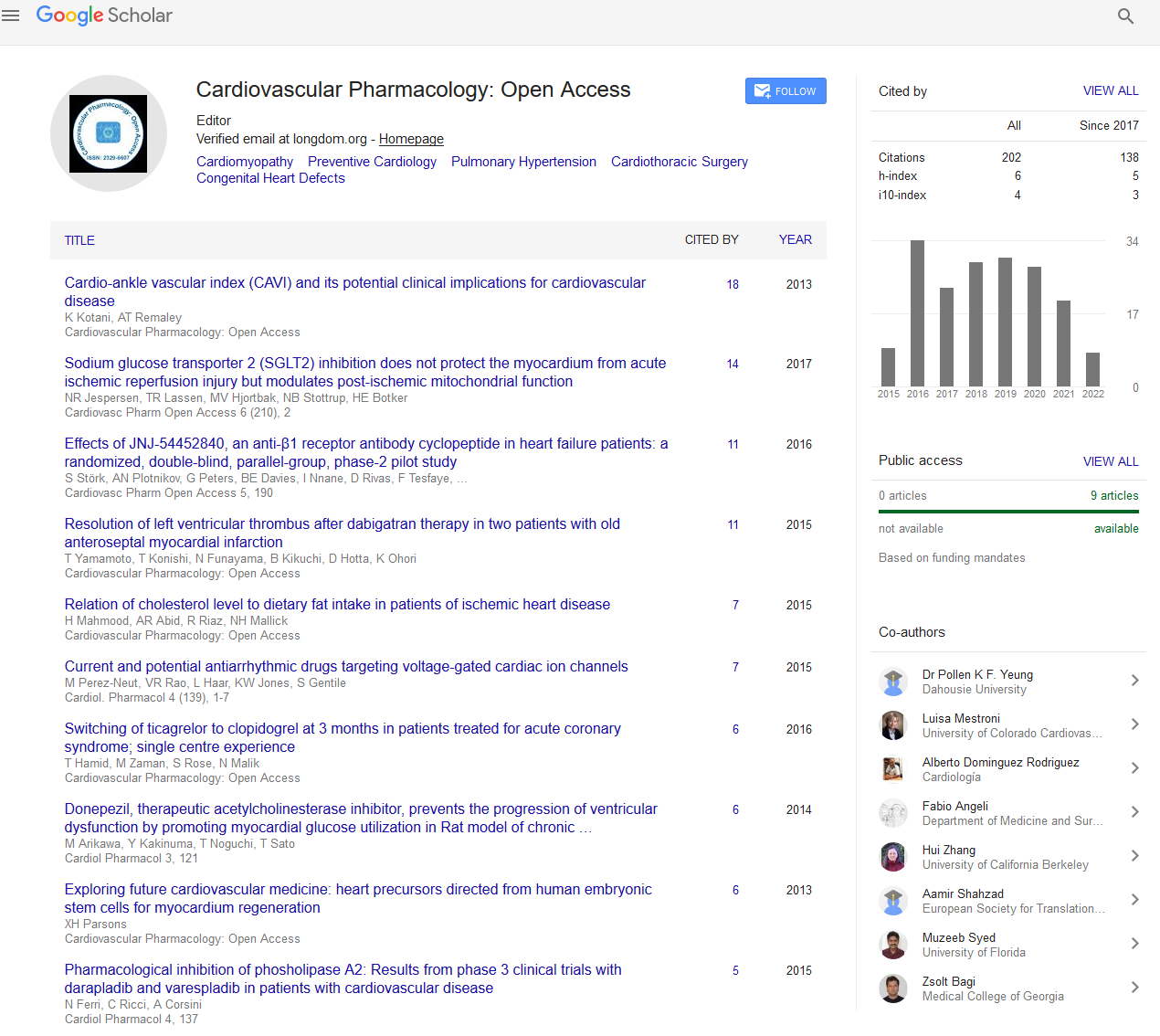
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2024) Volume 13, Issue 1
Innovative Pharmacological Techniques for the Treatment of Heart Failure
Glenn Fahey*Received: 04-Mar-2024, Manuscript No. CPO-24-25974; Editor assigned: 06-Mar-2024, Pre QC No. CPO-24-25974 (PQ); Reviewed: 21-Mar-2024, QC No. CPO-24-25974; Revised: 27-Mar-2024, Manuscript No. CPO-24-25974 (R); Published: 03-Apr-2024, DOI: 10.35248/2329-6607.24.13.383
Description
Heart Failure (HF) is a complex clinical syndrome resulting from any structural or functional impairment of ventricular filling or ejection of blood. It is a major public health issue, associated with high morbidity, mortality, and healthcare charges. Advances in cardiovascular pharmacology have significantly improved the management of heart failure, introducing novel therapeutic agents and optimizing existing treatment protocols.
Novel drug classes in heart failure management
Recent years have seen the emergence of several novel drug classes that have transformed the therapeutic countryside of heart failure. Among these, the most notable are Angiotensin Receptor-Neprilysin Inhibitors (ARNIs), Sodium-Glucose co- Transporter-2 (SGLT2) Inhibitors, and Soluble Guanylate Cyclase (sGC) stimulators.
Angiotensin Receptor-Neprilysin Inhibitors (ARNIs): Sacubitril/valsartan, the first ARNI approved for heart failure, combines the effects of neprilysin inhibition and angiotensin II receptor blockade. Sacubitril inhibits neprilysin, an enzyme that degrades natriuretic peptides, leading to increased levels of these peptides that promote vasodilation, natriuretic, and diuresis. Valsartan blocks the angiotensin II receptor, reducing the effects of the Renin-Angiotensin-Aldosterone System (RAAS), which include vasoconstriction, sodium retention, and fibrosis. This dual mechanism results in significant reductions in mortality and hospitalization for heart failure compared to traditional RAAS inhibitors.
SGLT2 inhibitors: Initially developed for diabetes management, SGLT2 inhibitors like dapagliflozin and empagliflozin have demonstrated substantial benefits in heart failure patients, regardless of diabetic status. These drugs inhibit glucose reabsorption in the renal proximal tubules, leading to glucosuria and osmotic diuresis. The resulting effects include reduced preload and afterload on the heart, improved cardiac energy metabolism, and favorable effects on cardiac remodeling. Clinical trials such as DAPA-HF and EMPEROR-Reduced have shown significant reductions in heart failure hospitalization and cardiovascular mortality with SGLT2 inhibitors.
Soluble Guanylate Cyclase (sGC) stimulators: Vericiguat is a novel sGC stimulator that enhances the Cyclic Guanosine Monophosphate (cGMP) Pathway, leading to vasodilation and improved myocardial function. By stimulating sGC independently of Nitric Oxide (NO), vericiguat addresses NO deficiency common in heart failure patients. The VICTORIA trial demonstrated that vericiguat significantly reduced the risk of cardiovascular death and heart failure hospitalization in patients with worsening heart failure.
Mechanisms of action: Insights into therapeutic benefits
Understanding the mechanisms of action of these novel agents is crucial for optimizing their use in clinical practice. The distinct pathways targeted by ARNIs, SGLT2 inhibitors, and sGC stimulators provide complementary benefits in heart failure management.
ARNIs: By inhibiting neprilysin and blocking the angiotensin II receptor, ARNIs enhance natriuretic peptide activity while mitigating the adverse effects of RAAS activation. This dual action results in reduced cardiac remodeling, decreased ventricular stiffness, and improved overall cardiac function.
SGLT2 inhibitors: These drugs reduce heart failure symptoms through multiple mechanisms, including osmotic diuresis, reduced interstitial edema, improved ventricular loading conditions, and beneficial effects on myocardial energy utilization and fibrosis. Their glucose-lowering effects are secondary to their cardiovascular benefits.
sGC stimulators: By increasing cGMP levels, sGC stimulators promote vasodilation and improve endothelial function. This leads to decreased systemic vascular resistance and reduced myocardial oxygen demand, ultimately enhancing cardiac output and reducing heart failure symptoms.
Citation: Fahey G (2024) Innovative Pharmacological Techniques for the Treatment of Heart Failure. Cardiovasc Pharm. 13:383.
Copyright: © 2024 Fahey G. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.<