Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
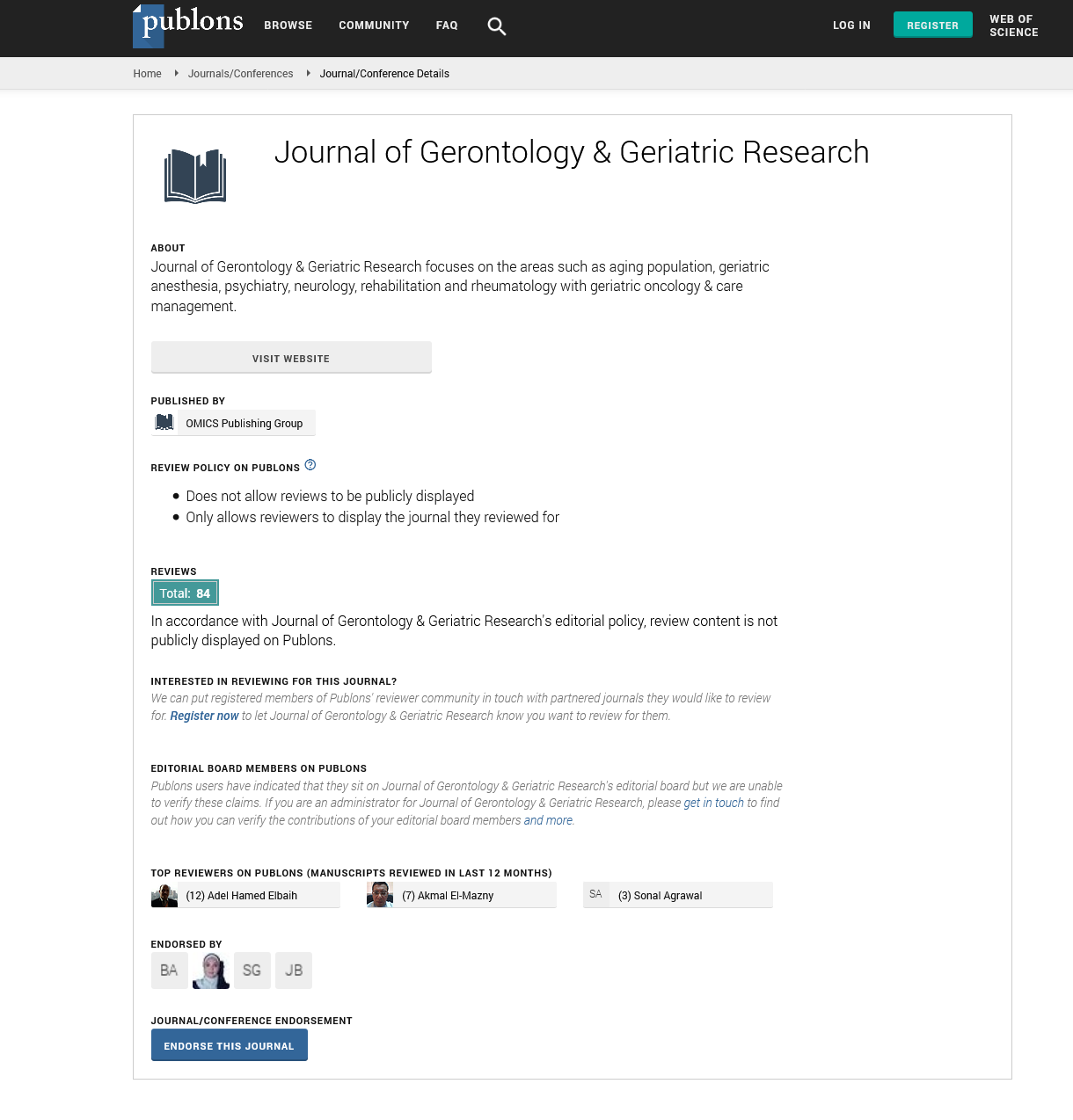
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Mini Review - (2024) Volume 13, Issue 2
Innovations in Palliative Care: Addressing the Unique Needs of the Aging Population
Frazee Bradley*Received: 01-Apr-2024, Manuscript No. jggr-24-25833; Editor assigned: 02-Apr-2024, Pre QC No. P-25833; Reviewed: 16-Apr-2024, QC No. Q-25833; Revised: 22-Apr-2024, Manuscript No. R-25833; Published: 30-Apr-2024, DOI: 10.35248/2167-7182.2024.13.730
Abstract
This article discusses the ethical challenges in conducting research with older adults, focusing on issues such as informed consent, risk-benefit analysis, and the inclusion of vulnerable populations. It provides guidelines for ethical research practices aimed at protecting the rights and well-being of elderly participants. As our global population ages, the demand for quality palliative care continues to rise. Palliative care, often associated with end-of-life support, extends far beyond that narrow perception. It encompasses a holistic approach to enhancing the quality of life for individuals facing serious illnesses, focusing on physical, emotional, and spiritual well-being. With advancements in medical technology and evolving societal attitudes toward aging, innovations in palliative care are playing a pivotal role in meeting the unique needs of the aging population.
Keywords
Palliative care; Medical technology; Aging population
Introduction
One of the most significant innovations in palliative care is the shift toward personalized care plans. Recognizing that each individual's journey is unique, healthcare providers now tailor palliative care interventions to address specific needs and preferences. This personalized approach considers factors such as cultural background, spiritual beliefs, and personal values, ensuring that the care provided is not only effective but also respectful of individual dignity and autonomy.
The advent of telemedicine has revolutionized the delivery of palliative care, particularly for elderly patients who may have limited mobility or live in remote areas. Through telemedicine platforms, healthcare professionals can conduct virtual consultations, monitor symptoms, and provide timely interventions without the need for patients to travel long distances. Remote monitoring devices, such as wearable sensors and smart home technology, enable continuous assessment of vital signs and early detection of health issues, enhancing proactive management of symptoms and improving overall quality of life.
Technology plays a pivotal role in enhancing the delivery of palliative care to the aging population. From advanced pain management techniques to virtual reality therapy for psychological distress, innovative technologies are providing new avenues for symptom relief and emotional support. For example, robotic companions and AI-driven chatbots offer companionship and assistance with daily tasks, alleviating feelings of loneliness and isolation often experienced by elderly individuals with serious illnesses.
Effective palliative care requires collaboration among various healthcare professionals, including physicians, nurses, social workers, psychologists, and spiritual counselors. Innovations in palliative care are fostering interdisciplinary teamwork, with specialized teams working together to address the complex needs of aging patients. By pooling expertise from different fields, healthcare providers can offer comprehensive support that considers not only medical needs but also psychosocial and spiritual aspects of care.
Advance care planning empowers individuals to express their preferences for medical treatment and end-of-life care while they are still capable of making decisions. Innovations in advance care planning tools, such as electronic health records and digital platforms, enable patients to document their wishes, appoint healthcare proxies, and engage in meaningful conversations with their families and healthcare providers [1-3]. By facilitating proactive communication and decision-making, advance care planning helps ensure that aging individuals receive care that aligns with their values and goals.
Literature Review
Recognizing the importance of providing palliative care in familiar environments, there is a growing emphasis on community-based palliative care services. These programs bring comprehensive support directly to patients' homes, enabling them to receive highquality care while remaining in familiar surroundings surrounded by loved ones. Community-based palliative care teams coordinate with primary care providers, hospice agencies, and other community resources to deliver holistic support tailored to the unique needs of each individual and their family.
Innovations in palliative care are transforming the landscape of aging care, offering new approaches to support the physical, emotional, and spiritual well-being of elderly individuals facing serious illnesses. From personalized care plans to advanced technologies and community-based services, these innovations are enhancing the quality of life for aging patients and their families. By embracing these advancements and fostering interdisciplinary collaboration, we can ensure that palliative care remains responsive to the evolving needs of our aging population, promoting dignity, comfort, and compassion for all.
The NIA, part of the National Institutes of Health, provides research and resources focused on aging-related issues, including palliative care. Their website offers information on funding opportunities, research findings, and programs related to aging and end-of-life care. CAPC is a national organization dedicated to increasing access to quality palliative care for people living with serious illness. Their website provides resources for healthcare professionals, including educational materials, training programs, and tools for implementing palliative care in various settings.
AAHPM is a professional organization for healthcare professionals specializing in hospice and palliative medicine. Their website offers resources, educational events, and publications related to palliative care for aging populations. This peer-reviewed journal publishes research and clinical articles on palliative care, including innovations in care delivery, symptom management, and end-of-life support for older adults. Subscribing to this journal can provide access to the latest research and advancements in the field.
Discussion
IAHPC is a global organization dedicated to promoting palliative care education, research, and advocacy worldwide. Their website offers resources, training opportunities, and information on global initiatives to improve palliative care for aging populations. AARP is a non profit organization focused on issues affecting older adults. Their website features articles, guides, and resources on end-oflife planning, caregiving, and aging-related healthcare options, including palliative care. HPNA is a professional organization for nurses specializing in hospice and palliative care. Their website offers educational resources, certification programs, and networking opportunities for nurses working with aging patients and their families.
Exploring these resources can provide you with more in-depth information on innovations in palliative care and strategies for addressing the unique needs of the aging population. The NIA is a branch of the National Institutes of Health focused on aging research, including palliative care. Researchers and healthcare professionals can access information on NIA-funded studies, clinical trials, and publications related to palliative care for older adults.
The NIA's website offers resources for caregivers, patients, and families, including guidance on end-of-life decision-making and supportive care options. CAPC is a leading organization dedicated to improving the quality of palliative care across healthcare settings. Healthcare professionals can access online courses, webinars, and toolkits designed to enhance their palliative care skills and knowledge. CAPC offers resources for healthcare administrators and policymakers, including guidance on integrating palliative care into healthcare organizations and measuring quality outcomes.
AAHPM provides education, advocacy, and professional development opportunities for physicians and healthcare professionals specializing in hospice and palliative medicine. Members have access to research publications, clinical guidelines, and networking opportunities through conferences and events. AAHPM offers certification programs for healthcare professionals seeking advanced training in palliative care [4,5].
The Journal of Palliative Medicine is a peer-reviewed publication that covers a wide range of topics in palliative care, including innovations in care delivery and symptom management. Researchers and clinicians can access original research articles, case studies, and reviews on palliative care interventions for aging populations. Subscribing to the journal provides access to the latest advancements and evidence-based practices in palliative care. IAHPC is a global organization dedicated to promoting palliative care education, research, and advocacy worldwide. Members have access to resources, webinars, and educational materials on palliative care best practices and global initiatives.
IAHPC collaborates with international partners to support palliative care development in low- and middle-income countries, addressing disparities in access to end-of-life care. AARP offers resources and information on a wide range of aging-related topics, including endof- life planning and palliative care options. Caregivers and older adults can access articles, guides, and online tools to navigate healthcare decisions and advance care planning. AARP advocates for policies that support aging populations, including access to palliative care services and caregiver support programs.
HPNA provides education, certification, and networking opportunities for nurses specializing in hospice and palliative care. Nurses can access online courses, conferences, and publications to enhance their palliative care skills and knowledge. HPNA advocates for nursing practice standards and policies that promote quality end-of-life care for patients and families. Each of these resources offers valuable information and support for healthcare professionals, researchers, patients, and caregivers involved in palliative care for the aging population [6].
By leveraging these resources, stakeholders can stay informed about the latest innovations, best practices, and advocacy efforts in the field of aging and end-of-life care. To provide more specific information, could you please specify the aspect of palliative care or the aging population you would like to explore further? Are you interested in specific innovations, research findings, best practices, policies, or any other aspect related to palliative care and aging? Let me know, and I'll tailor the search to your preferences.
Conclusion
Innovations in palliative care are transforming the landscape of aging care, offering new approaches to support the physical, emotional, and spiritual well-being of elderly individuals facing serious illnesses. From personalized care plans to advanced technologies and community-based services, these innovations are enhancing the quality of life for aging patients and their families. By embracing these advancements and fostering interdisciplinary collaboration, we can ensure that palliative care remains responsive to the evolving needs of our aging population, promoting dignity, comfort, and compassion for all.
Acknowledgement
None.
Conflict of Interest
None.
References
- Smith T, Gildeh N, Holmes sC. The montreal cognitive assessment: Validity and utility in a memory clinic setting. Can J Psychiatry. 2007;52:329-332.
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: A preliminary report. "J Psychiatr Res.1982; 17:37-49.
- Coelho EM, Da Mota MP, Fonseca SC, Matos AP, Carvalhal MI. Exercise with music: An innovative approach to increase cognition and reduce depression in institutionalized elderly. Rev Psicol Deporte. 2020; 29:49-56.
- Jung YH, Lee S, Kim WJ, Lee JH, Kim MJ, Han HJ. Effect of integrated cognitive intervention therapy in patients with mild to moderate Alzheimer's disease. Dement Neurocogn Disord 2020;19:86.
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695-699.
- Feigin VL. Global burden of stroke and risk factors in 188 countries, during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016; 15:913-924.
Citation: Bradley F (2024). Innovations in Palliative Care: Addressing the Unique Needs of the Aging Population. J Gerontol Geriatr Res. 13: 730.
Copyright: © 2024 Bradley F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.