PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
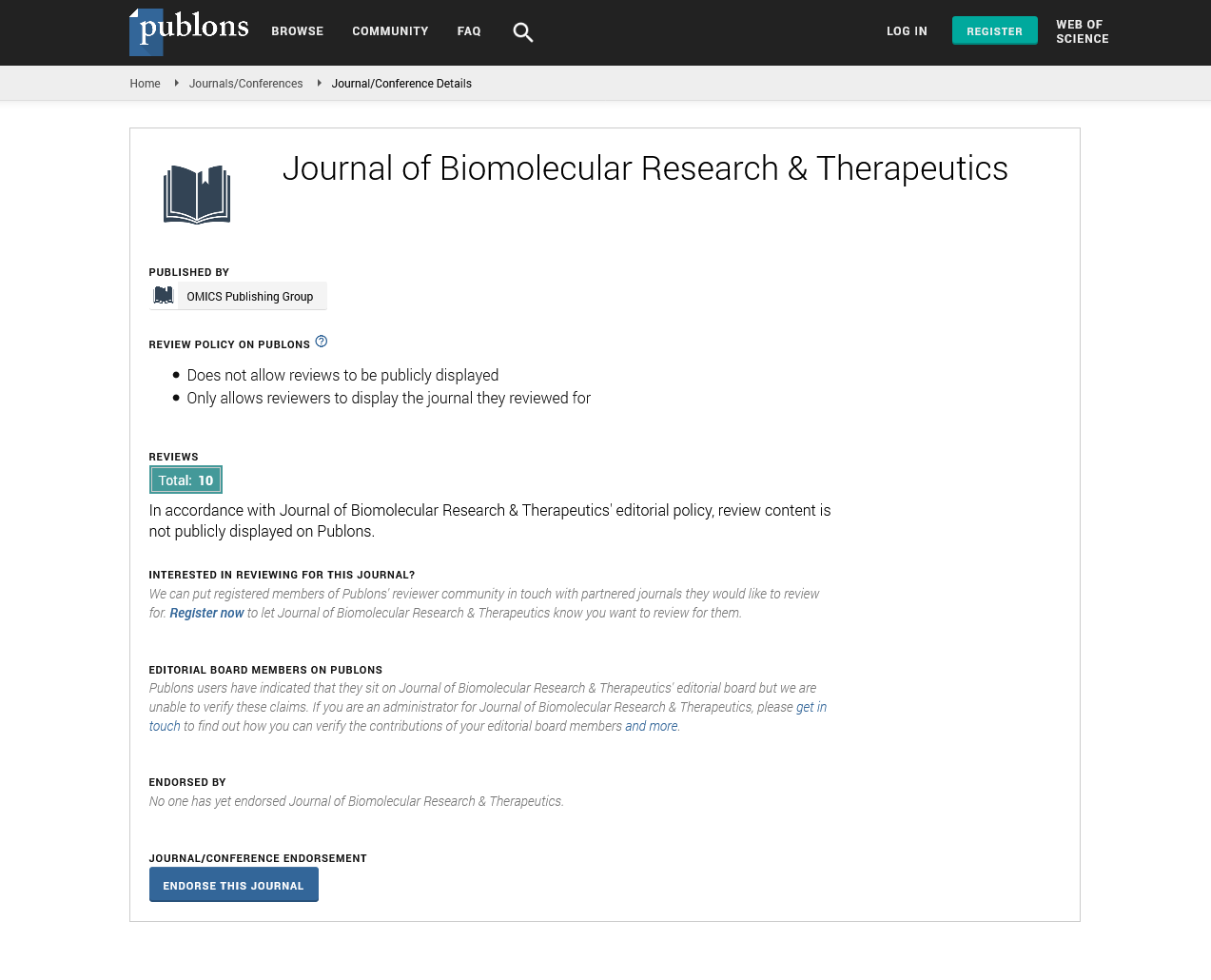
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2023) Volume 12, Issue 4
Importance of Electrochemical Biosensors in Glycine Metabolism
Davidson Bunte*Received: 03-Apr-2023, Manuscript No. BOM-23-21234; Editor assigned: 06-Apr-2023, Pre QC No. BOM-23-21234(PQ); Reviewed: 20-Apr-2023, QC No. BOM-23-21234; Revised: 27-Apr-2023, Manuscript No. BOM-23-21234(R); Published: 05-May-2023, DOI: 10.35248/2167-7956.23.12.281
Description
The regulation of the body's overall metabolism, which is necessary for human health, growth, development and survival, is a major function of Amino Acids (AAs). Glycine is the smallest Amino Acid (AA) because it only has one hydrogen atom in its side chain. Glycine makes up about 20% of the AA nitrogen in body proteins and approximately 11.5% of all AAs [1]. As a result, glycine has a strong correlation with a variety of human illness states making it one of the most appealing analyses for clinical applications [2]. While glycine may be endogenously biosynthesized in the human body, especially in the liver and kidneys it was formerly thought of as a non essential AA. This notion was supported by isotopic investigations that demonstrated how glycine over occurs during bodily metabolism, resulting in glycine changing into various chemicals and moving to various body regions.
However, the quantity of glycine that the body can synthesize on its own is insufficient to support body activity hence glycine is typically classified in present AA classifications as a conditionally necessary (or semi-essential) AA [3]. Nutritionally dietary glycine deficiency is not harmful but a chronic deficiency can have serious impacts on how the body functions including subpar growth weakened immunological responses and other negative effects on health and nutrient metabolism [4]. Furthermore glycine supplementation has been shown to enhance results in a wide range of clinical situations [5]. This is because it may assist to reduce the toxicity of some medications slow the growth of tumors and prevent the infiltration of inflammatory cells, among other things.
The framework of many structural proteins such as collagen fibrils and elastin and common metabolites such as glutathione, creatine, porphyrins, purines, heme and serine are built using glycine as the smallest and the only Non-Chiral Amino Acid (AA) [6]. Glycine also provides the flexibility required for conformational changes in the active sites of some specific enzymes. As a result glycine plays a variety of physiological roles in three essential processes cytoprotection, anti-inflammatory reactions and body growth and development [7].
Since many glycine-related ailments are linked to both its synthesis and catabolism any alteration to any of these processes may result in severe symptoms in the affected person. Until now, efforts have been focused on establishing a link between glycine levels and disease states which is a condition where there is an abnormally high level of glycine in the blood [8]. The glycine is one of the most studied macromolecules for clinical uses given the great variety of glycine activities and their participation in numerous biological processes. The current gold standard analytical method for glycine detection in the clinical field entails sample extraction (typically from blood and/or urine) and chromatographic or fluorometric analyses in centralized laboratories which causes significant delays in the delivery of results as well as high financial costs [9]. As a result there is a definite need for the development of trustworthy Point-Of-Care (POC) glycine detection technologies that can offer real-time information on a patient's health status. The construction of POC glycine platforms is currently being hampered by a number of analytical challenges. As a potential solution, electrochemical bio sensing is proposed. However, glycine has not been routinely detected in these fluids and there is little readily available clinical data addressing the amounts of glycine in humans. Additionally plasma and serum which are blood-derived fluids are frequently used in place of whole blood. Although these two matrices appear to exhibit comparable traits, due to various pre-treatment techniques their AA levels are not the same [10]. Current clinical glycine analysis generally prefers the use of plasma over serum in order to eliminate potential interferences.
References
- Azadi P, Inderwildi OR, Farnood R, King DA. Liquid fuels, hydrogen and chemicals from lignin: A critical review. Renew. Sustain. Energy Rev. 2013; 21:506-523.
- Bang G. Energy security and climate change concerns: Triggers for energy policy change in the United States? Energy Pol. 2010;38(4):1645-1653
- Carpio LG, de Souza FS. Optimal allocation of sugarcane bagasse for producing bioelectricity and second generation ethanol in Brazil: Scenarios of cost reductions. Renew. Sustain. Energy. 2017; 111:771-780
- de Assis Castro RC, Fonseca BG, dos Santos HT, Ferreira IS, Mussatto SI, Roberto IC. Alkaline deacetylation as a strategy to improve sugars recovery and ethanol production from rice straw hemicellulose and cellulose. Ind. Crop. Prod. 2017; 106:65-73.
- Medina JD, Alomia FB, Magalhaes Jr AI, de Carvalho JC, Woiciechowsky AL, Soccol CR. Simulation of different biorefinery configuration including environmental, technical and economic assay using sugarcane bagasse. J. Clean. Prod. 2021; 316:128162
- de Moraes Dutenkefer R, de Oliveira Ribeiro C, Mutran VM, Rego EE. The insertion of biogas in the sugarcane mill product portfolio: A study using the robust optimization approach. Renew. Sustain. Energy Rev. 2018; 91:729-740.
- Dias MO, Cunha MP, Jesus CD, Rocha GJ, Pradella JG, Rossell CE, et.al Second generation ethanol in Brazil: can it compete with electricity production? Bioresour. Technol. 2011; 102(19):8964-71
[Crossref] [Google Scholar] [PubMed]
- Dias MO, Junqueira TL, Cavalett O, Cunha MP, Jesus CD, Rossell CE, et.al. Integrated versus stand-alone second generation ethanol production from sugarcane bagasse and trash. Bioresour. Technol. 2012; 103(1):152-161.
[Crossref] [Google Scholar] [PubMed]
- Alvira P, Tomás-Pejó E, Ballesteros M, Negro MJ. Pretreatment technologies for an efficient bioethanol production process based on enzymatic hydrolysis: a review. Bioresour. Technol. 2010; 101(13):4851-4861
[Crossref] [Google Scholar] [PubMed]
- Duval A, Lawoko M. A review on lignin-based polymeric, micro-and nano-structured materials. React. Funct. Polym. 2014; 85:78-96
Citation: Bunte D (2023) Importance of Electrochemical Biosensors in Glycine Metabolism. J Biol Res Ther. 12:281.
Copyright: © 2023 Bunte D. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.