Indexed In
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Access to Global Online Research in Agriculture (AGORA)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- SWB online catalog
- Publons
- Euro Pub
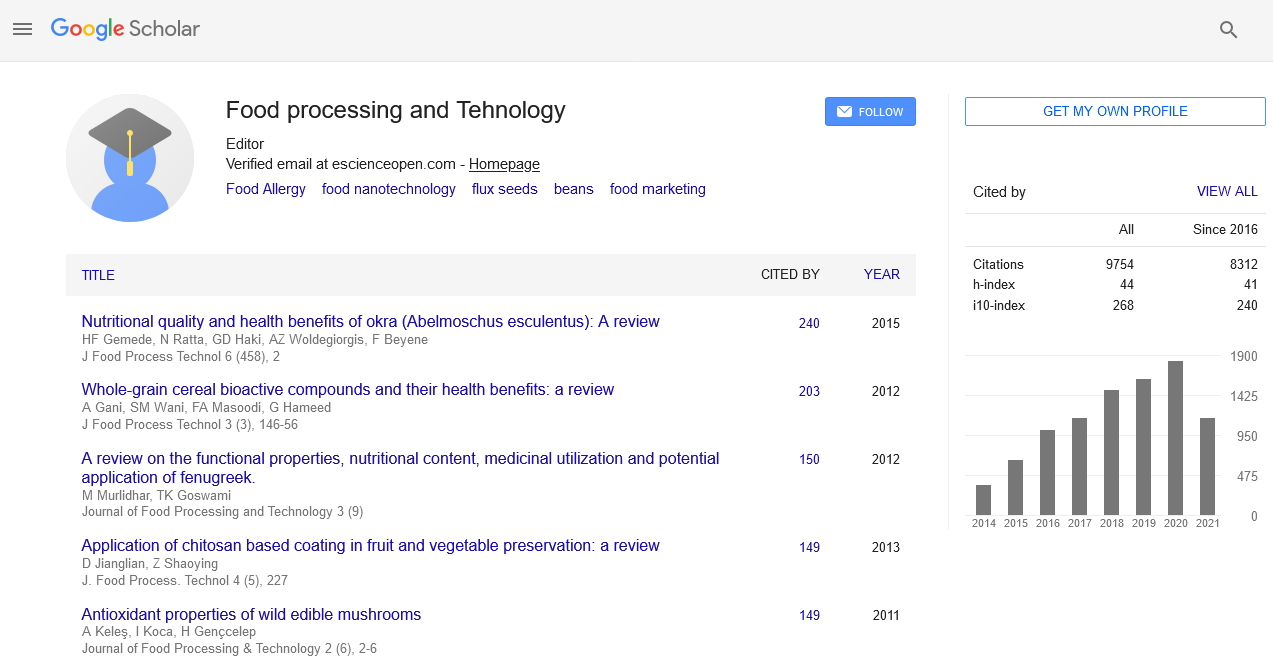
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2020) Volume 11, Issue 6
Implementing Nutrition in Cancer Care
Călescu Roxana*Received: 01-Jun-2020 Published: 10-Jul-2020, DOI: 10.35248/2157-7110.20.11.830
Abstract
Nutrition care alongside with pharmacological care is rarely used in East-Europe. Even though many physicians have seen dieticians integrated in the medical team in other countries doing that in their own countries is still a neglected procedure from many points of view.
The little number of dieticians that are integrated in the medical team in Romania normally consults all types of patients when it comes to pathologies. This can be a complicated mission, but a great challenge of achieving much medical knowledge.
But actually not getting integrated in the medical team can be the main problem. There are many patients that are not motivated by their physician to get the help of a dietician and, on the other side, patients that think they can handle their diet without the help of a dietician. But one thing is sure, once they make their first visit to the dietician they are very pleased to have someone that actually listen and advise them about their food choices.
Keywords
Cancer; Oncologist; Registered Dietician Nutritionist (RDN); Diet; Nutrition
Introduction
Cancer treatment is the main factor that influences many of the changes in the patient ’ s diet. Having side effects due to a treatment can really make you have a hard time in choosing the right food and getting advice from a dietician is exactly what you need.
Many people skip or avoid for a long time many nutritious dishes just because they know what they have to avoid, but not what to replace them with. Nobody knows that better than a dietician, whom not only will tell you what to eat instead, but also the exact amount and frequency of the foods you have to include in your diet when you are feeling sick (e.g., nausea, vomiting, diarrhoea, constipation).
It is helpful to have a weightier that measures the skeletal muscle mass, fat mass and metabolic rate in order to understand the changes that are happening at every examination, and to know what should be increased in the diet plan (proteins, fats, lipids, vitamins, minerals).
There are different types of patients in cancer when it comes to nutritional status. The first category, and unfortunately the most common one found in head and neck, lung and gastric cancer is cancer related malnutrition, a fast and hard to reverse weight lost, in which a dietician should fight first for maintaining the patient’s actual weight if he has lost ~5% in the last 6 months.
The second one would be the patients; mostly females treated for breast, endometrial and ovarian cancer which either gains or maintain an overweight or obese Body Mass Index (BMI). This means that you could find some common points in many of the patients, if we widely analyse them, but when it comes to eating each and every of them have different preferences, numbers of meals, quantities of food, foods that they like or dislike, food restrictions due to their diagnosis but not last, appetite influenced by the side effects of their cancer treatment.
Results and Discussion
The number of newly cancer diagnosed in 2017 was 1.7 million new cases [1], but cancer screening, early detection and treatment have reduced the annual number of deaths to 600.920 in the same year [1,2]. In order to manage complications due to disease focus has been increased on ameliorating symptoms through the cancer evolution [3].
The main aim of cancer treatment is to heal, monitor or alleviate, and on the other hand the role of nutritional support through the cancer pathway is to manage the needs and treatment goals [1-4]. All cancer patients may encounter malnutrition through the cancer trajectory even since the diagnosis [5,6]. Malnutrition has been identified in 15%-20% of all cancer patients at diagnosis, in 80% of those with advanced cancer, and (85-90)% of patients in terminal phase [7,8]. Malnutrition has been related with reduced response to chemotherapy, a negative impact on quality of life, and high mortality [9,10] being the cause of death in cancer of (20-30)% cases [7,8]. Losing 5% of the initial body weight before the diagnostic or starting the treatment has been predictor for early death no matter the cancer stage [10-12].
The main reasons of the risk for malnutrition in cancer and cancer related treatment are higher request for energy, which leads every biological response and all primary processes of the human body, including cardiopulmonary and immune responses [2,7].
The Academy of Nutrition and Dietetics and American Society of Parenteral and Enteral Nutrition defined malnutrition as having ≥ 2 of the following characteristics: lowered energy intake, weight loss, waste of muscle mass, waste of subcutaneous fat, edemas and lowered performance status by hand grip strength [13].
The mechanism of cancer is represented by hyper metabolic changes by releasing catabolic hormones and inflammatory cytokines that hold back protein synthesis and make increasing the lean body mass more difficult (e.g., ubiquitine-proteasome, complex acute-phase proteins, IL-6) [14-18]. In some types of cancers, functional and mechanical issues may impair the ability to eat or absorb nutrients (e.g., gastrointestinal and head and neck cancers) [15,19]. Some of the patients have different eating habits, appetite, culture and perception of tastes depending on the area they come from [20]. The initial nutritional status before diagnosis is important because patients may require additional macronutrients (carbohydrates, proteins, fats) and micronutrients (vitamins and minerals) before and during treatment. Higher initial intake of soy protein, omega-3 fatty acids, green tea, tomatoes have been associated with reducing cancer risk, compared to higher animal fat and beta-carotene that showed increased risk [14].
The type of treatment recommended for treating cancer (e.g., surgery, chemotherapy, radiation, hormone therapy, immunotherapy, biological therapy, target therapy, transplantation, or any of them combined) can affect appetite, taste, absorption, and loss of nutrients. Treatment’s side effects, like mucositis, nausea or vomiting, diarrhoea or constipation enhance the risk of malnutrition [21].
The National Comprehensive Cancer Network created a Palliative Care Guideline in which cancer cachexia and anorexia have been recognized as a concern of palliative care [13]. Diagnosing pre-cachexia or mild cachexia at its early-onset could help clinicians in to prevent moderate or severe cachexia [22-24].
Cancer cachexia is the type of progressive syndrome manifested by systemic inflammation, continuously waste of skeletal muscle mass (with or without waste of fat mass) with a negative protein/ energy balance [16]. Cancer cachexia is characterized by anorexia and weight lost and cannot be completely reversed by the conventional nutrition counselling [13,17]. Finally, cachexia leads to generalized weakness, cardiorespiratory weakness, delayed wound healing, affected immune system and on-going functional impairment [15,16,21].
Globally, it is estimated that ~2 million people will die every year due to the consequences of cancer related cachexia. Cachexia can be found in approximately 50% of all cancer patients, and is characterized by severe body weight lost, with skeletal muscle proteins waste of approximately 75% when the patients already lost 30% of body weight. Muscle wasting is one of the most important phenotypic characteristic of cancer cachexia, even though not much success has been achieved in reversing or preventing this catabolic process. When we talk about the elderly, the combination of age-related muscle loss (sarcopenia) and cancer diagnosis (with cachexia at the disease onset) is considered a metabolic challenge that older skeletal muscle is not able to do because of metabolic abnormalities like increased glucose turnover, increased lipolysis and insulin resistance, deregulated hormone housekeeping (hypogonadism), decreased muscle protein net balance, elevated cytokines and elevated acute-phase protein synthesis [25]. All of these factors can cause metabolic syndrome in the nutritionally compromised elderly, with the concomitant impairment of cancer therapy and quality of life. Therefore, it is needed that physicians and scientists to insure targeted nutritional support offered by a RDN in order to control the involuntary weight loss and death through the cancer treatment [26].
There have been eyes set on cancer survivors agreeing that reducing the recurrence of the disease consists in a healthy lifestyle based on healthy diet, normal weight and exercise in order to reduce cancer recurrence and death [27]. In order to do so, the nutrition experts, RDNs are well prepared to advice the patients in order to implement and apply healthy lifestyle interventions for those at high-risk for developing cancer, for cancer patients and for those who survived cancer. Early implementation of nutrition has benefits in improving quality of life and reducing future cancer risks [28]. RDN’s working with cancer patients have to develop specific knowledge, information, competencies and venue in order to provide safe and effective nutrition support in each stage of cancer (prevention, treatment and survivorship) [29].
An RDN has to provide oncology nutrition and dietetics care and services, to self-evaluate hers or his proper knowledge, information and venue in order to assure a safe and effective oncology nutrition and dietetics practice, to improve the topics in which better knowledge, information and venue are needed to become a competent, proficient or expert practitioner of oncology nutrition and dietetics. RDN’s must also create a base for public and professional accountability in oncology nutrition and dietetics support and facilities; sustain efforts for strategic planning, achievement and notification of oncology nutrition and dietetics facilities and resources; improve professional identity and ability in communicating the kind of oncology nutrition and dietetics care and services; to control the development of oncology nutrition and dietetics related education and on-going education programs, job descriptions, practical guidelines, skills evaluation tools and career pathways; and to attend educators and preceptors in teaching students and interns the knowledge, competencies and venue needed to work in oncology nutrition and dietetics and the understanding of the full role of applying it in cancer care [30].
A RDN can help patients with hyper metabolic conditions, such as cancer or undergoing cancer treatment [31]. The first step is to provide them more proteins, which are the main source of calories used in energy conversion. In order to manage hyper metabolism that occurs in stress and illness, patients need additional proteins [31]. Calculating the caloric/energetic needs for adults are assessed by current condition and custom body weight. A healthy person normally needs (25-30) kcal/kg/day; those that have to gain weight need (30-40) kcal/kg/day, while obese ones need (21-25) kcal/kg/day [8,31]. Another thing that must be taken in consideration is hydration because of the electrolyte balance, which maintains normovolemia and avoids dehydration [6,8]. Modalities of measuring hydration status are weight measurement, intake/discharge, edema, skin analyses, oral analyses and respiratory status [32]. Moderate dehydration can make patients manifest fatigue, xerostomia, dizziness, constipation and nausea amplified by cancer and treatment specific side effects such as nausea¸ vomiting¸ diarrhoea, ascites and fever [33]. The calculation of the fluid needs is (30-35) ml/kg.
When it comes to intervening with nutritional support the cancer type and stage are taken into consideration, as well as the treatment applied [8,34]. Two important targets of nutritional therapy are maintaining adequate calories, proteins, fluids, general nutrition status and preventing or dealing with cancer treatment side effects [3]. Early nutritional support identifies patients at risk of malnutrition and avoids nutritional impairment as encountered in cachexia [6].
Promoting a good nutritional support through the cancer pathway is equivalent with preventing malnutrition. The nutritional support must be centred on physical evaluation, weight monitoring, appetite, gastrointestinal modifications such as nausea, vomiting, diarrhoea, mucositis, and constipation [8]. Healthy diet with an adequate intake of proteins and proper hydration, combined with physical activity, of 150 minutes of moderate activity every week, are key factors for a longer survival [34]. If at the implementation of the treatment the patients are malnourished, the amount of protein calories must be increased [8,35]. The simplest way to achieve this target is by eating 6 small meals through the day with an adequate hydration. If nutritional requirements are not accomplished, the traditional oral supplements (e.g., Boost, Boost Control, Glucerna, Nutricomp, Nutridrink) might not be suitable because of the high amount of fructose and the gastrointestinal effect of carrageenan [31,36]. Organic supplements with a lower sugar content and carrageenan free provide better quality as protein source. Protein can be added in cooked meals as pea protein, hemp or whey supplements [8,34]. There are patients that believe certain foods can heal cancer. A RDN must modulate this discussion toward healthy diet, proper energy/protein intake and prevention of muscle atrophy and deconditioning due to the disease [35,37].
There are studies that show a lower risk for some cancers and chronic disease (e.g., heart disease, diabetes) [38-42] by consuming a variety of fruits, vegetables, seeds, legumes, whole grains, herbs and spices. These aliments are rich in antioxidants (vitamin A, C, E) that could pre- vent cancer and cellular deterioration. Care is needed, anyways, because of the concerns that antioxidants may lower the efficiency of some cancer treatment [43]. Before the use of any antioxidant it is better to communicate with the oncologist.
There are patients that during the cancer treatment don ’ t experience weight lost. Some of them were obese at the disease onset and can keep gaining weight. Obesity, especially abdominal, is a factor of risk in cervical, oesophageal, postmenopausal breast cancer, pancreatic, renal, colon and rectal cancer [3,41]. The abdominal obesity is associated with insulin resistance, increased insulin production, therefore increased cancer chance. Obesity is considered a factor of developing comorbidies or secondary cancers, and a weight loss diet could be appropriated. The ideal weight lost is maximum 1 kg per week, and special monitoring of body nutrient necessities meanwhile losing weight and following cancer treatment is required [3].
There is a concept in the medical practice and care that “sugar feeds cancer ” . By this we can understand that glucose is a mediator in the tumor metabolism by promoting cancer cell growth and division. The truth is that cancer cells normally use glucose with a higher rate than noncancerous cells, but this doesn ’ t mean that patients should take into consideration eliminating glucose or simple sugars (carbohydrates). This could even be a challenge for many patients, because carbohydrates provide the biggest proportion of the U.S. Recommended Daily Intake (RDI) from all macronutrients (carbohydrates, fats and proteins). When it comes to healthy individuals, the total daily caloric intake should be 20%-35% provided by fats, and approximately 50%-60% coming from carbohydrates. There is a contradiction between scientists when it comes to the appropriate RDI of proteins, although the current recommendation remains at 0.8 g/kg. The contradictions are focused on protein intake of healthy individuals, but little attention on the nutritional needs of the patient with cancer, no matter the age.
The plasma levels of all the essential amino acids (AAs, expecting tryptophan, and in some cases threonine) are lower than normal in patients with cancer [44-52], which shows inadequately nutritional intake. When it comes to the American Society for Parenteral and Enteral oncology patients, the recommendation is minimum daily protein supply of 1 g/kg body weight, and target supply of (1-1.2) g/kg. The argument for increased intake of protein and amino acid (AA) sources in cancer patients is simple: providing an anabolic stimulation on the skeletal muscles in moments when it is exposed to a higher rate of breakdown because of the cancer and tumor related factors [53].
When it comes to cancer and aging, the stimulation of the muscle protein synthesis can be achieved by adding amino acid (AA) such leucine, which is the principal nutrient responsible for the stimulation of muscle protein synthesis [54], to highprotein supplements [55-57], or well-adjusted meals with a lean protein source [58]. It is known that the difference exists in the time course of the anabolic response to nutritional support related to age, the ingestion of amino acid (AA) acutely [59-61] and chronically [62] stimulates muscle protein anabolism [63] in healthy older adults. By the use of isotopic methodologies and tracer of phenylalanine, one study showed that 40 g of mixed amino acids (AAs) given in small amounts to avoid gastrointestinal side effects stimulates muscle protein synthesis in a mix of younger and older patients with ovarian cancer [64].
Skeletal muscle anabolism in response to an amino acid (AA) supply in healthy elderly individuals can be solid, taking in count the degree of skeletal muscle anabolic resistance with aging [65-67] to amino acids (AAs), which can be valid in the case of elderly with cancer disease. The metabolic response in elderly with cancer is slower and affected compared to healthy elderly or younger cancer patients [64].
Conclusion
Implementing nutrition in cancer care is a major key to support the patient’s tolerance through all stages and types of therapy. Even though studies show inconclusive results or evidence when it comes to certain supplements formulas, higher attention is required on food intake.
A RDN must consult cancer patients after they have visited their oncologist and help them implement the proper diet for their cancer diagnosis and related diagnoses (e.g., diabetes, hypertension, gout, etc.).
Cancer treatment is the main factor that influences many of the changes in the patient ’ s diet. Having side effects due to a treatment can really make you have a hard time in choosing the right food and getting advice from a dietician is exactly what you need.
In order to understand and apply the nutritional indications correctly a personalized diet with all the meals of the day and the proper quantities should be delivered to the patient and explained.
If the patient can’t keep up with the diet for different reasons besides treatment’ s side effects or other oncological causes (e.g., dysphagia, odynophagia, total gastrectomy, etc.) and shows signs of depression he must be directed immediately to a psychologist for therapy. Being depressed can also make the patient neglect the meals and to back up not only when it comes to nutrition, but also dispense cancer treatment and lose touch with the medical team.
Therefore, a cancer patient needs to be treated by more than one specialist in order for him to follow the treatment with fewer complications than usually expected or seen in previous patients. Offering the patient ’ s multimodal supporting (treatment, nutrition, and psychology) can make him understand his diagnosis better and motivate him to continue the battle with cancer by creating better quality of life and emotional stability, all from his medical care team.
REFERENCES
- Siegel RL, Miller KD, Jemal A. Cancer statistics. CA Cancer J Clin. 2017;67:7-30.
- Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36:11-48.
- Leser M, Ledesma N, Bergerson S, Trujillo E. Oncology nutrition for clinical practice. Chicago, IL: Oncology nutrition dietetic practice group of the academy of nutrition and dietetics, 2013.
- Kushi LH, Doyle C, McCullough M, Rock CL, Wahnefried WD, Bandera EV, et al. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62:30-67.
- Feinberg J, Nielsen EE, Korang SK, Engell KH, Nielsen MS, Zhang K, et al. Nutrition support in hospitalised adults at nutritional risk. Cochrane Database Syst Rev. 2017.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology, Palliative Care, version 1. 2018;27:38-42.
- Suhag V, Sunita BS, Sarin A, Singh AK. Cancer, malnutrition and cachexia: we must break the triad. Int J Med Phys Clin Eng Radiat Oncol. 2015;4:64.
- Virizuela JA, Álvarez MC, Pérez LM, Grande E, Hernández JA, Madroño MJS, et al. Nutritional support and parenteral nutrition in cancer patients: an expert consensus report. Clin Transl Oncol. 2018;20:619-629.
- Nelm L, Sucher KP, Lacey K. Nutrition therapy and pathophysiology. 3rd ed. Boston. Cengage Learning. 2016.
- Aoyagi T, Terracina KP, Raza A, Matsubara H, Takabe K. Cancer cachexia, mechanism and treatment. World J Gastrointest Oncol. 2015;7:17-29.
- Alibhai SM, Greenwood C, Payette H. An approach to the management of unintentional weight loss in elderly people. Can Med Assoc J. 2005;172:773-780.
- Morley JE. Anorexia of aging: physiologic and pathologic. Am J Clin Nutr. 1997;66:760-773.
- Hoppe S, Rainfray M, Fonck M, Hoppenreys L, Blanc JF, Ceccaldi J, et al. Functional decline in older patients with cancer receiving first-line chemotherapy. J Clin Oncol. 2013;31:3877-3882.
- Soubeyran P, Fonck M, Bisson CB, Blanc JF, Ceccaldi J, Mertens C, et al. Predictors of early death risk in older patients treated with first-line chemotherapy for cancer. J Clin Oncol. 2012;30:1829-1834.
- Extermann M, Boler I, Reich RR, Lyman GH, Brown RH, DeFelice J, et al. Predicting the risk of chemotherapy toxicity in older patients: The Chemotherapy Risk Assessment Scale for High‐Age Patients (CRASH) score. Cancer. 2012;118:3377-3386.
- Lara KS, Turcott JG, Juárez E, Guevara P, Valencia CN, Ocaña LFO, et al. Association of nutrition parameters including bioelectrical impedance and systemic inflammatory response with quality of life and prognosis in patients with advanced non-small-cell lung cancer: a prospective study. Nutr Cancer. 2012;64:526-534.
- Prado CM, Baracos VE, McCargar LJ, Reiman T, Mourtzakis M, Tonkin K, et al. Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Clin Cancer Res. 2009;15:2920-2926.
- Antoun S, Baracos VE, Birdsell L, Escudier B, Sawyer MB. Low body mass index and sarcopenia associated with dose-limiting toxicity of sorafenib in patients with renal cell carcinoma. Ann Oncol. 2010;21:1594-1598.
- Wildiers H, Heeren P, Puts M, Topinkova E, Heijnen MLJ, Extermann M, et al. International Society of Geriatric Oncology consensus on geriatric assessment in older patients with cancer. J Clin Oncol. 2014;32:2595-2603.
- Rock CL, Doyle C, Wahnefried WD, Meyerhardt J, Courneya KS, Schwartz AL, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62:242-274.
- Ravasco P, Grillo IM, Vidal PM, Camilo ME. Dietary counseling improves patient outcomes: a prospective, randomized, controlled trial in colorectal cancer patients undergoing radiotherapy. J Clin Oncol. 2005;23:1431-1438.
- Paccagnella A, Morello M, Da Mosto MC, Baruffi C, Marcon ML, Gava A, et al. Early nutritional intervention improves treatment tolerance and outcomes in head and neck cancer patients undergoing concurrent chemoradiotherapy. Support Care Cancer. 2010;18:837-845.
- Van der Meij BS, Langius JA, Smit EF, Spreeuwenberg MD, von Blomberg BM, Heijboer AC, et al. Oral nutritional supplements containing (n-3) polyunsaturated fatty acids affect the nutritional status of patients with stage III non-small cell lung cancer during multimodality treatment. J Nutr. 2010;140:1774-1780.
- Hughes BG, Jain VK, Brown T, Spurgin AL, Hartnett G, Keller J, et al. Decreased hospital stay and significant cost savings after routine use of prophylactic gastrostomy for high‐risk patients with head and neck cancer receiving chemoradiotherapy at a tertiary cancer institution. Head neck. 2013;35:436-442.
- Nitenberg G, Raynard B. Nutritional support of the cancer patient: issues and dilemmas. Crit Rev Oncol Hematol. 2000;34:137-168.
- Deutz NE, Safar A, Schutzler S, Memelink R, Ferrando A, Spencer H, et al. Muscle protein synthesis in cancer patients can be stimulated with a specially formulated medical food. Clin Nutr. 2011;30:759-768.
- Enterria PG, Gonzalez LL. Preparation, methods and guidelines for the administration of home parenteral nutrition. Monitoring of patients. Education for patients and caregivers. Nutr Hosp Suplementos. 2009;2:18-24.
- Hernández JÁ, Carmona DM, Vila MP, Rodríguez IR, Rovira PS, Palmer MS. Consensus document. Hosp Nutr. 2008;1(1):13-48.
- Andersen D, Baird S, Bates T, Chapel DL, Cline AD, Ganesh SN, et al. Academy of nutrition and dietetics: Revised 2017 standards of practice in nutrition care and standards of professional performance for registered dietitian nutritionists. J Acad Nutr Diet. 2018;118:132-140.
- Thompson KL, Elliott L, Tarlovsky VF, Levin RM, Voss AC, Piemonte T. Oncology evidence-based nutrition practice guideline for adults. J Acad Nutr Diet. 2017;117:297-310.
- Mahan KL, Stump SE, Raymond J. Krause’s food and the nutrition care process. 13th ed. Elsevier Saunders. 2012.
- Dennett C. Nutrition-focused physical exams. Today’s Dietitian. 2016;18:36.
- Shah MK, Workeneh B, Taffet GE. Hypernatremia in the geriatric population. Clin Interv Aging. 2014;9:1987-1992.
- Ferraro CD, Grant M, Koczywas M, Dorr-Uyemura LA. Management of anorexia-cachexia in late stage lung cancer patients. J Hosp Palliat Nurs. 2012;14:1-12.
- Bressan V, Bagnasco A, Aleo G, Catania G, Zanini MP, Timmins F, et al. The life experience of nutrition impact symptoms during treatment for head and neck cancer patients: a systematic review and meta-synthesis. Support Care Cancer. 2017;25:1699-1712.
- White D, Guenter P, Jensen G, Malone A, Schofield M. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012;112:730-738.
- Marinho EDC, Custódio IDD, Ferreira IB, Crispim CA, Paiva CE, Maia YCP. Impact of chemotherapy on perceptions related to food intake in women with breast cancer: A prospective study. PLoS One. 2017;12:e0187573.
- American Cancer Society. Nutrition and physical activity and cancer prevention. 2017;5:47-55.
- Grosso G, Micek A, Godos J, Pajak A, Sciacca S, Galvano F, et al. Health risk factors associated with meat, fruit and vegetable consumption in cohort studies: A comprehensive meta-analysis. PLoS One. 2017;12:1-21.
- Freisling H, Arnold M, Soerjomataram I, O'Doherty MG, Mena JMO, Bamia C, et al. Comparison of general obesity and measures of body fat distribution in older adults in relation to cancer risk: meta-analysis of individual participant data of seven prospective cohorts in Europe. Br J Cancer. 2017;116:1486-1497.
- Lin PH, Aronson W, Freedland SJ. Nutrition, dietary interventions and prostate cancer: the latest evidence. BMC Med. 2015;13:3.
- Lin PH, Aronson W, Freedland SJ. An update of research evidence on nutrition and prostate cancer. Urol Oncol. 2019;37:387-401.
- Wittenaar HJ, Ottery FD. Assessing nutritional status in cancer: role of the patient-generated subjective global assessment. Curr Opin Clin Nutr Metab Care. 2017;20:322-329.
- Lee JC, Chen MJ, Chang CH, Tiai YF, Lin PW, Lai HS, et al. Plasma amino acid levels in patients with colorectal cancers and liver cirrhosis with hepatocellular carcinoma. Hepatogastroenterology. 2003;50:1269-1273.
- Norton JA, Gorschboth CM, Wesley RA, Burt ME, Brennan MF. Fasting plasma amino acid levels in cancer patients. Cancer. 1985;56:1181-1186.
- Ching N, Grossi C, Jham GU, Angers J, Zurawinsky H, Ching CY, et al. Plasma amino acid and serum unesterified fatty acid deficits and the effect of nutritional support in chemotherapy treatment. Surg. 1984;95:730-738.
- Watanabe A, Higashi T, Sakata T, Nagashima H. Serum amino acid levels in patients with hepatocellular carcinoma. Cancer. 1984;54:1875-1882.
- Naini AB, Dickerson JW, Brown MM. Preoperative and postoperative levels of plasma protein and amino acid in esophageal and lung cancer patients. Cancer. 1988;62:355-360.
- Yamanaka H, Kanemaki T, Tsuji M, Kise Y, Hatano T, Hioki K, et al. Branched-chain amino acid-supplemented nutritional support after gastrectomy for gastric cancer with special reference to plasma amino acid profiles. Nutr. 1990;6:241-245.
- Georgiannos SN, Weston PM, Goode AW. Correlation between albuminuria and positively charged amino acids in gastrointestinal cancer. Int Surg. 1995;80:49-52.
- Kubota A, Meguid MM, Hitch DC. Amino acid profiles correlate diagnostically with organ site in three kinds of malignant tumors. Cancer. 1992;69:2343-2348.
- Pearlstone DB, Lee JI, Alexander RH, Chang TH, Brennan MF, Burt M. Effect of enteral and parenteral nutrition on amino acid levels in cancer patients. J Parenter Enteral Nutr. 1995;19:204-208.
- August DA, Huhmann MB. American Society for Parenteral and Enteral Nutrition (ASPEN) Board of Directors. ASPEN clinical guidelines: nutrition support therapy during adult anticancer treatment and in hematopoietic cell transplantation. J Parenter Enteral Nutr. 2009;33:472-500.
- Wolfe RR. Regulation of muscle protein by amino acids. J Nutr. 2002;132:3219-3224.
- Katsanos CS, Kobayashi H, Moore MS, Aarsland A, Wolfe RR. A high proportion of leucine is required for optimal stimulation of the rate of muscle protein synthesis by essential amino acids in the elderly. Am J Physiol Endocrinol Metab. 2006;291:381-387.
- Koopman R, Verdijk L, Manders RJ, Gijsen AP, Gorselink M, Pijpers E, et al. Co-ingestion of protein and leucine stimulates muscle protein synthesis rates to the same extent in young and elderly lean men. Am J Clin Nutr. 2006;84:623-632.
- Rieu I, Balage M, Sornet C, Giraudet C, Pujos E, Grizard J, et al. Leucine supplementation improves muscle protein synthesis in elderly men independently of hyperaminoacidaemia. J Physiol. 2006;575:305-315.
- Symons TB, Moore MS, Wolfe RR, Jones DP. Moderating the portion size of a protein-rich meal improves anabolic efficiency in young and elderly. J Am Diet Assoc. 2009;109:1582-1586.
- Jones DP, Moore MS, Zhang XJ, Volpi E, Wolf SE, Aarsland A, et al. Amino acid ingestion improves muscle protein synthesis in the young and elderly. Am J Physiol Endocrinol Metab. 2004;286:321-328.
- Volpi E, Moore MS, Rasmussen BB, Wolfe RR. Basal muscle amino acid kinetics and protein synthesis in healthy young and older men. Jama. 2001;286:1206-1212.
- Katsanos CS, Kobayashi H, Moore MS, Aarsland A, Wolfe RR. Aging is associated with diminished accretion of muscle proteins after the ingestion of a small bolus of essential amino acids. Am J Clin Nutr. 2005;82:1065-1073.
- Dillon EL, Moore MS, Jones DP, Gilkison C, Sanford AP, Casperson SL, et al. Amino acid supplementation increases lean body mass, basal muscle protein synthesis, and insulin-like growth factor-I expression in older women. J Clin Endocrinol Metab. 2009;94:1630-1637.
- Volpi E, Kobayashi H, Moore MS, Mittendorfer B, Wolfe RR. Essential amino acids are primarily responsible for the amino acid stimulation of muscle protein anabolism in healthy elderly adults. Am J Clin Nutr. 2003;78:250-258.
- Dillon EL, Volpi E, Wolfe RR, Sinha S, Sanford AP, Arrastia CD, et al. Amino acid metabolism and inflammatory burden in ovarian cancer patients undergoing intense oncological therapy. Clin Nutr. 2007;26:736-743.
- Durham WJ, Casperson SL, Dillon EL, Keske MA, Jones DP, Sanford AP, et al. Age-related anabolic resistance after endurance-type exercise in healthy humans. FASEB J. 2010;24:4117-4127.
- Guillet C, Prod’homme M, Balage M, Gachon P, Giraudet C, Morin L, et al. Impaired anabolic response of muscle protein synthesis is associated with S6K1 dysregulation in elderly humans. FASEB J. 2004;18:1586-1587.
- Volpi E, Mittendorfer B, Rasmussen BB, Wolfe RR. The response of muscle protein anabolism to combined hyperaminoacidemia and glucose-induced hyperinsulinemia is impaired in the elderly. J Clin Endocrinol Metab. 2000;85:4481-4490.
Citation: Roxana C (2020) Implementing Nutrition in Cancer Care. J Food Process Technol 11:830. doi: 10.35248/2157-7110.20.11.830
Copyright: © 2020 Roxana C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.