Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
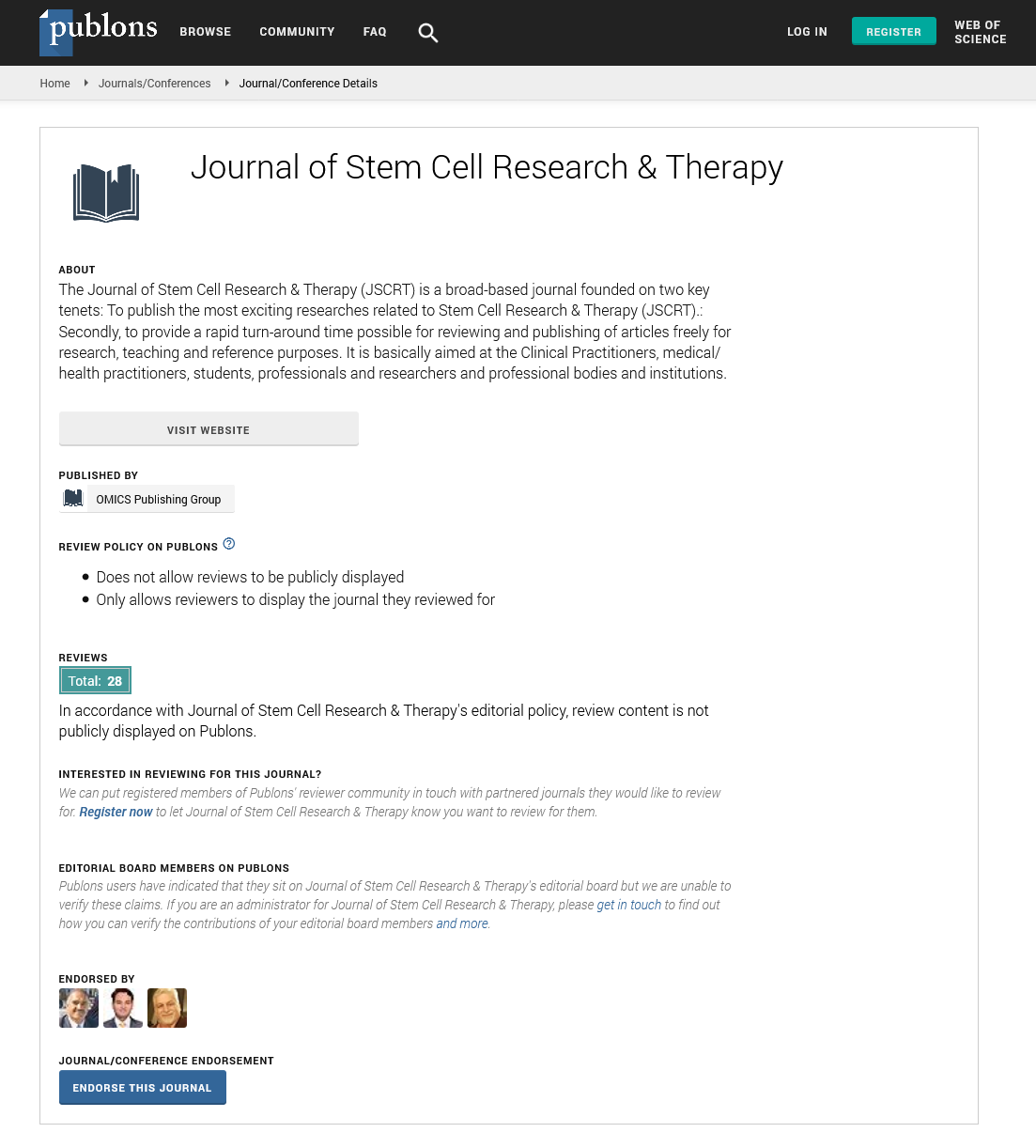
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2022) Volume 12, Issue 5
Impact of Stem Cell Based Therapies for Brain Stroke
Jimin Hoo*Received: 29-Apr-2022, Manuscript No. JSCRT-22-16822; Editor assigned: 03-May-2022, Pre QC No. JSCRT-22-16822(PQ); Reviewed: 17-May-2022, QC No. JSCRT-22-16822; Revised: 26-May-2022, Manuscript No. JSCRT-22-16822(R); Published: 02-Jun-2022, DOI: 10.35248/2157-7633.22.12.533
Description
To restore brain integrity, stem cell therapies for stroke aim to repair, replace, and enhance the biological activity of injured or dead cells. Differentiated neural progenitor cells, for example, can restore the circuitry of functioning neurons, and the paracrine substances they release can help endogenous penumbral progenitor cells survive, differentiate, and migrate.
MSCs include UCB Mononuclear Cells (MNCs), Human Umbilical Cord Mesenchymal Stem Cells (HUCMSCs), Bone Marrow Stem Cells (BMSCs), and Adipose Tissue Derived Stem Cells (ADSCs), whereas endogenous stem cells include peripheral blood CD34 cells, GCSF-induced CD34 cells, and Neural Stem Cells (NSCs). Each form of stem cell has a unique influence on stroke recovery; nonetheless, MSCs are the most often used cell type for stroke therapy at the moment. We'll go through the many types of stem cells employed in preclinical research in this section.
Umbilical cord blood mononuclear cells
In vitro and in vivo, human UCB contains a large number of hematopoietic and endothelial primitive cells with high replication capabilities. Furthermore, the high amounts of EGF, VEGF, G-CSF, and IL-10 in UCB imply that it could help patients with cerebral stroke regain immunological homeostasis while also enhancing the healing of injured neurons. In addition to their regenerative properties, UCB MNCs exhibit immunomodulatory and anti-inflammatory properties, this may protect penumbral tissue from additional harm induced by inflammation after a stroke.
Human umbilical cord matrix MSCs
Human Umbilical Cord (HUC) is a new source of MSCs (HUCMSCs), which have rapid renewal properties and may be collected without pain. HUCMSCs are produced from the cord lining, Wharton's jelly, and perivascular tissue, and can be separated into three germ layers that promote tissue repair. By upregulating 1-integrin, HUCMSCs can improve both functional angiogenesis and neuroplasticity in animal models of stroke.
Hematopoietic factor and endogenous stem cell mobilization
GCSF is a cytokine that belongs to the growth factor family. GCSF has the ability to move hematopoietic stem cells from the bone marrow into the bloodstream. GCSF was once commonly utilised to treat neutropenia and re-establish bone marrow; however, bone marrow has lately substituted hematopoietic stem cells in transplantation to regenerate non-hematopoietic tissues in diseases such as Myocardial Infarction (MI). By boosting angiogenesis and neurogenesis, GCSF reduced the infarction area and improved the recovery of stroke rats. As a result, GCSF could be used to treat acute and chronic strokes.
MSCs and peripheral hematopoietic stem cells (CD34+)
Because of GCSF's efficacy, the possibility of Peripheral Hematopoietic Stem Cells (PBSCs) for treating acute and chronic cerebral ischemia was investigated, while clinical usage of embryonic stem cells is hampered by ethical concerns. PBSCs are a source of hematopoietic stem cells in stem cell therapy for stroke and are increasingly being used for transplantation. GCSF has been shown to mobilise and enhance the amount of PBSCs in bone marrow. Intracerebral PBSC transplantation has been found to significantly enhance neurological function in rats with chronic cerebral ischemia. To facilitate angiogenesis in the wounded brain area, healing mechanisms include macrophage/ microglial cells produced from stem cells and the production of 1 integrin.
Neural stem cells
NSCs have also been shown to have an effect in animal models of stroke, according to growing data. The implantation of intraparenchymal NSCs around the infarct region, for example, was found to improve sensorimotor dysfunction and motor disability, while further analysis of the infarct area suggested that lesion topology plays a key role in functional recovery after NSC transplantation, especially for striatal strokes.
Conclusion
Stroke is the primary cause of adult neurological disability worldwide, resulting in sensory-motor function impairment and neuronal death; nevertheless, there are no medicinal or surgical treatments available to enhance neurological function and neurogenesis in chronic stroke patients. GCSF, mesenchymal stem cells, autologous CD34+ peripheral blood stem cells, umbilical cord blood and stromal stem cells, and autologous adipose derived mesenchymal stem cells are among the hematopoietic growth factors and stem cell transplantation therapies for stroke that have gained increasing translational and clinical evidence.
Citation: Hoo J (2022) Impact of Stem Cell Based Therapies for Brain Stroke. J Stem Cell Res Ther. 12:533.
Copyright: © 2022 Hoo J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.