Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
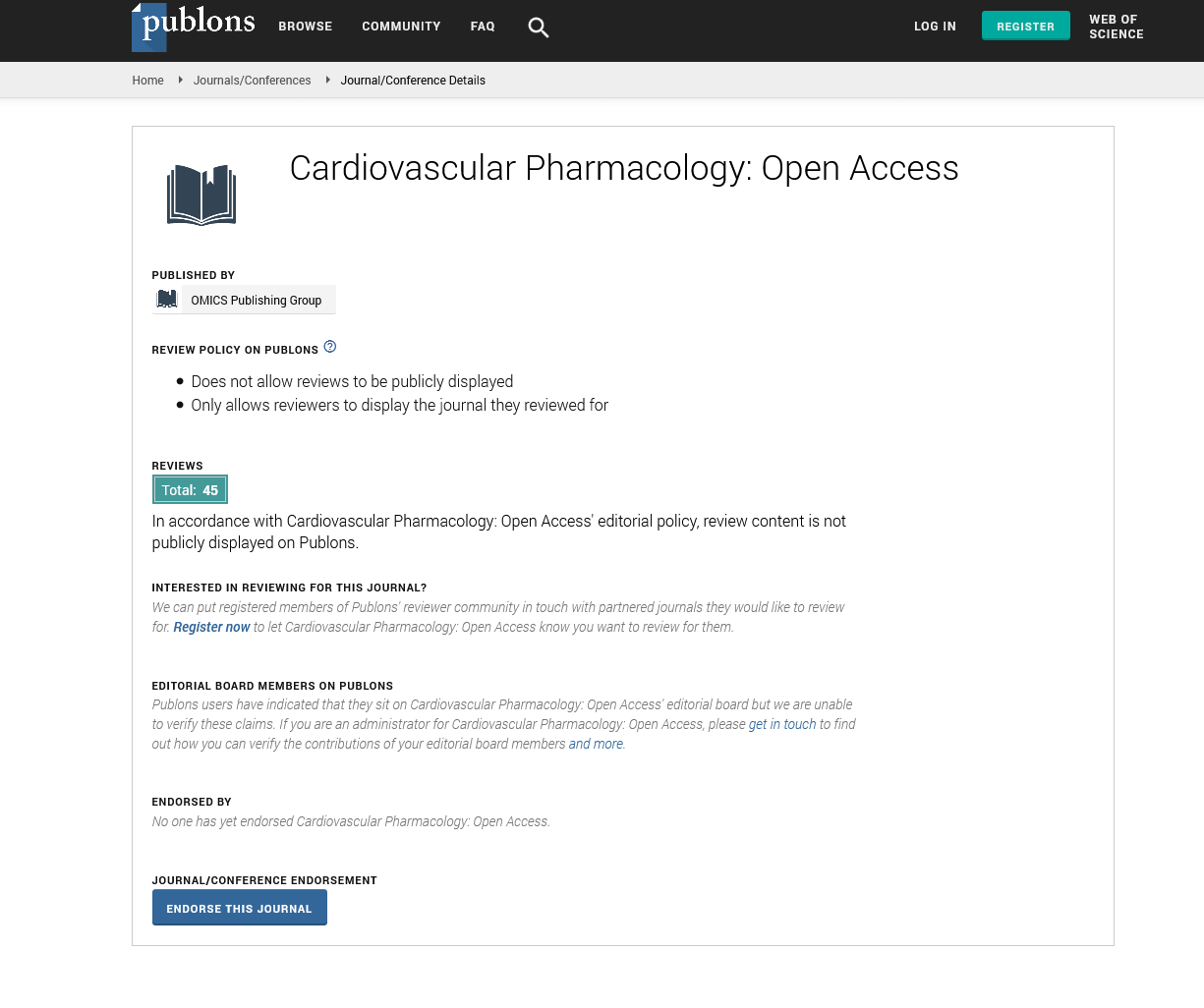
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
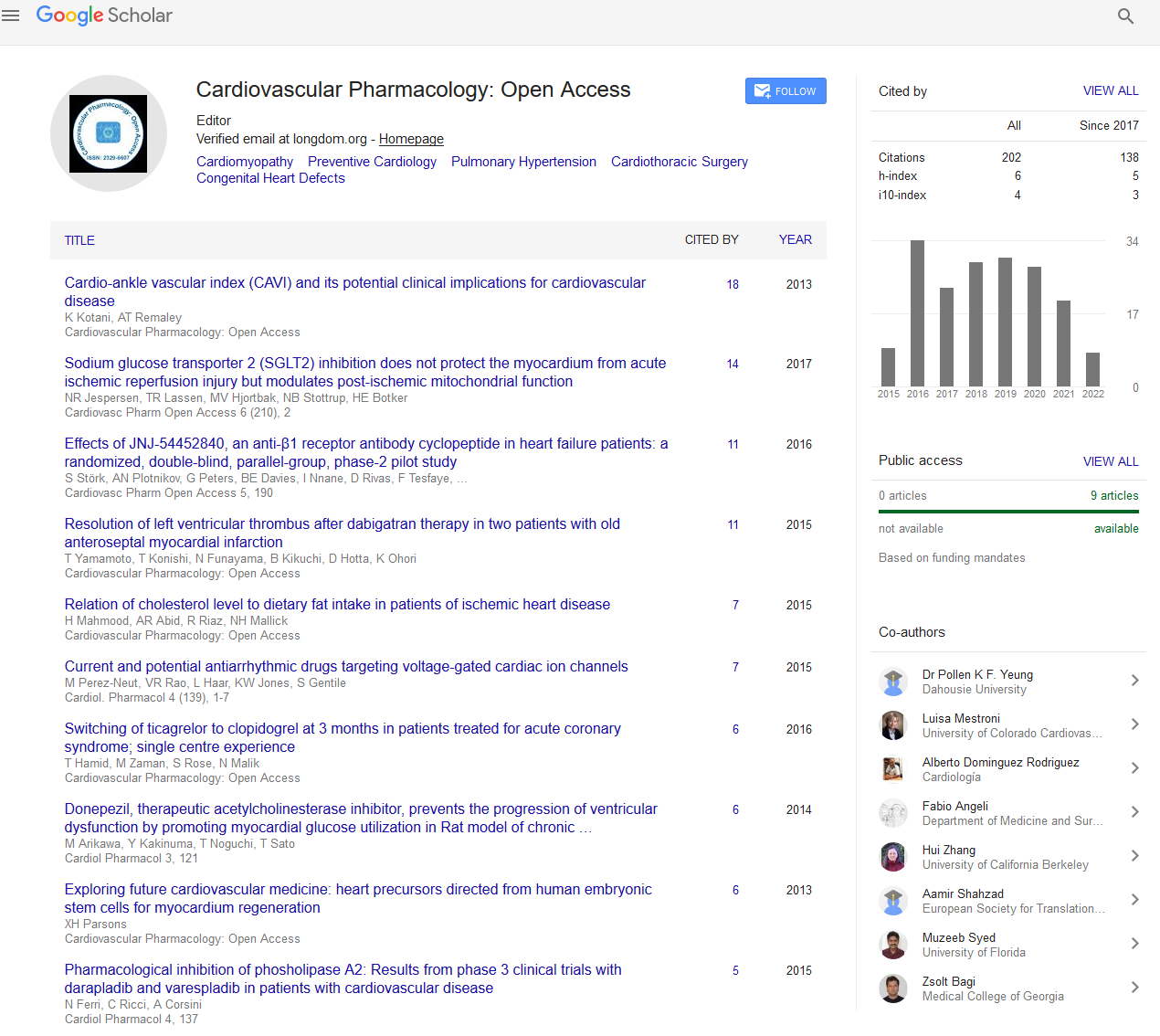
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion - (2024) Volume 13, Issue 1
Impact of Pharmacogenomics on Personalized Medicine in Cardiovascular Pharmacotherapy
Chen Jain*Received: 04-Mar-2024, Manuscript No. CPO-24-25977 ; Editor assigned: 06-Mar-2024, Pre QC No. CPO-24-25977 (PQ); Reviewed: 20-Mar-2024, QC No. CPO-24-25977 ; Revised: 27-Mar-2024, Manuscript No. CPO-24-25977 (R); Published: 03-Apr-2024, DOI: 10.35248/2329-6607.24.13.386
Description
Pharmacogenomics, the knowledge of how an individual's genetic personality affects their response to drugs, has revolutionized the field of personalized medicine, particularly in cardiovascular pharmacotherapy. This revolutionary castigation embraces the capacity of adapting medication regimens to individual patients based on their genetic contour, ultimately maximizing efficacy while minimizing opposing effects. The impacts of pharmacogenomics on modified medicine in cardiovascular pharmacotherapy are multifaceted, spanning from drug development and clinical decision-making to patient effects and healthcare economics. One of the most significant impacts of pharmacogenomics on personalized medicine in cardiovascular pharmacotherapy mendacities in drug development. By elucidating genetic variations that influence drug metabolism, efficacy, and toxicity, pharmacogenomics enables pharmaceutical companies to develop drugs targeted at specific patient populations. This targeted methodology not only increases the probability of therapeutic success but also reduces the risk of adverse reactions, thus reorganization the drug development process and improving overall patient safety. Furthermore, pharmacogenomics plays a central role in clinical decision-making by providing clinicians with valuable perceptions into individual patients' responses to medications. By analysing a patient's genetic contour, clinicians can identify genetic variants that may impact drug metabolism or efficacy, allowing them to modify treatment plans accordingly.
For example, in the case of anticoagulant therapy for cardiovascular disease, genetic testing can reveal variations in genes such as CYP2C9 and VKORC1, which influence the metabolism and response to drugs like warfarin. Armed with this information, clinicians can adjust drug dosages to achieve optimal therapeutic outcomes while minimizing the risk of bleeding or thrombotic actions. Moreover, pharmacogenomics empowers patients to take a proactive role in their healthcare by providing them with personalized treatment options based on their genetic predispositions.
By thoughtful how their genetic personality influences their response to medications, patients can make informed decisions in collaboration with their healthcare providers, leading to more effective and safer treatment outcomes. This personalized approach fosters a sense of enabling and commitment among patients, ultimately enhancing medication adherence and overall health outcomes. In addition to improving individual patient care, pharmacogenomics has broader implications for healthcare systems and economics. By optimizing medication regimens and minimizing adverse happenings, pharmacogenomics has the potential to reduce healthcare costs associated with medicationrelated complications, hospitalizations, and ineffective treatments. Moreover, by modifying treatments to individual patients, pharmacogenomics can help mitigate the societal burden of cardiovascular disease by improving outcomes and reducing the overall prevalence of the condition However, despite its immense potential, the widespread implementation of pharmacogenomics in personalized medicine still faces several challenges. One significant challenge is the integration of pharmacogenomics data into clinical practice in a manner that is both practical and cost-effective.
While advances in technology have made genetic testing more accessible and affordable, there are still barriers to widespread adoption, including the need for standardized testing protocols, clinician education, and reimbursement policies. Furthermore, there are moral and collective considerations surrounding the use of pharmacogenomics data, including issues related to patient privacy, consent, and equity in access to testing and treatment. Ensuring equitable access to pharmacogenomics testing and personalized treatments is essential to preventing advance differences in healthcare outcomes based on socioeconomic position or physical situation.
Citation: Jain C (2024) Impact of Pharmacogenomics on Personalized Medicine in Cardiovascular Pharmacotherapy. Cardiovasc Pharm. 13:386.
Copyright: © 2024 Jain C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.