Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
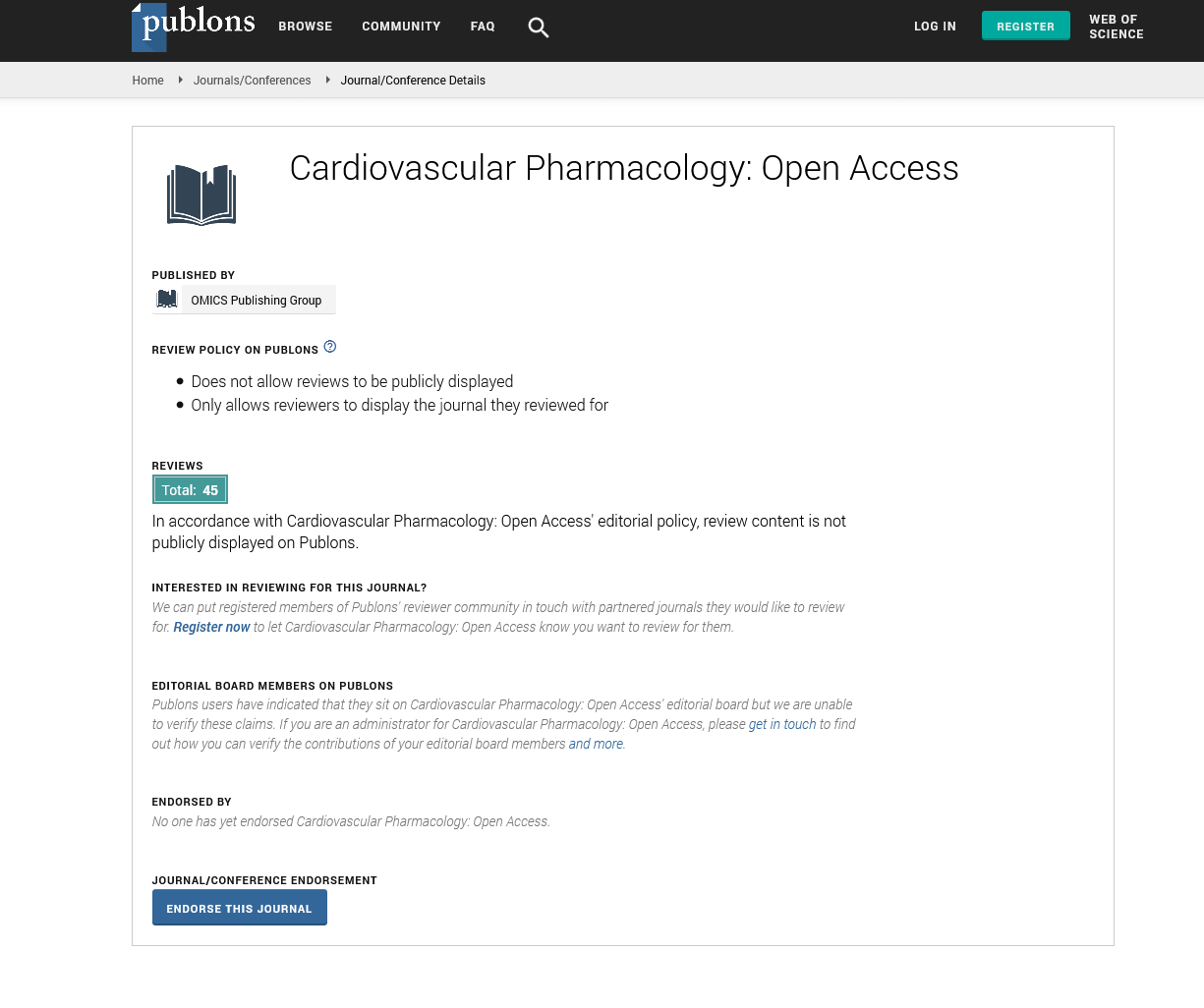
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
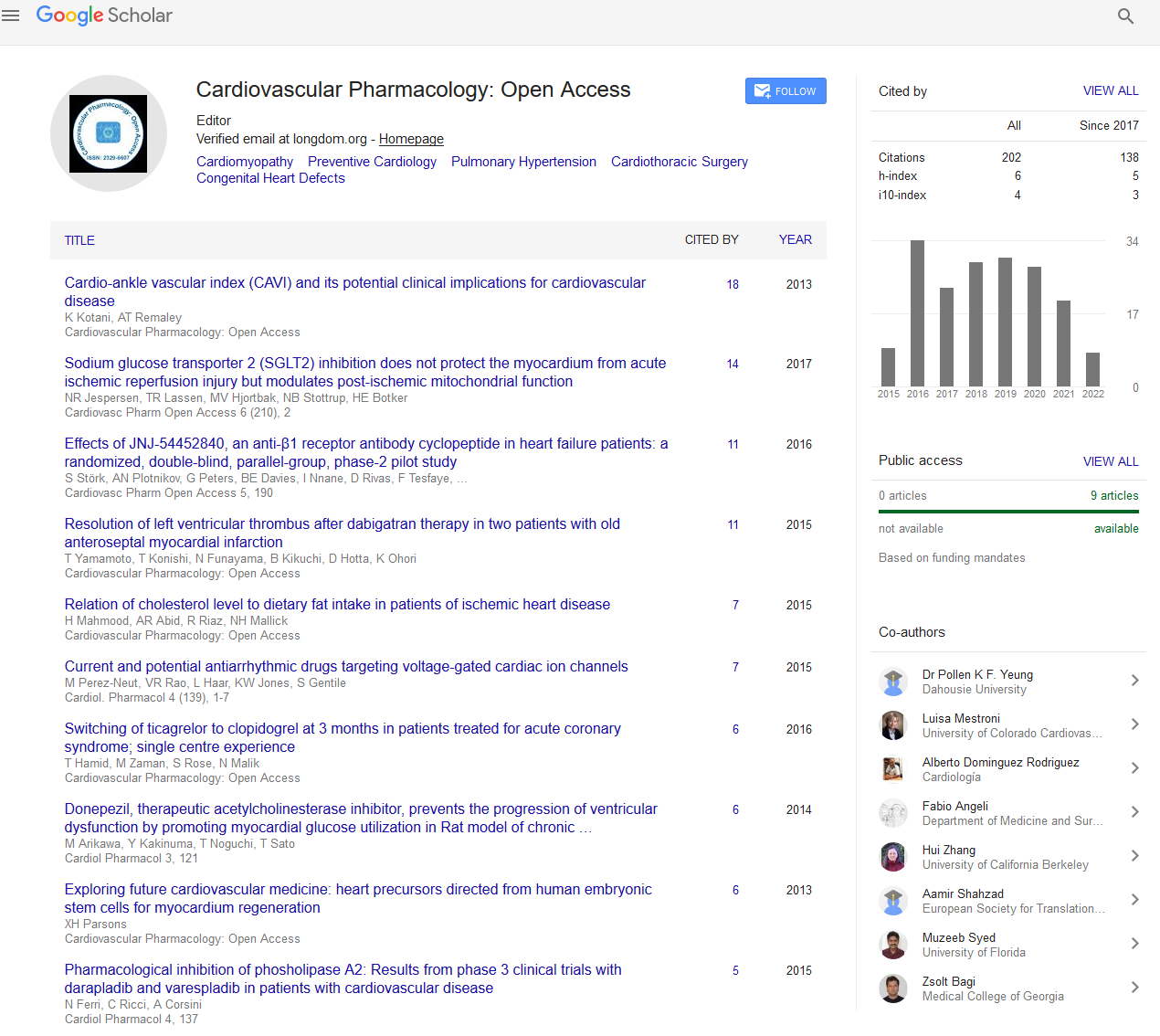
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2024) Volume 13, Issue 3
Immunological Aspects Involved in Brugada Syndrome
Liam Anderson*Received: 30-Aug-2024, Manuscript No. CPO-24-27834; Editor assigned: 02-Sep-2024, Pre QC No. CPO-24-27834 (PQ); Reviewed: 16-Sep-2024, QC No. CPO-24-27834; Revised: 23-Sep-2024, Manuscript No. CPO-24-27834 (R); Published: 30-Sep-2024, DOI: 10.35248/2329-6607.24.13.403
Description
Brugada Syndrome (BRS) is an inherited cardiac arrhythmia characterized by a distinctive Electrocardiographic (ECG) pattern and an increased risk of sudden cardiac death. First described in 1992 by the Brugada brothers, Pedro and Josep Brugada, the syndrome has received considerable attention due to its unique clinical presentation and potential immunological implications. Understanding the immunological aspects of Brugada syndrome may provide insight into the underlying pathophysiology and potential therapeutic approaches [1]. This article explains the historical background of Brugada syndrome, highlights the contributions of fundamental figures in the study of the syndrome and discusses the positive and negative aspects of the immunological links associated with the condition.
Historically, Brugada syndrome was identified when the Brugada brothers observed a group of patients with syncope (temporary loss of consciousness) and sudden cardiac death at night, accompanied by characteristic changes in their ECGs, particularly ST-segment elevation [2,3]. This discovery was significant because it established Brugada syndrome as a clinical entity distinct from other manifestations of arrhythmogenic disorders. Understanding the genetic basis of Brugada syndrome has since become a focus, emphasizing the abnormal function of ion channels, particularly the sodium channels encoded by the SCN5A gene [4]. This genetic aspect, although largely electrical in nature, has opened the way to explore the potential interplay between genetics, immunity and inflammation.
Immunological research into Brugada syndrome has emerged more recently, with studies suggesting that inflammation may influence the manifestation of the syndrome. It is hypothesized that systemic inflammation may influence the expression or function of myocardial ion channels, thereby facilitating the passage of arrhythmogenic substrates. Advantages of recognizing these immunological connections include potential new methods for treatment and risk stratification. Immunomodulatory therapies may be explored to modify inflammation in individuals susceptible to Brugada syndrome.
For example, Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) or corticosteroids may reduce inflammation and potentially reduce the incidence of arrhythmic events. Additionally, biomarkers identified from immunological studies may guide clinicians in assessing the risk of sudden cardiac death in patients with Brugada syndrome, thereby contributing to more proactive and personalized patient care [5,6].
However, despite the potential methods for surrounding the immunological aspects of Brugada syndrome, a number of challenges and limitations must be acknowledged. The relationship between inflammation and cardiac electrical activity is complex and current knowledge does not allow for a clear cause-and-effect relationship. Several studies have yielded conflicting results regarding the importance of inflammatory markers in Brugada syndrome, creating uncertainty among clinicians regarding the role of targeted immunotherapy [7]. Aspects such as individual genetic variability and the heterogeneity of the syndrome further complicate management and prognostic strategies.
Furthermore, there is a risk of oversimplifying the complex nature of Brugada syndrome. Brugada syndrome does not occur in isolation. It may present in association with other cardiovascular and systemic diseases in which inflammatory processes play a major role [8]. This interdependence may lead to misinterpretation of results unless careful comparative studies are performed. It raises concerns about the potential clinical implications if treatment is directed against inflammation without a full understanding of its interactions with genetic and environmental factors [9,10].
In conclusion, the emergence of immunological research on Brugada syndrome holds the potential to clarify its pathophysiology and to illuminate treatment options. Historical developments have laid the foundation for understanding the genetic and epigenetic aspects of the syndrome, while recent findings suggest that inflammation may play a central role in its clinical manifestation. While the positive implications of this knowledge are remarkable, they also come with challenges that require careful interpretation and further study.
As research continues to explore deeper into the immunological basis of Brugada syndrome, it is essential that clinicians and researchers remain alert to the complexity of the disease mechanism. Collaborative interdisciplinary efforts will be necessary to elucidate the complex genetic, immunological and cardiovascular networks underlying Brugada syndrome, with the ultimate goal of improving patient outcomes and reducing the rate of sudden cardiac death.
References
- Escárcega RO, Jiménez-Hernández M, Garcia-Carrasco M, Perez-Alva JC, Brugada J. The Brugada syndrome. Acta Cardiol. 2009;64(6):795-801.
[Crossref] [Google Scholar] [PubMed]
- Gaw AC, Lee B, Gervacio-Domingo G, Antzelevitch C, Divinagracia R, Jocano F Jr. Unraveling the enigma of Bangungut: Is Sudden Unexplained Nocturnal Death Syndrome (SUNDS) in the Philippines a disease allelic to the Brugada syndrome? Philipp J Intern Med. 2011;49(3):165-176.
[Google Scholar] [PubMed]
- Vohra J. Diagnosis and management of Brugada syndrome. Heart Lung Circ. 2011;20(12):751-6.
[Crossref] [Google Scholar] [PubMed]
- Matsusue A, Kashiwagi M, Hara K, Waters B, Sugimura T, Kubo S. An autopsy case of sudden unexpected nocturnal death syndrome with R1193Q polymorphism in the SCN5A gene. Leg Med (Tokyo). 2012;14(6):317-9.
[Crossref] [Google Scholar] [PubMed]
- Hermida JS, Six I, Jarry G. Drug-induced pericarditis mimicking Brugada syndrome. Europace. 2007;9(1):66-8.
[Crossref] [Google Scholar] [PubMed]
- Dendramis G, Paleologo C, Piraino D, Assennato P. Coronary artery fistulas and Brugada ECG pattern, a random association? Int J Cardiol. 2015 Oct 15:197:78-80.
[Crossref] [Google Scholar] [PubMed]
- Kuroki K, Yamamoto M, Sato A. Successful treatment of life-threatening giant cell myocarditis in a patient with Brugada syndrome, controlled through dual ablation procedures and immunosuppressive therapy. Eur Heart J Cardiovasc Imaging. 2024;25(2):e97.
- Wilcken DE. Overview of inherited metabolic disorders causing cardiovascular disease. J Inherit Metab Dis. 2003;26(2-3):245-57.
[Crossref] [Google Scholar] [PubMed]
- Moras E, Gandhi K, Narasimhan B, Brugada R, Brugada J, Brugada P, et al. Genetic and molecular mechanisms in Brugada syndrome. Cells. 2023;12(13):1791.
[Crossref] [Google Scholar] [PubMed]
- Spartalis M, Athanasiou A, Spartalis E, Voudris V. The development of Brugada syndrome phenotype is multifactorial, combining genetic and environmental factors. Eur Rev Med Pharmacol Sci. 2020;24(7):3444-3445.
[Crossref] [Google Scholar] [PubMed]
Citation: Anderson L (2024). Immunological Aspects Involved in Brugada Syndrome. Cardiovasc Pharm. 13:403.
Copyright: © 2024 Anderson L. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.