Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
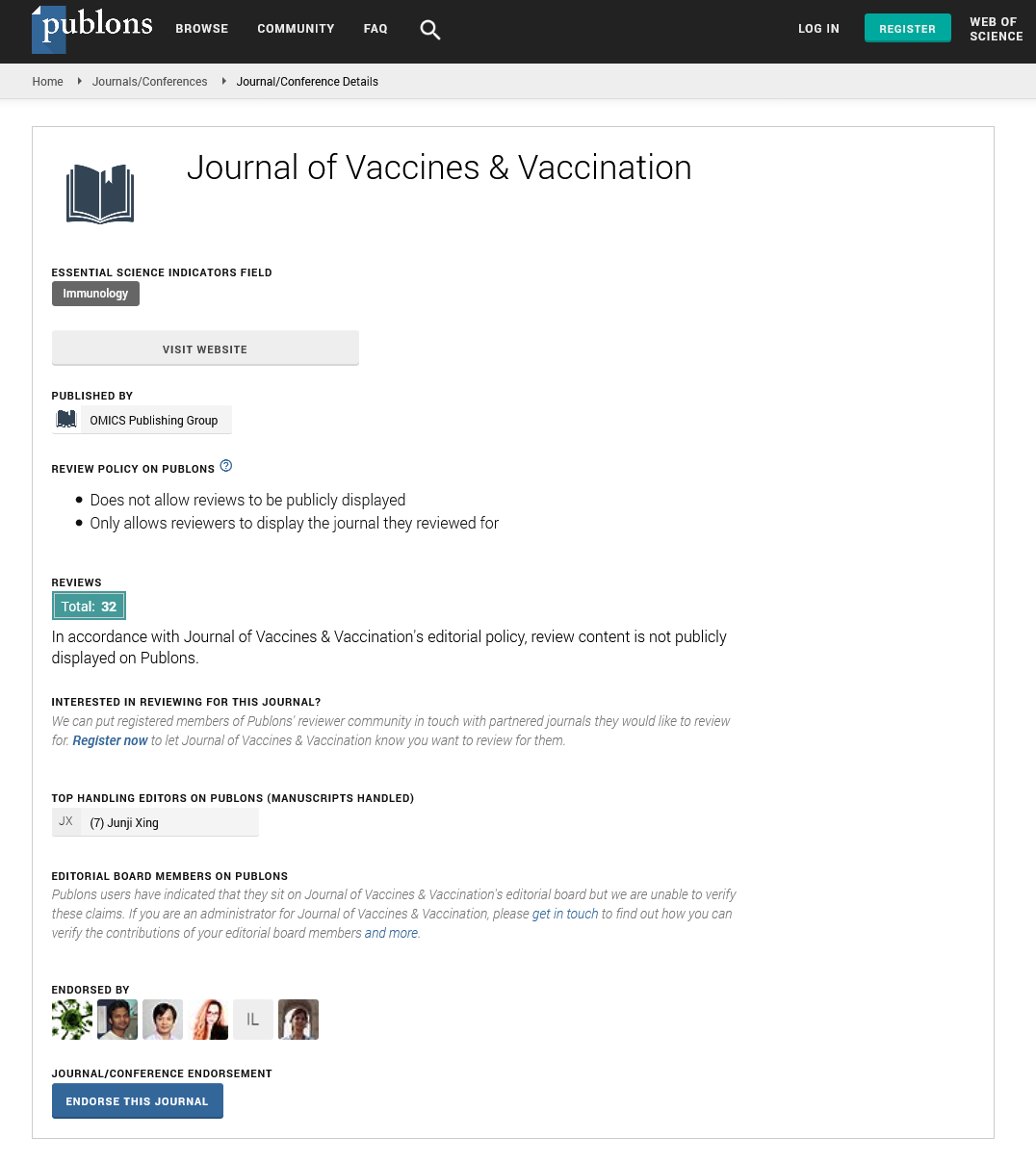
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2019) Volume 10, Issue 1
Human Papilloma Virus Vaccine Access and Use?The First Three Years After Introduction
Mungrue K*, Abraham R, Ahow K and Elder RReceived: 15-Sep-2018 Published: 25-Jan-2019
Abstract
Objective: The aim of this study is to measure the proportion of children aged 9-26 years who have received at least one HPV and the required three vaccination in Trinidad and parental awareness and attitude towards the HPVvaccine.
Design and methods: We used a cross-sectional prospective study design. The population consisted of all parents 18 years and over with at least one live birth attending a paediatric out-patient clinic at three teaching hospitals associated with the University of the West Indies. A de novo questionnaire was designed and administered to all participants.
Results: We report three key findings: 1) parents with children eligible for the HPV vaccine overall knowledge of HPV as well as the vaccine was low, 2) very few parents understood the types and nature of the vaccine and 3) there was a law uptake particularly in the school-based program.
Conclusion: We provide evidence on parental barriers to the HPV vaccination program introduced in 2013 as well as the current uptake of the vaccine.
Introduction
Cervical cancer is the third most commonly diagnosed cancer and the fourth leading cause of cancer death in women worldwide [1]. Latin America and the Caribbean have one of the highest incidence and mortality rates from cervical cancer in the world [2], age-adjusted incidence rates range from 20 to 80 per 100 000 women per year. Trinidad reported one of the highest rates of mortality from cervical cancer with an age-standardized mortality rate for cervical cancer of 10 per 100 000 population for the period 2000-2008 [3]. The most important risk factor for development of cervical cancer is persistent infection by a high-risk subset of human papilloma virus (HPV) [4]. HPV is associated with approximately 99.7% of cervical cancers, 60% of oropharyngeal cancers, 91% of anal cancers, 75% of vaginal cancers, 69% of vulvar cancers, and 63% of penile cancers [5-7]. The human papilloma virus vaccine (HPVc) is the first and only vaccination that helps protect women and men from getting these different types of cancer that are associated with different HPV strains. The vaccine was licensed in 2006, as a primary prevention strategy with the hope of reducing morbidity and mortality primarily from cervical cancer. Three prophylactic HPV vaccines are available as bivalent, quadrivalent, and nanovalent (9-valent) vaccines. The bivalent vaccine protects against HPV -16 and -18, the most common oncogenic HPV types, which are responsible for approximately 70% of HPV-associated cervical cancers and a large proportion of other HPV related cancers [8]. The quadrivalent vaccine in addition to protecting against HPV -16 and -18 also protects against HPV -6 and -11, two non-oncogenic HPV types that cause genital warts and respiratory papillomatosis [9]. The 9-valent vaccine protects against HPV -6, -11, -16, and -18 and against 5 other oncogenic types: HPV -31, -33, -45, -52, and -58 [10].
Routine HPV vaccination is recommended for both females and males aged 11-12 years. HPV vaccination can be started by the age of 9 years or can be given between the ages of 13-26 years for females and 13-21 years for males who did not receive the HPV vaccine previously. For males who have sex with males or those who are immunocompromised, it can be given through age 26 years. Any of the vaccines may be given to females while only the quadrivalent or 9- valent vaccines are recommended for males [11].
In Trinidad, routine HPV vaccination of girls began in 2013 using “Gardasil” (HPV 6,11,16,18, 20/40/40/40 mcg, with amorphous aluminium hydroxyl phosphate sulphate adjuvant), for routine vaccination in girls of 9 to 26 years. Because of the slow natural history of HPV oncogenesis, the effect of vaccination on invasive cancers will not be evident for decades. Pre-invasive cervical intraepithelial neoplasia 2 and 3 and adenocarcinoma in situ (together referred to as CIN2+), which are detected through routine screening, take less time to develop and are used as a surrogate for cervical cancer in vaccine trials. Real-world reductions in CIN2+ have been shown in countries with high vaccination coverage and catch-up programs for older persons and where it is possible to link data across population-based disease, screening, and vaccination registries [12].
The CDC and NIH report continuously low uptake of the HPV vaccine with vaccination of males being significantly lower than females. Current estimates indicate that four out of ten adolescent girls and six out of ten adolescent boys have not started the HPV vaccine series. Despite a slight overall increase (3%) in both 2013 and 2014, uptake of the HPV vaccine has fallen in the past few years from its initial uptake after it was approved [13-16]. Additionally, studies done worldwide regarding knowledge and attitudes to the HPV vaccine generally show trends of low knowledge about HPV, the HPV vaccine and associated cancers. There are also many concerns about the vaccine, with the most significant barriers consisting of vaccine efficacy, safety and side effects [17-20].
Although widespread vaccination could greatly reduce the incidence of cervical cancer and other conditions associated with HPV this will only be achieved with significant increases of HPV vaccination both nationally and globally. The extent of this need is reflected in the collaborative effort of various nations in support of GAVI to facilitate introduction of the HPV vaccine in low income countries. Several studies have reported declines in cervical and vulvovaginal infection with incidence of HPV related disease declining following HPV vaccination, and HPV prevalence decreasing by 56% from the pre vaccine era. A substantially lowered risk of developing genital warts was also observed with reduction in persistent external genital and anal HPV infection and lesions including condyloma and squamous intraepithelial lesions [21]. The main efficacy study of the bivalent vaccine reported 93% prevention of cervical pre-cancers due to HPV, while the quadrivalent trial showed nearly 100% vaccine efficacy in preventing cervical and vulvovaginal pre-cancers and genital warts in women, and 90% in preventing genital warts and 75% in preventing anal precancers in men [22].
In Trinidad, a decline in population-level CIN2+ attributable to vaccination is difficult to measure because of lack of national screening registries and because CIN2+ diagnosis is affected by changes in screening recommendations. It is important therefore, in the first instance, to determine the current rate of HPV vaccine uptake, as well as, the perception of mothers to the vaccine. Currently females are the focus of HPV vaccination in Trinidad, however it is necessary to consider the importance of male vaccination as well. This would not only assist in prevention of HPV-related diseases such as genital warts, anal cancer, and penile cancer in males, but may also have the benefit of decreased transmission of HPV infection to females. Monitoring of human papillomavirus (HPV) vaccination coverage is fundamental to assess the performance of vaccination programs and the potential impact of HPV vaccines on HPV-related diseases.
Thus we aimed to quantify the cumulative coverage of the publicly funded HPV immunization program in Trinidad, which started in 2013, as well as determining current parental awareness and attitude towards the HPV vaccine.
Methods
This study consisted of two parts, 1) a survey of parental attitudes and 2) an evaluation of the actual number of children and adults who received the vaccine between 2013-2015, in a defined geographical area. In the first part of the study all parents 18 years and over with at least one live birth attending a paediatric outpatient clinic at three teaching hospitals associated with the University of the West Indies (UWI), i.e. Eric Williams Medical Sciences Complex (EWMSC), the San Fernando General Hospital (SFGH), and the Sangre Grande General Hospital (SGGH) represented the population for the study. Proportionate stratification was used to select participants from each site, calculated as 37% from the EWMSC and the SFGH as these are two large hospitals serving large populations and 26% from the SGGH serving a smaller population. Consecutive sampling was used at each site to select participants. An estimated sample size of 240 was calculated. Participants were then selected first by randomly selecting paediatric outpatient clinic sessions at each of the three centers. Participants while waiting to visit the paediatrician at these sessions were invited to participate in the study. All eligible participants who agreed to participate were informed of the nature and purpose of the study and after verbal consent was obtained was administered a structured questionnaire. The 10-item survey assessed knowledge and attitudes to the HPV vaccine and knowledge about the HPV. Questions regarding attitudes about vaccines, and HPV, were based on psychological constructs from two validated models of health protective behavior: the Health Belief Model (HBM) and the Theory of Reasoned Action. The HBM offers, a useful framework for understanding vaccine acceptance, according to which the uptake of a health intervention is associated with perceived susceptibility to and severity of the relevant disease and the intervention's safety and efficacy. Empirical studies have validated this model as a predictor of vaccine refusal. Participants <18 years of age or with diminished mental capacity were excluded from the study. In the second part of the study we selected a dense population area consisting of 20 primary schools with an estimated population of 4000 children >9 years. We measured the proportion of children who received HPV vaccination. We also measured the number of adults who received at least one dose of the vaccine. The data were stored and analyzed using the SPSS vs. 21. Data analysis consisted of descriptive statistics including frequencies and mean scores. The significance level was set at p <0.05. Ethical approval was obtained from the Ethics Committee of the UWI.
Results
Using proportional stratification 99 participants were selected from the EWMSC, 91 from the SFGH and 54 from the SGGH. A total of 244 participants entered the study 134 (54.9%) mothers and 110 (45.1%) fathers. The mean age of participants was 26 years (SD ± 14.58), with 20.0% of the participants adolescents aged<20 years. Other characteristics of the sample included 36% (88) of participants had a child between the age 9-26 years and therefore eligible for vaccination and 20 (8.2%) had a university level education. There was a significant difference between parents who had knowledge of the vaccine 98(40.2%) than those who did not 146 (59.8%), p<0.05 (Table 1). A significantly higher proportion of parents 175 (72%, p=0.001) had no knowledge of the virus, as well as recognizing that this was a sexually transmitted infection (STI). The level of education attained had only a marginal influence on knowledge of the HPV, however there was a very small number of participants with tertiary level education. Very few participants (17, 7%) had knowledge of vaccine types particular the currently used quadravalant vaccine as opposed to 9-valent vaccine, which contains HPV types 45, 52 and 58 which may be more appropriate in the Caribbean. Notwithstanding more parents 152 (62.3%) expressed willingness to have their children vaccinated.
| Yes n (%) | No n (%) | |
|---|---|---|
| Knowledge of HPV vaccine | 98 (40.2) | 146 (59.8) |
| Knowledge of HPV virus | 69 (28.3) | 175 (71.7) |
| Vaccine Types | 17 (7) | 227 (93) |
| Side effects | 22 (9) | 222 (91) |
Table 1: knowledge of the HPV and the HPV vaccine among parents attending paediatric outpatient clinics.
In order to measure behaviours, we enquired from parents (mothers) those who actually received the vaccine and found only 13/134 (9.7%) did. Further we also enquired from all parents if they had a child eligible to receive the vaccine if they had already taken at least one dose, and found only 8 (3.3%) were vaccinated, 2 males and 6 females. Notwithstanding as much as 152 (62.3%) parents expressed willingness to give their children the vaccine as well as acknowledging that it may be beneficial.
The HPV vaccine is being delivered at designated clinics and as a school-based program. We evaluated one such urban clinic serving a large population in North-Central Trinidad. The school health program began in 2013 of which only 11 children aged 9-12 were vaccinated. In 2014, 175 (4.4%) children had one dose and 37 (1%) completed 3 doses, however in 2015, only 10 (.25%) children were vaccinated all received 3 doses. At the designated clinic in 2014, 175 adults were vaccinated of which only 4 completed 3 doses. However in 2015, 275 adults were vaccinated of which 25 completed 3 doses.
Discussion
There are three key findings of this study. The first important finding was among parents with children eligible for the HPVc overall knowledge of HPV as well as the vaccine was low. Yet more parents indicated willingness to vaccinate their children. In other words there were high levels of willingness and acceptability of the HPVc but low levels of knowledge and awareness of HPV or HPVc. In a systematic review of 29 similar studies Perlman and colleagues reported similar findings, as well as Halliday and colleagues in the Bahamas [23,24]. Thus these findings continue to underscore the urgent need for more education to inform the public about HPV, HPVc, and cervical cancer, particularly to key demographics, (adolescents, parents and healthcare professionals), in order to leverage the high levels of willingness and acceptability of HPV vaccine, towards successful implementation of HPV vaccination programs. This is against a background in which studies from Australia one of the first countries to implement a HPVc program in 2007, have shown a large decline in genital warts, from 11.3% in 2007 to 3.1% in 2011 [25]. A previous study has shown that providing parents with an HPV information sheet did appear to improve knowledge about HPV; however, this increased knowledge had little effect on the acceptability of the vaccine by parents [26]. Instead, attitudes and life experiences seemed to be more important factors influencing HPV vaccine acceptability among parents [27].
The second key finding was very few parents understood the types and nature of the vaccine. This is particularly important in this setting, as one study has shown that the most common HPV high-risk types detected in the cervix of healthy Tobagonian women was HPV45 rather than HPV16 and 18 [28], and a pilot study in Trinidad showed HPV 52 (12.7%) was the most frequently occurring high-risk type, followed by HPV 66 (10.3%), HPV 16 (9.5%), and HPV 18 (8.6%) [29]. A similar study in Jamaica showed that the most common high-risk HPV types were HPV 45 (21.7%), compared to HPV 16 (18.4%), and HPV 18 (14.5%) [30]. HPV vaccination only protects against HPV types to which the individual has never been exposed. Most parents therefore are unlikely to make an informed decision, which raises ethical issues. Further most parents did not know that HPV infection is a sexually transmitted infection (STI). This raises the issues surrounding the proctection of children from STI in a multicultural, multireligious society
The third key finding was the law uptake particularly in the schoolbased program. The proportion of vaccinated girls in the school-based program is below expectations, particularly as this approach has proven to be efficient [31].
Our study contains some limitations. Participants were recruited from hospital-based clinics serving an ethnically diverse, predominantly low-income, population. The daughter's vaccination status was based on the participant's report only. We are however confident that we collected reliable estimates given that 1) many participants indicated that their daughter did not receive the vaccine, so overestimation of uptake is unlikely, and 2) girls could only receive the HPV vaccine with consent of an adult caregiver, so it is very likely that the mother accompanied them and thus knows the number of doses received. Strength of the study is data were obtained from the program itself and hence is a more reliable estimate of the true uptake.
Conclusion
In conclusion we provide evidence on parental barriers to the HPV vaccination program introduced in 2013 as well as the current situation. Vaccine-preventable diseases face many challenges, however vaccine refusal, is a critical but neglected component. Refusal of the polio vaccine in both Nigeria and Parkistan for example, has caused major setbacks to the global polio eradication. Many factors contribute to the development of clusters of people who refuse vaccines, including low priority, changing epidemiology and competing health issues. Resistance to vaccination can be overcome with carefully planned and executed social mobilization initiatives but requires substantial human and financial resources.
REFERENCES
- International Agency for Research on Cancer. Global cancer observatory. 2019.
- Forman D, de Martel C, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L, et al. Global burden of human papillomavirus and related diseases. Vaccine 2012;30:F12–23.
- Parkin DM, Almonte M, Bruni L, Clifford G, Curado MP, Piñeros M. Burden and trends of type-specific human papillomavirus infections and related diseases in the Latin America and Caribbean region. Vaccine 2008;26:L1–15.
- PAHO. Universal Health, Everyone, Everywhere. 2019.
- Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999;189:12–19.
- AK Chaturvedi, Engels EA, Pfeiffer RM. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol 2011;29:4294–4301.
- Gillison ML, Chaturvedi AK, Lowy DR. HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer 2008;113:3036–3046.
- CDC. Centres for disease control and prevention. 2019.
- Lacey CJ, Lowndes CM, Shah KV. Burden and management of non-cancerous HPV-related conditions: HPV-6/11 disease. Vaccine 2006;24:S35–41.
- Joura EA, Giuliano AR, Iversen OE, Bouchard C, Mao C, Mehlsen J, et al. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. N Engl J Med 2015;372:711–723.
- Gertig DM, Brotherton JM, Budd AC, Drennan K, Chappell G, Saville AM. Impact of a population-based HPV vaccination program on cervical abnormalities: a data linkage study. BMC Med 2013;11:227.
- Crowe E, Pandeya N, Brotherton JM, Dobson AJ, Kisely S, Lambert SB, et al. Effectiveness of quadrivalent human papillomavirus vaccine for the prevention of cervical abnormalities: case–control study nested within a population based screening programme in Australia. BMJ 2014;348:g1458.
- Baldur-Felskov B, Dehlendorff C, Munk C, Kjaer SK. Early impact of human papillomavirus vaccination on cervical neoplasia—nationwide follow-up of young Danish women. J Natl Cancer Inst 2014;106:djt460.
- Pollock KG, Kavanagh K, Potts A, Love J, Cuschieri K, Cubie H, et al. Reduction of low- and high-grade cervical abnormalities associated with high uptake of the HPV bivalent vaccine in Scotland. Br J Cancer 2014;111:1824–1830.
- Cox JT, Palefsky JM. Human papillomavirus vaccination. 2019.
- CDC. Teens Vaccination. 2019.
- Nelson R. HPV Vaccine Uptake Remains 'Unacceptably Low,' CDC Says. 2014.
- Presidents’s cancer panel annual report. Accelerating HPV vaccine uptake: Urgency for action to prevent cancer. 2019.
- Presidents’s cancer panel annual report. The case for HPV vaccination. 2019.
- Wong MC, Lee A, Ngai KL, Chor JC, Chan PK. Knowledge, attitude, practice and barriers on vaccination against human papillomavirus infection: a cross-sectional study among primary care physicians in Hong Kong. PLoS One. 2013;8:e71827.
- Al-Dubai SA, Alshagga MA, Al-Naggar RA, Al-Jashamy K, Baobaid MF, Tuang CP, et al. Knowledge, attitudes and barriers for human papilloma virus (HPV) vaccines among Malaysian women. Asian Pac J Cancer Prev. 2010;11:887-892.
- Walsh C, Gera A, Shah M, Sharma A, Powell J, Wilson S. Public knowledge and attitudes towards Human Papilloma Virus (HPV) vaccination. BMC Public Health 2008;8:368.
- Perlman S, Wamai RG, Bain PA, Welty T, Welty E, Ogembo JG. Knowledge and Awareness of HPV Vaccine and Acceptability to Vaccinate in Sub-Saharan Africa: A Systematic Review. PLoS ONE 2014;9:e90912.
- Halliday D, Butler R, Francis D, Thompson J, Joseph M, Ragin CC. Knowledge and attitudes toward HPV and the HPV vaccines in the Bahamas. West Indian med J 2013;62: 731-737.
- H Ali, B Donovan, H Wand. Genital warts in young Australians five years into national human papillomavirus vaccination programme: National surveillance data BMJ 2013;346: f2032.
- Fernández ME, Le YCL, Espada NF, Calo WA, Savas LS, Vélez C, et al. Knowledge, attitudes, and beliefs about human papillomavirus (HPV) vaccination among puerto rican mothers and daughters, 2010: A Qualitative Study. Prev Chronic Dis 2014;11:140171.
- Amanda F, Dempsey, Gregory D, Zimet, Robert L, Koutsky L. Factors That Are Associated With Parental Acceptance of Human Papillomavirus Vaccines: A Randomized Intervention Study of Written Information About HPV. Pediatrics 2006;117:1486-1493.
- Ragin CC, Wheeler VW, Wilson JB, Bunker CH, Gollin SM. Distinct distribution of HPV types among cancer-free Afro-Caribbean women from Tobago. Biomarkers 2007;12:510-522.
- Andall-Brereton GM, Hosein F, Salas RA, Mohammed W, Monteil MA, Goleski V, et al. Human papillomavirus genotypes and their prevalence in a cohort of women in Trinidad. Rev Panam Salud Publica 2011;29:220–226.
- Watt A, Garwood D, Jackson M, Younger N, Ragin C, Smikle M,et al. High-risk and multiple human papillomavirus (HPV) infections in cancer-free Jamaican women. Infect Agent Cancer 2009;4:S11.
- Paul P, Fabio A. Literature review of HPV vaccine delivery strategies: Considerations for school- and non-school based immunization program. Vaccine 2014;32:320–326.
Citation: Mungrue K (2019) Human Papilloma Virus Vaccine Access and Use-The First Three Years After Introduction. J Vaccines Vaccin 10:398. doi: 10. 24105/2157-7560.10.398
Copyright: © 2019 Mungrue K, et al.. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.