Indexed In
- The Global Impact Factor (GIF)
- CiteFactor
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Virtual Library of Biology (vifabio)
- International committee of medical journals editors (ICMJE)
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 20, Issue 7
Huge Osteosarcoma of Mandible in a 16 Year Girl: A Case Report
Prabhat Chandra Thakur1, Pravin Kumar Jaiswal1*, Sishir Sharma2, Surendra Basnet2, Krishna Nagarkoti2 and Sudeep Amatya22Department of Plastic Surgeon, Nepal Cancer Hospital, Lalitpur, Kathmandu, Nepal
, DOI: 10.35248/2247-2452.21.20.1143
Abstract
Osteosarcomas are primary malignant bone tumors in which mesenchymal cells produce osteoid. It is generally the most common malignant bone neoplasm, although lesions of the jaw are uncommon. Osteosarcoma of the Jaw (JOS) presents a lower incidence of metastasis and a better prognosis than osteosarcoma of the long bones. However, patients with JOS can exhibit advanced tumors, mainly when early diagnosis is not performed. This article reports on a case of an advanced osteosarcoma of the mandible. A 16-year-old lady came for evaluation and treatment of lower jaw mass. The patient had been noticing loose teeth and progressively enlarging mass since 3 months. Computed tomography showed large heterogenous lesion measuring 8.4 × 6.8 cm arising from mandible with cortical destruction and periosteal reaction. She had undergone incisional biopsy which revealed ill circumscribed subepithelium tumor with alternating areas of chondromyxoid and fibrocellular components, foci of osteoid formation, areas of ischemia type of necrosis, abscess formation and established the diagnosis as osteosarcoma of bone chondroblastic type. The patient was then recommended for oncologic treatment with 2 cycles of pre-operative chemotherapy. She received 1 cycle NACT (adriamycin+cisplastin), but as the disease was progressing quickly, so she was referred to our centre and underwent surgery.
Keywords
Oral cancer, Osteosarcoma, Jaw, Free flap, Reconstructive surgery.
Introduction
Osteosarcomas are rare malignant tumors of the connective tissues which originate from undifferentiated mesenchymal cells that are the precursors of osteoid tissue [1]. Approximately 7% of osteosarcomas form in the jaws [2–4]. Peak age for jaw tumors being 30 to 39 years. Males slightly outnumber females in reported cases [1,3,5].
In this report we present a case of osteosarcoma of the mandible in a 16-year-old female. Two months after the clinical appearance of the swelling, the patient underwent surgery. This case is unique in that the age of occurrence and the biologic behavior of the tumor were not consistent with the reported literature. The case report is followed by a discussion of osteosarcoma of the jaw pertaining to its clinical presentation, diverse radiologic appearance, varied histopathologic picture, and prognosis.
Case Presentation
A 16-year-old female presented to the outpatient department with complaints of swelling over her middle 3rd of lower jaw for the last 2 months. There was also associated history of loosening of teeth above the swelling. On clinical examination, there was a hard, nontender swelling, around 8 cm × 8 cm in size involving the middle 3rd of the mandible. It was extending anteriorly from 1st molar to 1st molar of contralateral side. It seemed to be infiltrating the lower alveolus and the gingivobuccal sulcus. The patient had no trismus, and the rest of the oral cavity did not present any abnormal findings.
A CT scan of the face and neck showed a 4 cm × 3 cm × 5 cm expansile lesions over the ramus of the left half of the mandible which was hypointense on T2-weighted images. The biopsy of the swelling revealed osteosarcoma of bone, chondroblastic type.
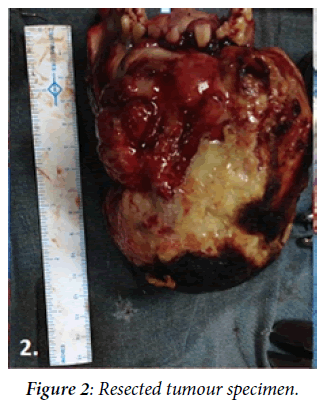
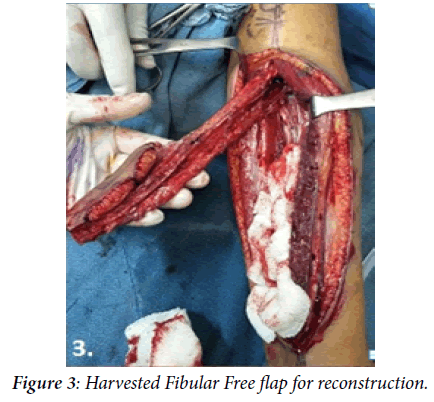
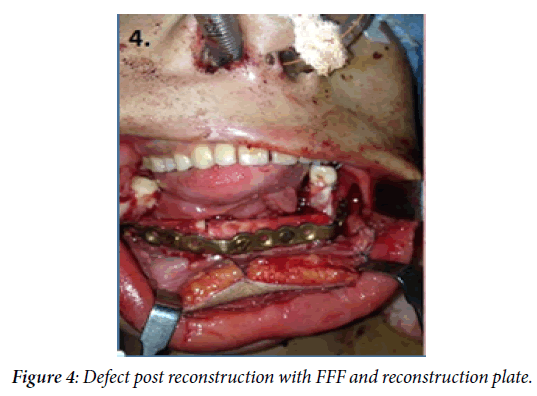
With this clinicoradiological picture, the patient was treated with neoadjuvant chemotherapy, with 1 cycle of adriamycin, and cisplatin. On completion of 1st cycle chemotherapy, tumor size had increased. The case was discussed in the multimodality tumor board, and in view of the patient's young age and the due to no response of her disease to chemotherapy, it was decided to treat her with a curative intent through surgery. She underwent a wide local excision of the tumor with a middle 3rd mandibulectomy and osteomyocutaneous fibular free flap. The postoperative histology showed clear margins with post chemotherapy changes. Patient was planned for adjuvant chemotherapy but she refused for it. She was kept on a three monthly follow-up and is continuing till now.
Results and Discussion
Osteosarcoma is a rare malignant tumor of the bone. The mandible presents a rare site of involvement with a distinct clinical profile with an older age of presentation and lesser chances of distant metastasis. Clinically, OS of the jaw bones tends to present commonly as a swelling with associated paresthesia which is dissimilar from the presentation of the disease of long bones where pain during activity is the more common complaint [5].
Radiologically, osteosarcoma can appear with a variable bone density depending on the amount of bone formed by the neoplasm. In some cases “sunray” appearance is observed at the periphery of the tumor. Widened periodontal ligament space has been described as a classical sign of early osteosarcoma [6]. The widening of periodontal ligament space and inferior dental canal, together with sunburst effect are almost pathognomonic of OS of the jaw bone, but not all lesions may show these characteristics [7].
CT and MRI are valuable adjuncts in evaluating the extent of the tumor and its relationship with neighboring tissues [8]. Differentiation of osteosarcoma from other bony lesions like Paget’s disease, fibrous dysplasia, multiple myeloma, and metastatic tumors is based more on microscopical than radiological evidence [9] (Figures 1-6).
Figure 1: Pre-Operative Image.
Figure 2: Resected tumour specimen.
Figure 3: Harvested Fibular Free flap for reconstruction.
Figure 4: Defect post reconstruction with FFF and reconstruction plate.
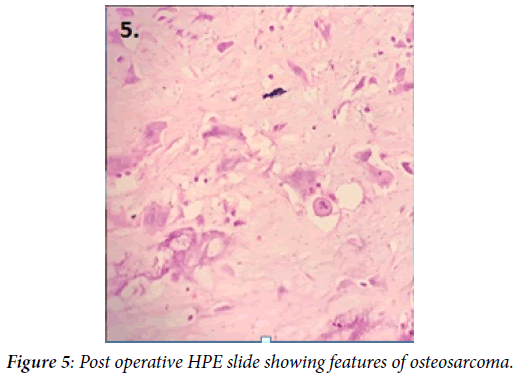
Figure 5: Post operative HPE slide showing features of osteosarcoma.
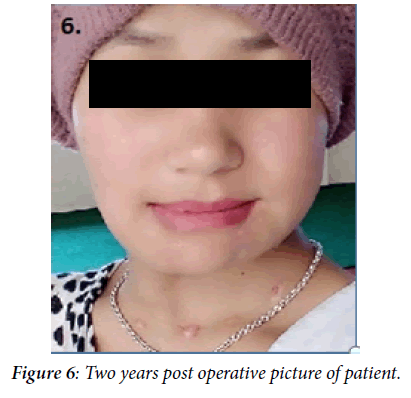
Figure 6: Two years post operative picture of patient.
Besides the size of the lesion, the histologic type and grading of the tumor are important factors in determining the prognosis. Histologically, they are composed of malignant spindle cells which produce foci of osteoid or immature bone. Conventional osteosarcoma can be subdivided into osteoblastic, chondroblastic, and fibroblastic histologic variants depending on the extracellular matrix produced by the tumor cells [1]. In the jaws, about half of the lesions demonstrate a cartilaginous differentiation [10]. In general, osteosarcomas of the jaws tend to be better differentiated than in long bones [11,12].
Histologic picture of the present case showed areas of chondroblastic type with post chemotherapy changes of anterior buccal mucosa, grade 1. Mitosis was 2/10 hpf, necrosis was not identified. The histological grading is thought to be more important than all the other features combined in determining the prognosis.
Pathologically, conventional high-grade intramedullary OS comprisesabout 80% of the tumors [13]. Low-grade intramedullary OS is <2%, and the others include parosteal and periosteal OS accounting for <5%. Majority of mandibular OSs are conventional. OS spreads microscopically through the narrow spaces between bone tissue with other possible routes being the mandibular canal and the structures which connect the intraosseous components and soft tissues, such as the periodontal ligament and the mental and inferior alveolar nerves. Route of distant metastasis is hematogenous with the most common site being the lungs.
The prognosis of osteosarcoma of the jaws is better than that of long bone, with a 5-year-survival rate of 34.8 percent for the mandible. The median survival time is 6.5 years for the mandible [14]. Usually, the prognosis of a jaw osteosarcoma gets better as the age at which it occurs increases [5]. Older patients are reported to have increased resistance to the tumor, thus increasing the chances of a better prognosis [15]. OS of the jaw has a clinically distinct profile from that of the long bones although early and prompt diagnosis with interplay of surgery and chemotherapy remain the cornerstone of management.
Early diagnosis and complete tumor resection are the most important factors in increasing prognosis of jaw osteosarcomas [16]. Treatment of osteosarcoma is radical surgery [17]. This usually is accompanied by radiotherapy or chemotherapy. Anatomic limitations in the orofacial region cause difficulties in achieving uninvolved margins and for this reason local recurrence of the lesions is high between 33% and 39%. Tumor-free margins in surgery, chemotherapy with multidrugs, and radiotherapy after surgery have effects in the prognosis of osteosarcoma [18].
Conclusion
Jaw osteosarcoma is an aggressive neoplasm with high mortality and less distant metastases. Early diagnosis and radical surgery with good reconstruction and followed by adjuvant chemotherapy have been found to be with good prognosis. In this patient delayed diagnosis and non-response to neoadjuvant chemotherapy was seen. She underwent radical surgery and again adjuvant chemotherapy and is in good health. Overall in jaw osteosarcoma it is wise to go for surgery first followed by adjuvant therapy if the lesion is respectable.
REFERENCES
- Bennett JH, Thomas G, Evans AW, Speight PM. Osteosarcoma of the jaws: a 30-year retrospective review. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2000;90(3):323-333.
- Mardinger O, Givol N, Talmi YP, Taicher S. Osteosarcoma of the jaw: the Chaim Sheba Medical Center experience. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2001;91(4):445-451.
- Ogunlewe MO, Ajayi OF, Adeyemo WL, Ladeinde AL, James O. Osteogenic sarcoma of the jaw bones: a single institution experience over a 21-year period. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2006;101(1):76-81.
- AJ A. A retrospective clinicopathological study of 59 osteogenic sarcoma of jaw bone archived in a stomatology unit. Malays J Pathol. 2010;32(1).
- Garrington GE, Scofield HH, Cornyn J, Hooker SP. Osteosarcoma of the jaws. Analysis of 56 cases. Cancer. 1967;20(3):377-391.
- Gardner DG, Mills DM. The widened periodontal ligament of osteosarcoma of the jaws. Oral Surgery, Oral Medicine, Oral Pathology. 1976;41(5):652-656.
- Lindqvist C, Teppo L, Sane J, Holmström T, Wolf J. Osteosarcoma of the mandible: Analysis of nine cases. J Oral Maxillofac Surg. 1986;44(10):759-764.
- Wilner D. Radiology of bone tumors and allied disorders. 1982.
- Roca AN, Smith Jr JL, Jing BS. Osteosarcoma and Parosteal Osteogenic Sarcoma of the Maxillaand Mandible: Study of 20 Cases. Am J Clin Pathol. 1970;54(4):625-636.
- Vege DS, Borges AM, Aggrawal K, Balasubramaniam G, Parikh DM, Bhaser B. Osteosarcoma of the craniofacial bones: a clinico-pathological study. J Craniomaxillofac Surg. 1991;19(2):90-93.
- Unni KK, Dahlin DC, McLeod RA, Pritchard DJ. Intraosseous well‐differentiated osteosarcoma. Cancer. 1977;40(3):1337-1347.
- Fernandes R, Nikitakis NG, Pazoki A, Ord RA. Osteogenic sarcoma of the jaw: a 10-year experience. J Oral Maxillofacl Surg. 2007;65(7):1286-1291.
- Klein MJ, Siegal GP. Osteosarcoma: anatomic and histologic variants. Am J Clin Pathol. 2006;125(4):555-581.
- Patel SG, Meyers P, Huvos AG, Wolden S, Singh B, Shaha AR, et al. Improved outcomes in patients with osteogenic sarcoma of the head and neck. Cancer. 2002;95(7):1495-1503.
- Slootweg PJ, Müller H. Osteosarcoma of the jaw bones Analysis of 18 cases. J Maxillofac Surg. 1985;13:158-166.
- Russ JE, Jesse RH. Management of osteosarcoma of the maxilla and mandible. Am J Surg. 1980;140(4):572–576.
- Smeele LE, Van Der Wal JE, Van Diest PJ, Van Der Waal I, Snow GB. Radical surgical treatment in craniofacial osteosarcoma gives excellent survival. A retrospective cohort study of 14 patients. European Journal of Cancer Part B: Oral Oncology. 1994;30(6):374-376.
- August M, Magennis P, Dewitt D. Osteogenic sarcoma of the jaws: factors influencing prognosis. Int J Oral Maxillofac Surg. 1997;26(3):198-204.