Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 9, Issue 4
High Blood Pressure and Obstructive Sleep Apnea: A Cross-Sectional Study
S Duong-Quy1,2,3, K Dang-Thi-Mai4, H Tran-Do5, K Tran-Quang5, Q Vu-Tran-Thien6,7, K Bui-Diem6,7 and V Nguyen-Nhu7,8*2Department of Respiratory Physiology, Penn State Medical College, PA, USA
3Department of Respiratory Physiology, Pham Ngoc Thach Medical University, HCM City, Vietnam
4Department of Respiratory Diseases, Cho Ray Hospital, HCM City, Vietnam
5Can Tho University of Medicine and Pharmacy, Can Tho, Vietnam
6Department of Physiology, Pathophysiology and Immunology, University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam
7Department of Respiratory Functional Exploration, University Medical Center, Ho Chi Minh City, Vietnam
8Department of Family Medicine, University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam
Received: 02-Jul-2021 Published: 23-Jul-2021, DOI: 10.35248/2329-6925.21.9.418
Abstract
Objective: To investigate the clinical features in Obstructive Sleep Apnea (OSA) patients with High Blood Pressure (HBP) Method: It was a descriptive cross-sectional study. There were 164 subjects underwent respiratory polygraph in sleep lab, including 141 OSA patients who were divided into 2 groups: OSA-HBP (n=76) and OSA-non-HBP (n=65). Clinical and respiratory polygraphy characteristics of two groups were analyzed.
Results: Two groups of patients did not differ significantly with regard to the main characteristics, including Body Mass Index (BMI), Apnea-Hypopnea Index (AHI) and Oxygen Desaturation Index (ODI). Systolic Blood Pressures (SBP) were higher in HBP patients (p=0.011). ESS (Epworth Sleepiness Scale) was not significantly different between two groups. EDS (Excessive Daytime Sleepiness) percentage was higher in OSA-HBP group than OSA-non-HBP group (p=0.024). SBP were correlated with desaturation time measured by respiratory polygraphy (p=0.024).
Conclusion: In patients with OSA, the frequency of EDS was significantly higher in subjects with HBP. Hence, the daytime sleepiness may be used as a potential and relevant clinical symptom to screen HBP subjects with OSA.
Keywords
Obstructive sleep apnea; High blood pressure; Apnea hypopnea index; Epworth sleepiness scale
Introduction
Obstructive Sleep Apnea (OSA) is characteristic by short hypopneas and apneas which last more than ten seconds and repeat during sleep due to partial or total collapse of the upper airway [1]. The prevalence of OSA in Vietnam had been 8.5% following EPSASIE study reported in 2018 [2]. Previous observed study has shown the prevalence of hypertension (high blood pressure: HBP) comorbid with OSA varied from 30% to 80%, within high prevalence in resistant (refractory) hypertension [3]. Many cross-sectional studies regarding the relationship between OSA and hypertension suggest that OSA might be considered as an independent risk factor of hypertension [4,5]. OSA is also a risk factor for other cardiovascular diseases such as coronary disease, arrhythmia, heart failure and stroke, etc.… [6,7]. OSA is also a risk factor to develop cardiovascular events during the night including heart attack, coronary infarction or sudden death due to increasing catecholamine and sympathetic activity related to intermittent hypoxia [8,9].
Therefore, it is necessary to clarify the clinical and Para clinical symptoms related to sleep disorders at night and daytime sleepiness in patients with HBP to predict OSA in these patients; that might increase the accuracy of OSA diagnosis in patients with HBP.
Materials and Methods
Subjects >18 years responded to inclusion criteria were included in the present study. All study subjects were included from November 2017 to November 2019. The present study was approved by Institutional Review Board.
Inclusion criteria
Patient with suspected OSA who came to the consultation for doing respiratory polygraphy which confirmed the diagnosis of OSA with apnea-hypopnea index (AHI) ≥ 5/hour; and all included patients had been accurately measured blood pressure at admission.
Exclusion criteria
Patients did not accept to participate in the study; patients had an uncontrolled or severe crisis HBP; patients who had acute cardio- respiratory diseases or infectious problems.
Study population
Patients with suspected OSA who had been undergone respiratory polygraphy and had blood pressure measurement at admission were included in the present study. OSA patients were diagnosed with AHI ≥ 5/hour. They were divided into two groups: non-HBP/ OSA and HBP/OSA patients.
Study procedure
Respiratory Polygraphy (CIDELEC®, France) with 7 channels including nasal flow sensor, snoring sensor, ECG, positional sensor, thoracic and abdominal belts, pulse oxygen saturation sensor.
Respiratory Polygraphy (RP) data, including apnea, hypopnea, AHI, and SpO2 were used for analysis. The software CIDELEC 2.0 gave the result first, and then the investigator re-scored and confirmed the result. The American Academy of Sleep Medicine scoring manual 2005 was used for scoring of respiratory events. Apnea was defined as complete cessation of airflow for at least 10 seconds in duration and hypopnea as >50% amplitude reduction of airflow lasting at least 10 seconds or associated with 4% desaturation during sleep. AHI was used to confirm OSA diagnosis and OSA severity: AHI < 5/hour = non-OSA, 5≤AHI<15/hour = mild OSA, 15≤AHI<30/hour = moderate OSA, AHI≥ 30 /hour = severe OSA. All study subjects underwent respiratory polygraphy in the DRD of Cho Ray hospital, Ho Chi Minh City.
Statistical analysis
Quantitative variables were presented as mean ± Standard Deviation (SD) and qualitative variables were presented as frequency or percentage. Comparison of independent groups was performed by sample T-test or Analysis of Variance (ANOVA). Categorical variables were compared by chi-square’s exact tests. The correlation between different variables was evaluated by Pearson or Spearman correlation test based on normal distribution or none. All analyses were conducted with SPSS 22.0 (SPSS Inc, Chicago, IL, USA). The p<0.05 was considered statistically significant.
Results
Clinical characteristics of OSA patients
One hundred forty one OSA patients were included in the present study and divided into 2 groups: OSA-non-HBP (n=76) and OSA- HBP (n=65). The mean age of study subjects was 53.5±14.7 years; male was dominant with 76.6%. The anthropometric characteristics of OSA patients are presented in Table 1.
| Non-HBP, n=76 | HBP, n=65 | p | |
|---|---|---|---|
| Male, n (%) | 58 (76.3) | 50 (76.9) | 1 |
| Age, years | 47.0 ± 13.5 | 61.0 ± 12.4 | <0.001 |
| AHI /h, mean±SD | 47.2 ± 23.7 | 47.0 ± 24.0 | 0.978 |
| BMI, kg/m2, mean±SD | 27.8 ± 4.8 | 28.5 ± 5.5 | 0.051 |
| ESS, mean±SD | 8.7 ± 4.5 | 9.9 ± 5.1 | 0.167 |
| Neck circumference, cm | 40.1 ± 3.8 | 41.3 ± 3.6 | 0.059 |
| Waist circumference, cm | 98.7 ± 11.4 | 106.9 ± 11.4 | <0.001 |
Note: ESS: Epworth Sleepiness Scale, BMI: Body Mass Index, AHI: Apnea Hypopnea Index.
Table 1: Characteristics of OSA patients.
There was no significant difference between 2 groups for systolic and diastolic blood pressures (Sys BP and Dias BP) (Figure 1). Among 65 OSA-HBP patients, the percentage of each anti-hypertensive treatment was as following: calcium-channel treatment: 47% (n=30), angiotensin II blockers: 34% (n=22), beta blockers: 8% (n=5), and angiotensin-converting enzyme inhibitors: 27% (n=17). The percentage of patients receiving bi-therapy was 14% (n=9), triple therapy with diuretics: 3% (n=2).
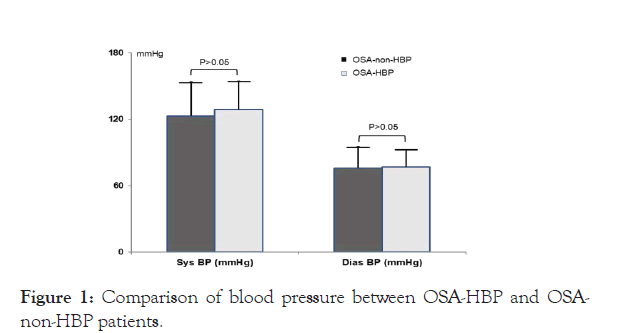
Figure 1: Comparison of blood pressure between OSA-HBP and OSA- non-HBP patients.
Comparison of ESS in OSA-HBP vs OSA-non-HBP
ESS was used to evaluate the daytime sleepiness severity (ESS>10). The frequency of excessive daytime sleepiness in OSA-HBP group was significantly higher than OSA-non-HBP group (44.6% vs 30.3%; p=0.039) (Figure 2). In severe OSA group, the frequency of EDS in patients with HBP was significantly higher than those in non-HBP group (Figure 3).
Figure 2: Comparison of excessive daytime sleepiness (EDS) frequency between OSA-HBP vs OSA-non-HBP patients.
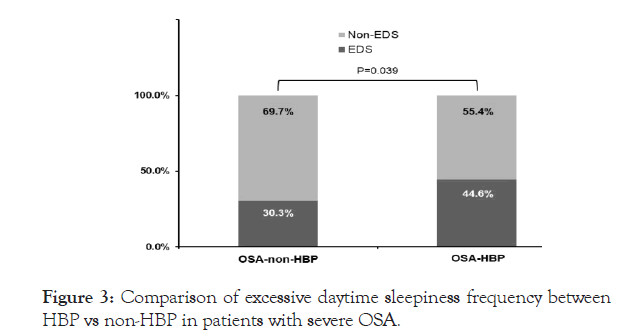
Figure 3: Comparison of excessive daytime sleepiness frequency between HBP vs non-HBP in patients with severe OSA.
Correlation between blood pressures with clinical and respiratory polygraphy parameters
Systolic and diastolic blood pressures were not significantly correlated with AHI and minimum saturation (Table 2). Sys BP were significantly correlated with desaturation time, BMI, and neck and waist circumferences (p<0.05 and p<0.01). Dias BP were only significantly correlated with BMI (p<0.05;) (Table 2) & Pearson’s correlation, *p<0.05; **p<0.01.
| AHI | Min SpO2 | Desaturation time | BMI | Neck cir | Waist circ | |
|---|---|---|---|---|---|---|
| Sys BP | 0.08 | -0.136 | 0.190* | 0.212* | 0.206* | 0.235** |
| DiasBP | 0.133 | -0.099 | 0.122 | 0.188* | 0.122 | 0.154 |
Note: Sys BP: Systolic blood pressure; Dias BP: Diastolic blood pressure, Neck cir: Neck circumference, Waist cir: Waist circumference.
Table 2: Correlation between blood pressure and respiratory polygraphy and demographic parameters.
Discussion
In the present study, 141 patients were included and divided into two groups depending on their blood pressure (HBP or non-HBP). The results showed that there were not any significant differences between OSA-HBP vs OSA-non-HBP patients for anthropometric features excepting waist circumference (Table 1). In the present study, ESS was used to compare daytime sleepiness severity between study patients. Although ESS was not significantly different between two groups, the percentage of patients with EDS in OSAHBP group was significantly higher than that in OSA-non-HBP group (Figures 2 and 3).
It is obvious that the use of ESS to predict OSA in patients with or without HBP is still controversial. In study realized by Martynowicz, et al. Including 374 subjects with OSA, the mean ESS in HBP group was significantly lower than non-HBP group [10]. The author suggested that OSA might be more difficult to diagnose in hypertensive patients than non-hypertensive patients. Therefore, ESS is a typical symptom of OSA but it is not a relevant clinical feature to differentiate OSA patients with or without systemic hypertension.
In the present study, the percentage of OSA patients who had EDS >10 had been compared between HBP and non-HBP groups. The result showed that the percentage of OSA-HBP patients with significant EDS was higher than OSA-non-HBP (Figure 2). Previous studies also demonstrated the high prevalence of EDS in patients with OSA-HBP and it was varied from 30% to 37% [11,12]. In patients with OSA, the increased risk of hypertension has been explained by the increase of sympathetic activity due to intermittent hypoxia related to apnea and hypopnea events during sleep. Meanwhile, sympathetic activation in OSA might have an impact on systemic hypertension via the mechanism related to baroreceptor and parasympathetic receptor [13,14].
In the present study, systolic blood pressure associated with neck, waist circumference and BMI. The previous studies had the similar results with neck, waist circumference and BMI correlated with blood pressure [15-17]. The mechanism of this association was not clear. Some researches favored the theory of the correlation of BMI or waist circumference with blood pressure due to the increase of free fatty acid, insulin resistance or vascular endothelial dysfunction; and oxidative stress as a mechanism of this complex association [15]. Besides that, OSA has been found as a risk factor of hypertension due to the imbalance of the autonomic nervous system [18]. The correlation between systolic blood pressure and desaturation time was also described in the present study. Obviously, chronic intermittent hypoxia induces oxidative stress; vascular endothelial dysfunction inducing systemic hypertension has been considered as a risk factor of cardiovascular diseases [19-21] and related to the reduction of endothelial NO synthase inducednitric/ nitrate production [22-24]. However, this detrimental effect might be reversed under target treatment [25-27]. Therefore, the use of exhaled NO might be useful in the screening OSA patients with endothelial dysfunction [28-30]; especially, it might be useful in developing country with high prevalence of OSA and other comorbidities associated with OSA in children and adult [31-36].
Finally, besides giving relevant additional information to the clinical practice for OSA patients with hypertension, the present study has some limitations related to a small number of study subjects, the use of portable polygraphy for diagnosing OSA and the lack of CPAP treatment follow-up.
Conclusion
The presence of high frequency of EDS in OSA patients with hypertension is useful for screening HBP in OSA. While ESS is not depending on the co-existence of HBP in OSA, other clinical parameters such as BMI, neck and waist circumferences and desaturation time during sleep were significantly correlated with blood pressures. Therefore, all subjects with hypertension should be screened for OSA.
Conflict of Interest
None
REFERENCES
- Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014; 383 (9918): 736-747.
- Duong Quy S, Dang Thi Mai K, Nguyen Xuan Bich H, Tran Van N, Hua Huy T, Chalumeau F, et al. EPSASIE : étude épidémiologique du syndrome d’apnées obstructives au cours du sommeil (SAOS) au Vietnam. Médecine du Sommeil. 2015;12(1):26-27.
- Marin JM, Agusti A, Villar I, Forner M, Nieto D, Carrizo SJ, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. Jama. 2012;307(20):2169-2176.
- Hla KM, Young TB, Bidwell T, Palta M, Skatrud JB, Dempsey J. Sleep apnea and hypertension. A population-based study. Ann Intern Med. 1994;120(5):382-388.
- Lavie P, Herer P, Hoffstein V. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ (Clinical research ed). 2000;320(7233):479-482.
- Shah NA, Yaggi HK, Concato J, Mohsenin V. Obstructive sleep apnea as a risk factor for coronary events or cardiovascular death. Sleep Breath. 2010;14(2):131-136.
- Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353(19):2034-2041.
- Gami AS, Howard DE, Olson EJ, Somers VK. Day-night pattern of sudden death in obstructive sleep apnea. N Engl J Med. 2005;352(12):1206-1214.
- Kuniyoshi FHS, Garcia-Touchard A, Gami AS, Romero-Corral A, van der Walt C, Pusalavidyasagar S, et al. Day-night variation of acute myocardial infarction in obstructive sleep apnea. J Am Coll Cardiol. 2008;52(5):343-346.
- Martynowicz H, Skomro R, Gac P, Mazur G, Porebska I, Brylka A, et al. The influence of hypertension on daytime sleepiness in obstructive sleep apnea. J Am Soc Hypertens. 2017;11(5):295-302.
- Broström A, Sunnergren O, Årestedt K, Johansson P, Ulander M, Riegel B, et al. Factors associated with undiagnosed obstructive sleep apnoea in hypertensive primary care patients. Scand J Prim Health Care. 2012;30(2):107-113.
- Seguro F, Bard V, Sedkaoui K, Riche M, Didier A, Bouhanick B. Screening obstructive sleep apnea-hypopnea syndrome in hypertensive patients: a comparative study of the efficiency of the Epworth sleepiness scale. BMC pulmonary medicine. 2018;18(1):173.
- Cortelli P, Lombardi C, Montagna P, Parati G. Baroreflex modulation during sleep and in obstructive sleep apnea syndrome. Auton Neurosci. 2012;169(1):7-11.
- Lombardi C, Parati G, Cortelli P, Provini F, Vetrugno R, Plazzi G, et al. Daytime sleepiness and neural cardiac modulation in sleep-related breathing disorders. J Sleep Res. 2008;17(3):263-270.
- Fan S, Yang B, Zhi X, He J, Ma P, Yu L, et al. Neck circumference associated with arterial blood pressures and hypertension: A cross-sectional community-based study in northern Han Chinese. Sci Rep. 2017;7(1):2620.
- Zhou J-y, Ge H, Zhu M-f, Wang L-j, Chen L, Tan Y-z, et al. Neck circumference as an independent predictive contributor to cardio-metabolic syndrome. Cardiovascular diabetology. 2013;12:76.
- Lee BJ, Kim JY. A comparison of the predictive power of anthropometric indices for hypertension and hypotension risk. PloS one. 2014;9(1):e84897-e.
- Calhoun DA. Obstructive sleep apnea and hypertension. Curr Hypertens Rep. 2010;12(3):189-195.
- Oyarce MP, Iturriaga R. Contribution of Oxidative Stress and Inflammation to the Neurogenic Hypertension Induced by Intermittent Hypoxia. Front Physiol. 2018;9:893.
- Saxena A, Little JT, Nedungadi TP, Cunningham JT. Angiotensin II type 1a receptors in subfornical organ contribute towards chronic intermittent hypoxia-associated sustained increase in mean arterial pressure. Am J Physiol Heart Circ Physiol. 2015;308(5):H435-H446.
- Kim SJ, Fong AY, Pilowsky PM, Abbott SBG. Sympathoexcitation following intermittent hypoxia in rat is mediated by circulating angiotensin II acting at the carotid body and subfornical organ. J Physiol. 2018;596(15):3217-3232.
- Duong-Quy S. Endothelial Dysfunction in Patients with Obstructive Sleep Apnea (OSA). J Vasc Med Surg. 2015;3(1):1-2.
- Tran-Van H, Vo-Thi-Kim A, Duong-Quy S. The Study of Correlation between Diurnal Blood Pressure with Nocturnal Oxygen Desaturation and Nitrite Production in Subjects with Obstructive Sleep Apnea (OSA). J Vasc Med Surg. 2017;5(3):317.
- Duong-Quy S, Dao P, Hua-Huy T, Le-Dong NN, Dinh-Xuan AT. Impairment of Pulmonary Vasoreactivity in Response to Endothelin-1 In Patients With Chronic Obstructive Pulmonary Disease (COPD). J Vasc Med Surg. 2015;3:213.
- Vo-Thi-Kim A, Nguyen-Xuan B, Dao-Van D, Duong-Quy S. The Effect of Continuous Positive Airway Pressure (CPAP) in Treatment of Patients with Refractory High Blood Pressure Associated with Severe Obstructive Sleep Apnea (OSA). J Vasc Med Surg. 2015;5:2.
- Tran-Van H, Vo-Thi-Kim A, Tran-Ngoc T, Duong-Quy S. Comparison of Long Term Oxygen-Therapy (LTOT) and LTOT Combined with Sildenafil and Simvastatin in the Treatment of Severe Chronic Obstructive Pulmonary (COPD) with Hypoxia at Rest and Severe Pulmonary Arterial Hypertension. J Vasc Med Surg. 2017;5(3):324.
- Dinh-Thi-Dieu H, Vo-Thi-Kim A, Tran-Van H, Duong-Quy S. Efficacy and adherence of auto-CPAP therapy in patients with obstructive sleep apnea: a prospective study. Multidiscip Respir Med. 2020;15(1):468.
- Dang-Thi-Mai K, Le-Dong NN, Le-Thuong V, Tran-Van N, Duong-Quy S. Exhaled Nitric Oxide as a Surrogate Marker for Obstructive Sleep Apnea Severity Grading: An In-Hospital Population Study. Nat Sci Sleep. 2021;13:763-773.
- Hua-Huy T, Le-Dong NN, Duong-Quy S, Luchon L, Rouhani S, et al. Increased alveolar nitric oxide concentration is related to nocturnal oxygen desaturation in obstructive sleep apnoea. Nitric Oxide. 2015;45:27-34.
- Duong-Quy S, Hua-Huy T, Tran-Mai-Thi HT, Le-Dong NN, Craig TJ, Dinh-Xuan AT. Study of Exhaled Nitric Oxide in Subjects with Suspected Obstructive Sleep Apnea: A Pilot Study in Vietnam. Pulm Med. 2016;2016:3050918.
- Dang-Thi-Mai K, Dang Vu T, Tran Van N, Nguyen Thi Hong A, Duong–Quy S. Obstructive Sleep Apnea (OSA) and Metabolic Syndrome (MetS). J Func Vent Pulm. 2020;11(33):36-41.
- Duong-Quy S, Dang Thi Mai K, Tran Van N, Nguyen Xuan Bich H, Hua-Huy T, Chalumeau F, et al. Study about the prevalence of the obstructive sleep apnoea syndrome in Vietnam. Rev Mal Respir. 2018;35(1):14-24.
- Nguyen-Hoang Y, Nguyen-Thi-Dieu T, Duong-Quy S. Study of the clinical and functional characteristics of asthmatic children with obstructive sleep apnea. J Asthma Allergy. 2017; 10:285-292.
- Nguyen-Thi-Hong L, Duong-Quy S. Obstructive Sleep Apnea Syndrome: The challenges in developing countries. J Func Vent Pulm. 2016; 22(7):1-2.
- Duong-Quy S. Obstructive Sleep Apnea (OSA) in children: Fact and challenge. J Func Vent Pulm. 2015; 9(27):1-2.
- Duong-Quy S. Sleep disorder in COPD: a forgotten entity. J Func Vent Pulm. 2015; 19(6):1.
Citation: Duong-Quy S, Dang-Thi-Mai K, Tran-Do H, Tran-Quang K, Vu-Tran-Thien Q, Bui-Diem K, et al. (2021) High Blood Pressure and Obstructive Sleep Apnea: A Cross-Sectional Study. J Vasc Med Surg. 9:418.
Copyright: © 2021 Duong-Quy S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

