Citations : 2345
Dentistry received 2345 citations as per Google Scholar report
Indexed In
- Genamics JournalSeek
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 10, Issue 6
Gingival Depigmentation Using CO2 Laser and Scalpel Technique with PRF Membrane-A Clinical and Histological Study
Waqas N. Ansari*, Sangeeta D. Muglikar, Prerna S. Ghodke, Rashmi V. Hegde, Salika Sheikh and Hamed BadaamReceived: 20-Jul-2020 Published: 24-Aug-2020, DOI: 10.35248/2161-1122.20.10.563
Abstract
Introduction: Gingival hyperpigmentation is the increase in pigmentation beyond the expected degree. There are various methods for the removal of pigmentation (depigmentation) which can be surgical stripping, use of lasers, chemicals etc. This is a spilt mouth study where surgical stripping and CO2laser depigmentation along with the added benefits of Platelet-Rich Fibrin (PRF) membrane have been evaluated clinically and histologically.
Materials and Method: 40 sites from 10 patients who were aesthetically conscious of their dark gums were enrolled in the study and a spilt mouth treatment protocol was followed where there were 4 groups as follows: 1) Group 1: CO2laser sites with PRF membrane (n=10). 2) Group 2: CO2 laser sites without PRF membrane (n=10). 3) Group 3: Scalpel technique/surgical stripping sites with PRF membrane (n=10). 4) Group 4: Scalpel technique/surgical stripping sites without PRF membrane (n=10). All the above groups were performed on one patient in one single sitting and by a single operator and follow up were done at 1 day, 1 week and 10 days assessing the visual analogue scales and landrys wound healing index. Histological specimen was obtained on the 7th day from the lateral incisor regions of all four groups.
Results: At day 1 of the follow up it was noticed that Group 1 had the least pain, followed by Group 3 and then the groups where PRF membrane was not used. At 10 days post operatively, all the groups showed no pain. Considering healing index, also the groups with PRF membrane showed better healing as compared to the groups where PRF membrane was not used. Therefore it was shown in the study that PRF membrane has helped in better healing as well and reducing the pain post operatively.
Conclusion: Within the limitations of the study, it can be concluded that, CO2laser with PRF membrane has shown faster healing and lesser pain perception therefore it can be used as a routine procedure for depigmentation.
Keywords
Depigmentation; CO2 laser; Platelet rich fibrin
Introduction
Gingival hyperpigmentation, that is the overproduction of melanin pigment, mostly seen in the anterior region of the gingiva, is a common esthetic concern especially in persons with high smile line or excessive gingival display. The most commonly seen melanin pigmentation occurs as a diffuse, deep purplish to brown discoloration which can be uniform or patched [1]. Dummett classified pigmentation into 6 types which are melanin, melanoid, carotene, reduced hemoglobin, oxyhemoglobin and soft keratin [2-6].
Gingival melanin hyperpigmentation can also be divided into physiologic (racial or physiologic) and pathologic (manifestation of systemic disease) can be endogenous or exogenous (exposure to UV light, drug-related, chemical, etc) [7].
It can be seen as early as 3 months on the gingiva of the new born infant. It is seen with a higher prevalence in the anterior region as compared to the posterior. Physiologic gingival hyperpigmentation is due to melanin (a non-hematogenous pigment) which is present in the basal and suprabasal laser of the epithelium and also can be present in small amounts in the underlying connective tissue as well. The cells producing melanin pigment are melanocytes which are synthesized in organelles called as premelanosomes or melanosomes. A study done by Lerner AB, et al. [8], found that a ratio of 1:15 (melanocyte/basal keratinocyte) is present in the human gingival epithelium. It is not the number, but the hyperactivity of the melanocytes that cause the pigmentation to be darker for a few individuals. Individuals, regardless of their race, have the same number of melanocytes approximately [8].
Generally, the pigmentation does not pose as a medical condition/ emergency that requires immediate treatment, but esthetic concerns can lead the patients to seek cosmetic treatment for the removal of pigmentation or so called “dark patches”. Gingival depigmentation can be performed by various techniques, sometimes giving immediate results. Techniques such as abrasion using a large round diamond bur [9], surgical methods (scalpel technique [10], electrosurgery [11], cryosurgery [12]), lasers (Argon laser, Carbon dioxide laser, Diode laser, Nd:YAG laser, Er:YAG laser and Er:Cr:YSGG laser) [13,14] methods to mask pigmentation (free gingival grafts, subepithelial connective tissue graft and acellular dermal matrix allografts), radiosurgery and ascorbic acid application have been used effectively [15].
Depigmentation is a procedure which leads to the formation of a wound that heals with secondary intention. Wound healing for various surgical protocols used for depigmentation is different. In surgical stripping (scalpel technique) complete wound healing is seen after 7 weeks where the newly formed gingiva is nonpigmented [16].
Depending upon the wavelength of laser used, the rate of wound healing can differ when compared to the healing following surgical stripping (scalpel technique). After depigmentation with lasers, generally the wound is covered with a yellowish white layer which is a layer of denatured protein coagulum which acts like a biologic dressing and protects the wound. It takes approximately 2 weeks for complete re-epithelization. After one month the depigmented gingiva resembles that of an untreated gingiva [17].
Platelet concentrates have recently gained importance in soft tissue surgeries because of the presence of numerous growth factors and faster wound healing ability. Choukroun [17], developed the concept of Platelet Rich Fibrin (PRF) in 2001. Since then numerous studies have been conducted regarding the healing potential of the same. With fundamental considerations, PRF can be considered to be a natural fibrin-based biomaterial favorable to the formation of a micro vascularization and able to guide epithelial cell migration to the surface. The interest of such a membrane is evident, namely, to protect open wounds and accelerate healing. It belongs to a new generation of platelet concentrates with simplified processing and without biochemical blood handling. It has shown faster wound healing by accelerated tissue cicatrization due to the development of effect neovascularization and nearly the total absence of infectious events. In this study, PRF membrane was used to cover the wounds after surgical stripping and CO2laser depigmentation. It acts as a soft tissue bandage when used on wounds that heal by secondary intention. PRF is an immune and a platelet concentrate which collects the factors on a single fibrin membrane which favors healing and immunity [18-20].
Platelets and leukocytes have the prime role in the biology of this material, but the fibrin matrix supporting them constitutes the determining element responsible for the real therapeutic potential of PRF [21]. The biologic effects of this PRF membrane are divided into 4 main aspects of healing that are angiogenesis, immune control, harnessing the circulating stem cells and wound protection by epithelial cover [22-24].
Many studies have been performed where the usage of periodontal packs has or has not been done following gingival depigmentation, leading to this topic, of covering a depigmentation wound, to be a controversy.
PRF membrane does have added benefits when used over open wounds, therefore this study was taken up to compare the effects of PRF membrane as a biologic dressing on depigmented sites using surgical stripping and CO2 laser in terms of wound healing, pain perception of the different treatments and histological analysis.
Aim of the study
The aim of the study was to compare the effects of PRF membrane on sites treated with CO2 laser and surgical stripping for depigmentation, clinically and histologically.
Material and Methods
Study design
A split mouth prospective study was conducted in the Department of Periodontology at MA Rangoonwala College of Dental Sciences and Research Centre, in Pune, India. 40 sites from 10 patients who were esthetically conscious of their dark gums and wanted treatment were selected for this study. As all the groups were present in one patient, they served as their own controls while comparing the effect of PRF membrane in CO2 and in surgical stripping depigmentation. Ethical clearance was obtained from the local ethical committee of the institution after the study was approved by the Internal Review Board (IRB).
Inclusion criteria
Systemically healthy individuals within the range of 15-50 years of age who had moderate to severe dark, continuous bands of pigmentation and hedin melanin index (1977) 3 score of 4, between the canines were included in the study (Figure 1A).
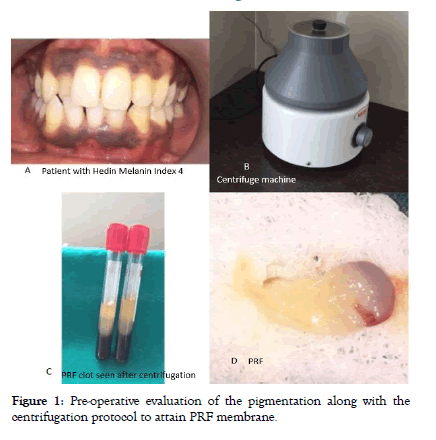
Figure 1: Pre-operative evaluation of the pigmentation along with the centrifugation protocol to attain PRF membrane.
Exclusion criteria
Patients with the habit of smoking or use of any other oral substance abuse, presence of gingival recession, missing teeth in the anterior region, patients on any form of Non-Steroidal Anti-Inflammatory Drug (NSAIDS), pregnant and lactating mothers and patients with any systemic involvement were excluded from the study.
Once the patients were selected based on the inclusion and exclusion criteria, they were made aware of what surgical protocol would be performed and also the use of platelet concentrates (PRF membrane) which would be obtained from their own blood. A verbal and written informed consent was procured from the participants of the study.
Allocation of sites as follows:
Group 1: CO2 laser sites with PRF membrane (n=10).
Group 2: CO2 laser sites without PRF membrane (n=10)
Group 3: Scalpel technique/surgical stripping sites with PRF membrane (n=10)
Group 4: Scalpel technique/surgical stripping sites without PRF membrane (n=10)
After the application of PRF membrane, interrupted sutures were given to hold the membrane in place for Group 1 and 3. Coe pack was applied in all four groups immediately following treatment and all the sites were treated on the same patient in a single day. The entire procedure was performed and evaluated by a single independent operator. The patients were asked not to perform any oral hygiene methods in the operated area for 3 days after the procedure. Chlorhexidine mouthwash was prescribed to them to be used twice daily for the next 15 days. Patients were asked to take painkillers of choice if they had any pain or discomfort following the procedure. Patient was recalled on the next day to assess the parameters and in this visit the coe-pak was removed. The sutures were removed on the 7th day post-surgery. The tissues were examined clinically at one week and 10 days and histological specimens were obtained on the 7th day post-surgery.
The parameter assessed pre-operatively was the hedin melanin index, given in the year 1977 with 5 stages of pigmentation starting from 0-4 where, 0=no pigmentation, 1=one or two solitary units of pigmentation in the papillary gingiva, 2=>3 units of pigmentation in the papillary gingiva without formation of a continuous ribbon, 3=>1 short continuous ribbons of pigmentation and 4=one continuous ribbon. In this study, all patients included had an index score of 4 [3].
The parameters assessed post operatively were:
1) Visual analogue scale for analysis of the pain [25] This scale was used to analyze the pain from 0-10, 0 indicating no pain, 1-3 indicated mild pain, 4-7 indicated moderate pain and 8-10 indicated severe pain.
2) Landry’s wound healing index for the analysis of the wound healing at different stages [26] This index ranged from a score of 1 (very poor healing), 2 (poor healing), 3 (good healing), 4 (very good healing) and 5 (Excellent healing).
Preparation of the PRF membrane
The Choukroun’s Platelet-Rich Fibrin (PRF) is considered as a second generation platelet concentrate. This simple method was developed in France by Choukroun et al. [27,28], and is produced in a totally natural manner, without using anticoagulant during blood harvesting. The protocol is very simple and low cost: venous blood is collected in 10 ml dry tubes and centrifuged at about 400 g/3000 rpm for 10 min in the PRF centrifugation machine (Figure 1B). After centrifugation, three layers are formed in the tube: a base of red blood cells at the bottom, acellular plasma on the top (supernatant), and finally, a clot of PRF between them (Figure 1C). This clot of PRF is removed gently from the tube and placed on wet gauze; the attached red blood cells are cut off from this PRF. To make it a membrane, this PRF is gently squeezed between two gauze pieces till the desired thickness was achieved (Figure 1D) [27,28].
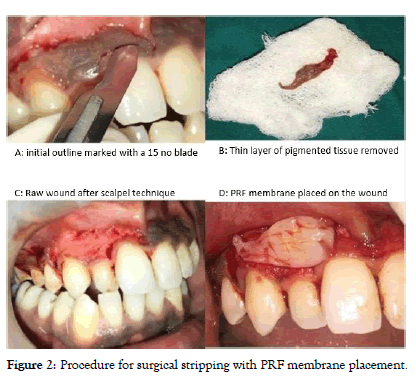
Figure 2: Procedure for surgical stripping with PRF membrane placement.
Surgical procedure for depigmentation
Scalpel technique/surgical stripping: In the scalpel technique, a 15 number blade was used to mark the outline of the pigmented regions after which a partial thickness incision was given to the desired depth and the complete epithelium and thin layer of connective tissue was removed in a uniform thickness leaving behind a raw area (Figure 2A-2C). Bleeding was encountered which had to be controlled otherwise visibility of deeper pigmentation would be hampered. Pressure pack with gauze soaked in local anesthesia was used to reduce the bleeding during the procedure. Once the bleeding was controlled, castroviejo scissors were used to trim the deeper tissues. Surgical stripping was performed on two sites out of which only one was covered with the PRF membrane as mentioned above (Figure 2D and 3A). Both the sites were covered with the coe-pak [29,30].
CO2laser: While using the CO2laser, 10,600 nm it is set at 2 W-4 W in a continuous wave mode (Figure 3B). This laser is used in non-contact mode where, initially a demarcation was made keeping the laser tip 1 cm away from the tissue to denote the region of pigmentation (focused mode), then the laser was held further away, around 3 cm (defocused mode) and the tissues within the denoted region were lased to induce a blister formation which was then peeled off (Figure 3C and 3D). The laser was always kept in continuous motion so that deeper structures were not damaged. If the beam was being brought near the tooth structure, then a pulsed mode was used to avoid damage to the hard tissues. The CO2laser is a complete hemostatic laser and leaves behind a raw surface and a bloodless field which makes the patients feels a slight itchy sensation.
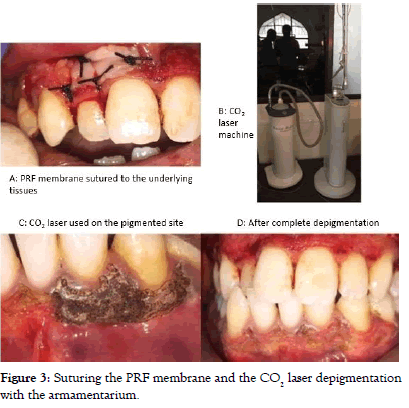
Figure 3: Suturing the PRF membrane and the CO2 laser depigmentation with the armamentarium.
As the CO2laser was used in two sites, one was covered with the PRF membrane and the other was not covered by the PRF membrane. The membrane was sutured to the underlying tissues with interrupted sutures (4-0). Both the sites were covered with coe-pak (Figure 4A).
The patients were called for follow ups on day 1, day 7, day 10 and day 14 (Figure 4 B and 4D).
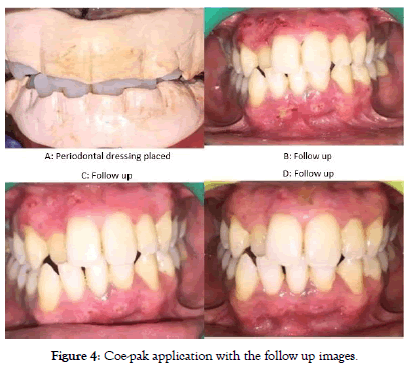
Figure 4: Coe-pak application with the follow up images.
Histological analysis
At 7th Day postoperative visit a section of tissue from the lateral incisor region of both arches was taken through punch biopsy from all the treated sites. Hematoxylin and eosin stained slides were prepared. At 40X magnification the tissues were observed under a light microscope (Figure 5A-5D).
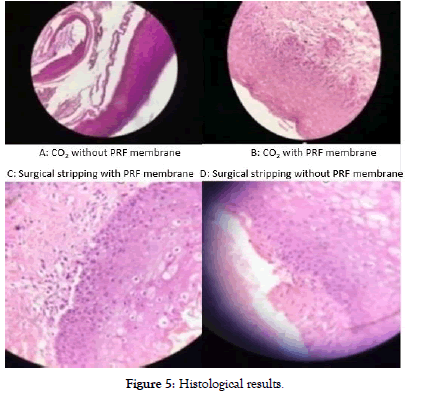
Figure 5: Histological results.
Statistics
The data was analyzed by an independent statistician using Statistical Packages for Social Sciences (SPSS) version 21.0. Frequency analysis in number and percentages were done. The power of the study was 80%, and a p<0.05 was considered statistically significant. The intergroup comparison of the variables was evaluated with Fisher’s exact test.
Results
Visual analogue scale was recorded for all four Groups at day 1, day 7 and day 10. The intragroup analysis was done and it was found that, In Group 1, according to Visual Analog Scale (VAS) there was no pain in 5 participants and mild pain in 5 participants at day 1. At day 7, it was found that there was no pain in 10 participants and similarly at day 10 there was no pain in 10 participants. This difference was statistically significant (p=0.005). In Group 2, according to VAS there was moderate pain in 10 participants at day 1. At day 7, it was found that there was mild pain in 10 participants and at day 10 there was no pain in 10 participants. This difference was statistically significant (p=0.000). In Group 3, according to VAS there was moderate pain in 10 participants at day 1. At day 7, it was found that there was mild pain in 10 participants and at day 10 there was no pain in 10 participants. This difference was statistically significant (p=0.000). In Group 4, according to VAS there was severe pain in 10 participants at day 1. At day 7, it was found that there was severe pain in 2 participants and moderate pain in 8 participants. At day 10 all 10 participants had moderate pain. This difference was statistically significant (p=0.000).
When VAS was compared between the groups on day 1, it was found that there was no pain and mild pain among 5 participants each in Group 1, moderate pain in 10 participants in Group 2, moderate pain in 10 participants in Group 3 and severe pain in 10 participants in Group 4. This difference was statistically significant (p<0.05). When VAS was compared between the groups on day 7, it was found that there was no pain among 10 participants in Group 1, mild pain in 10 participants in Group 2, mild pain in 10 participants in Group 3 and moderate and severe pain in 8 and 2 participants respectively in Group 4. This difference was statistically significant (p<0.05). When VAS was compared between the groups on day 10, it was found that there was no pain in all 10 participants in Group 1, Group 2 and Group 3. Whereas there was moderate pain in 10 participants in Group 4. This difference was statistically significant (p<0.05) (Graphs 1-3).
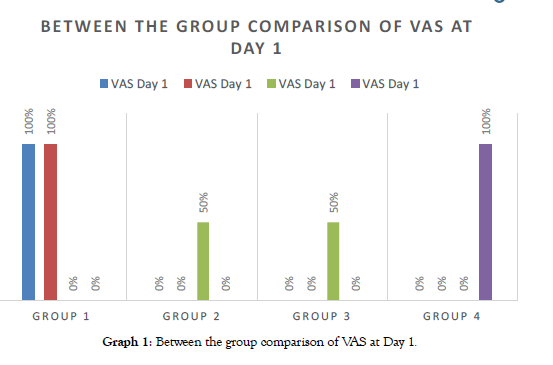
Graph 1: Between the group comparison of VAS at Day 1.
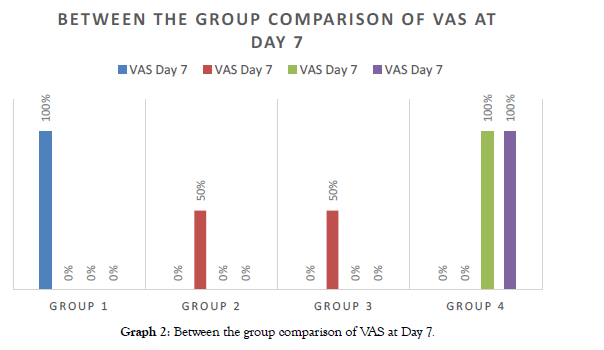
Graph 2: Between the group comparison of VAS at Day 7.
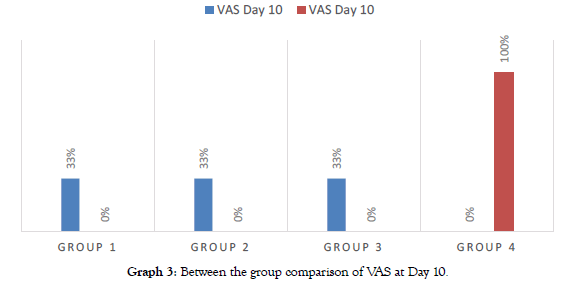
Graph 3: Between the group comparison of VAS at Day 10.
Landry’s wound healing index was assessed at day 1, day 7 and day 10. In Group 1, when Landry’s wound healing Index was assessed, healing was good in 2 participants and very good in 8 participants. At day 7, the healing was very good in 10 participants and at day 10, the healing was excellent for all 10 participants. This difference was statistically significant (p=0.000). In Group 2, when Landry’s wound healing index was assessed, healing was poor in 8 participants and good in 2 participants. At day 7, the healing was very good in 4 participants and very good in 6 participants.
At day 10, the healing was excellent for all 10 participants. This difference was statistically significant (p=0.000). In Group 3, when Landry’s wound healing index was assessed, healing was good in 8 participants and very good in 2 participants. At day 7, the healing was very good in 8 participants and good in 2 participants. At day 10, the healing was excellent for all 10 participants. This difference was statistically significant (p=0.000). In Group 4, when Landry’s wound healing index was assessed, healing was poor in 8 participants and good in 2 participants. At day 7, the healing was good in 10 participants and at day 10, the healing was excellent for all 10 participants. This difference was statistically significant (p=0.000).
When Landry’s wound healing index was compared between the groups on day 1, it was found that 8 participants each in Group 2 and Group 4 healing were poor. Healing was good in 2, 2, 8 and 2 participants in Group 1, Group 2, Group 3 and Group 4 respectively. Very good healing was seen in 8, 0, 2 and 0 participants in Group 1, Group 2, Group 3 and Group 4 respectively. This difference was statistically significant (p<0.05). When Landry’s wound healing index was compared between the groups on day 7, it was found that 0, 4, 2 and 10 participants in Group 1, Group 2, Group 3 and Group 4 respectively healing was good. Healing was very good in 10, 6, 8 and 0 participants in Group 1, Group 2, Group 3 and Group 4 respectively. This difference was statistically significant (p<0.05). When Landry’s wound healing index was compared between the groups on day 10, it was found that healing was excellent in all the 10 participants in each group i.e. Group 1, Group 2, Group 3 and Group 4.
From the above results it can be deciphered that Group 1 showed the best results in both VAS and Landry’s wound healing index followed by Group 2 and 3 with almost the same outcomes and then followed by Group 4 (Graphs 4-6).
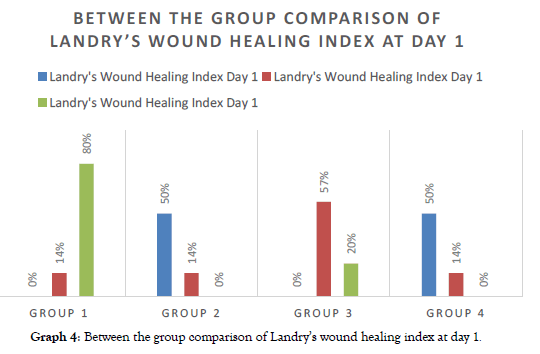
Graph 4: Between the group comparison of Landry’s wound healing index at day 1.
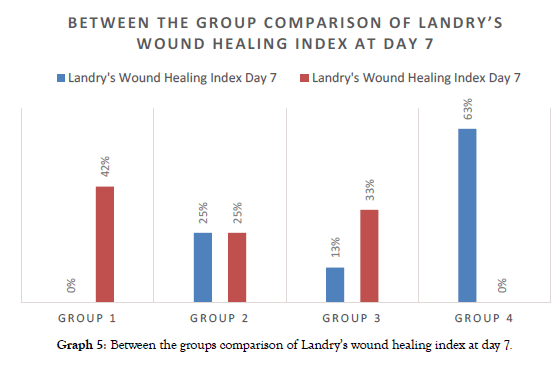
Graph 5: Between the groups comparison of Landry’s wound healing index at day 7.
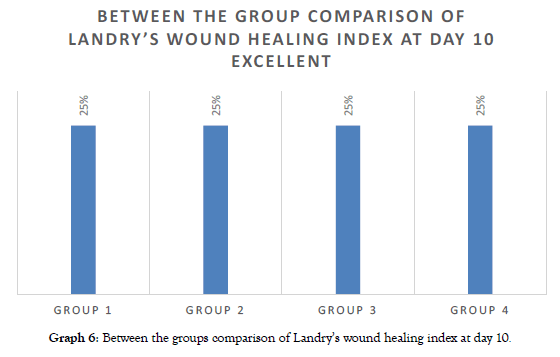
Graph 6: Between the groups comparison of Landry’s wound healing index at day 10.
Histological results
7 days after the procedure, a section of tissue was taken from the lateral incisor region of both the arches through a punch biopsy. Hematoxylin and eosin staining was performed and slides were prepared which were observed under 40x magnification. Comparing PRF and non-PRF sites, the PRFM sites had shown a distinct parakeratinized stratified squamous epithelium with moderate inflammatory cell infiltrate and the sites without Platelet- Rich Fibrin Matrix (PRFM) has severe inflammatory cell infiltrate. Therefore PRFM has shown to reduce the inflammatory.
Discussion
Depigmentation of the gingiva is routinely done for better aesthetics of the patient, and can be done by many techniques as mentioned above. Many of these procedures leave behind a raw wound which increases discomfort of the patient. The use of dental lasers have shown advantages such as a relatively bloodless field, the ability to cut, coagulate or vaporize the tissues, sterilization of the wound site, minimal swelling and scarring, lesser mechanical trauma as compared to surgical stripping, reduction of surgical time and with all of this obviously comes high patient acceptance.
The results of this study have shown that the group of CO2laser with PRF membrane as a biological dressing has shown better VAS scores and healing index as compared to the other groups. This can be mainly attributed to the fact that the laser used in this study was the CO2laser which is a completely hemostatic laser and caused a dry wound and a bloodless field of surgery. The only drawback seen with this type of a laser is that it delayed the process of wound healing as a dry wound takes longer to heal and left back an itchy sensation for the patient as soon as the anesthesia wore off. In some circumstances, if the laser beam was focused at one position for a longer duration than required, it may have led to damage of the deeper tissues and led to the formation of an ulcer. To overcome these issues, the PRF membrane was used to cover the sites and to provide faster healing of the dry wound. PRF membrane being obtained from the patient themselves had better tissue acceptability. The only disadvantage being that it created secondary wounds after the procedure of depigmentation as sutures had to be given to hold the membrane in its position.
By property, lasers have the ability to seal the blood vessels therefore reducing the bleeding during surgery. There is a yellowish white layer which is denatured protein coagulum which protects the wound that is formed a few hours after the procedure. Healing in laser depigmentation occurs by intermediate intention.
Depigmentation by surgical stripping creates a wound that heals by secondary intention. The procedure leaves a raw wound with multiple nerve endings that open up to the surface therefore creating increased pain perception. To avoid this raw surface, PRF membrane was used to cover the wound and provide decreased pain to the patient. In this study, surgical stripping with PRF membrane has shown better VAS scores as compared to surgical stripping without PRF membrane.
Many studies have been performed where coe-pak as a dressing has been used to cover the sites of depigmentation. But such dressings have no curative property and only protect the wound from mechanical trauma and therefore it provides the patient with comfort immediately after the surgery. In this study, all four groups were covered with coe-pak, so that the PRF membrane was held in position during the healing process. Coe-pak is dimensionally unstable which shows slight contraction after a few minutes of setting. This may lead to delayed wound healing. To overcome this, the use of PRF membrane as biological dressing been done in this study. As mentioned before the biologic effects of this PRF membrane are divided into 4 main aspects of healing. Fibrin is the natural guide for angiogenesis, which is the formation of new blood vessels inside the wound [21].
The property of angiogenesis of the fibrin matrix is explained by the 3 dimensional structures of the fibrin gel and by the simultaneous action of cytokines which are trapped inside the meshwork [22].
Angiogenesis soluble factors such as fibroblast growth factors, vascular endothelial growth factors, and platelet derived growth factors are present in the fibrin gel. Fibrin and the Fibrinogen Degradation Products (FDP) stimulate the migration of neutrophils and increase the membrane expression of CD 11c or CD 18 receptors. These factors help in the transmigration of the neutrophils [23]. The fibrin matrix serves as a guide to cover the injured tissues. Fibrin, fibronectin, Platelet-Derived Growth Factor (PDGF) and Transforming Growth Factor-Beta (TGF-β) are required to modulate fibroblast proliferation, and their migration into the wound [24].
When comparing VAS score and healing index for different studies where PRF membrane has been used as a biological dressing, Debnath K et al. [31], evaluated clinically and histologically the effect of PRF membrane and PRF matrix post the procedure of depigmentation done by abrasion method. The outcomes were that, the group with platelet concentrates had moderate pain and the group with only periodontal coe-pak had severe pain on the third day. This was in coordination with this study as the group with the PRF membrane had mild to moderate pain. They measured healing of the tissues using Landry’s healing index and stated that the groups with PRF and PRF membrane showed good healing, whereas the group with coe-pak showed poor healing. This too was in accordance to the present study. They concluded by stating that the application of PRF membrane and PRFM gel had shown a successful approach to protect the raw wound area of depigmented sites with better patient comfort and faster healing [31]. Another similar study conducted by Bansal M et al [32], was a split mouth study where PRF membrane was applied in the first quadrant and non-eugenol dressing (coe-pack) in the second quadrant. They evaluated the epithelialization with toluidine blue and it revealed that PRF treated sites stained less and therefore that meant there was better wound healing as compared to the coe pack sites. The assessed the VAS scores at three time intervals and noted that the patients with only coe-pak had slight pain whereas the sites with PRF had no pain. The same results were obtained in this study as the sites where PRF membrane was used, the patient acceptance was better and they had no pain. They measured healing of the tissues and stated that coe-pak sites had a greater erythematous area as compared to PRF which was similar to this study. Thus, they concluded by stating that PRF membrane as a periodontal dressing is a successful approach to protect the raw wound area of the depigmented site to reducing healing time and patient discomfort [32].
Numerous studies have been performed where any pack or biological dressing was not used to cover the depigmentation wound and have let the sites heal naturally being in direct contact with saliva. Saliva creates a humid environment that improves the survival and functioning of the inflammatory cells that are required for wound healing. It also contain secretory Ig A, growth factors such as Epidermal Growth Factors (EGF), Transforming Growth Factors (TGF) and vascular endothelial growth factors. Saliva also has several proteins that enhance wound healing by inhibiting the inflammatory response. Hegde R, et al. [14] conducted a study where 140 sites from 35 patients were considered and treated with surgical stripping, CO2laser and Er:YAG laser. The VAS scores for the three groups, were that, surgical stripping had the highest scores followed by CO2laser and then Er:YAG laser. This was in accordance to the present study where CO2laser has the least VAS scores (no pain) followed by surgical stripping having more values (severe pain). At one week postoperatively, all three groups showed a significant drop in VAS scores. The same was seen in the present study where the VAS scores dropped to no pain at the end of 10 days. Comparing with the present study, no micro ulcerations were seen as the PRF membrane had an added effect of serving as a biological membrane therefore aiding in the healing process [14]. Another study done by Basha MI, et al. [33] compared surgical stripping with Nd:YAG laser on 40 sites from 20 patients. Parameters such as plaque index, DOPI, Hedin melanin index, size of the pigmented area (statistically insignificant) and pain assessment (statistically significant) was taken. The mean VAS scores were 3.45 for Nd:YAG laser sites and 5.10 for surgical stripping sites. In the present study also, the VAS scores for the laser (CO2) group with PRF membrane was comparatively lower than the sites where surgical stripping was performed. There was less bleeding while using the Nd:YAG laser, than surgical stripping as it caused coagulation of blood vessels. The same findings can be seen in this study where, the CO2laser because of its complete hemostatic property led to the sealing of the blood vessels and therefore lesser bleeding during the procedure. They concluded by saying that Nd:YAG is a good alternative method for depigmentation but the surgical stripping remains the gold standard [33].
Emin Esen et al. [34], conducted a study in which the used the super pulsed mode of CO2for the procedure of depigmentation. Ablation of the hyperpigmented gingiva was accomplished with minimal carbonization and little or no bleeding. Post-operative healing was uneventful with less postoperative pain [34].
For the histological analysis, representative samples were taken from each group and after comparing PRF and non-PRF sites, the PRFM sites had shown a distinct parakeratinized stratified squamous epithelium with moderate inflammatory cell infiltrate and the sites without PRFM has severe inflammatory cell infiltrate. Therefore PRFM has shown to reduce the inflammatory component. This was in accordance to the studies done by Debnath K, et al. [31] and Bansal M, et al. [32] where no inflammatory cell infiltrates were seen in the group with PRF membrane and the groups with only a periodontal pack had severe chronic inflammatory infiltrates and the connective tissue was relatively fibrous [31,32].
Conclusion
Within the limitations of this study, it has been proven that, as 4 sites were evaluated in each patient in a split-mouth design, patient level bias and biological variation in wound healing were eliminated. Four groups were studied considering all possibilities of using and not using PRFM with CO2laser and surgical stripping. The use of PRFM for the procedure of depigmentation has been studied histologically along with the clinical parameters such as visual analogue scale and wound healing index following all four groups.
From the data obtained from the study, it can be concluded that CO2laser with PRFM has shown better results, clinically and histologically, as compared to the other groups. However, a study with a larger sample size and a longer follow up along with recurrence rate following the above techniques, would help in the evaluation of the success of all the procedures performed in the study.
Conflict of Interest
NoneFunding
None
REFERENCES
- Dummett CO, Barens G. Pigmentation of the oral tissues: A review of the literature. J Periodontol. 1967;38:369-378.
- Axeix T, Hedin CA. Epidemiologic study of excessive oral melanin pigmentation with special reference to the influence of tobacco habits. Eur J Oral Sci. 1982;90:434-442.
- Hedin CA. Smokers' melanosis: occurrence and localization in the attached gingiva. Arch Dermatol. 1977;113:1533-1538.
- Ozbayrak S, Dumlu A, Ercalik YS. Treatment of melanin-pigmented gingiva and oral mucosa by CO2laser. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:14-15.
- Coleton S. Lasers in surgical periodontics and oral medicine. Dent Clin N Am. 2004;48:937-962.
- Dummett sr CO. Clinical observations on pigment variations in healthy oral tissues of the Negro. J Dent Res. 1945;24:7-13.
- Bourquelot E, Bertrand G. Le bleuissement et le noircissement des champignons. Comp Rend Soc Biol. 1895;2:582-584.
- Lerner AB, Case JD. Part III: General considerations of skin pigmentation: pigment cell regulatory factors. J Invest Dermatol. 1959;32:211-221.
- Bishop K. Treatment of unsightly oral pigmentation: a case report. Dent Update. 1994;21:236-237.
- Almas K, Sadig W. Surgical treatment of melanin-pigmented gingiva; an esthetic approach. Indian J Dent Res. 2002;13:70.
- Gnanasekhar JD, Al-Duwairi YS. Electrosurgery in dentistry. Quintessence Int. 1998;29:649-654.
- Tal H, Landsberg J, Kozlovsky A. Cryosurgical depigmentation of the gingiva: A case report. J Clin Periodontol. 1987;14:614-617.
- Tal H, Oegiesser D, Tal M. Gingival depigmentation by erbium: YAG laser: clinical observations and patient responses. J Periodontol. 2003;74:1660-1667.
- Hegde R, Padhye A, Sumanth S, Jain AS, Thukral N. Comparison of surgical stripping; erbium‐doped: yttrium, aluminum, and garnet laser; and carbon dioxide laser techniques for gingival depigmentation: a clinical and histologic study. J Periodontol. 2013;84:738-748.
- Baghani Z, Kadkhodazadeh M. Periodontal dressing: a review article. J Dent Res Dent Clin Dent Prospects. 2013;7:183-191.
- Grover HS, Dadlani H, Bhardwaj A, Yadav A, Lal S. Evaluation of patient response and recurrence of pigmentation following gingival depigmentation using laser and scalpel technique: A clinical study. J Indian Soc Periodontol. 2014;18:586-592.
- http://blackwhiteimplants.weebly.com/uploads/5/4/5/4/5454101/prf_choukroun_overview_article.pdf.
- Dohan D, Donsimoni JM, Navarro G, Gaultier F. Platelet concentrates. Part 1: technologies. Implantodontie. 2003;12:5-16.
- Dohan D, Donsimoni JM, Navarro G, Gaultier F. Platelet concentrates. Part 2: associated biology. Implantodontie. 2003;12:17-25.
- Gaultier F, Navarro G, Donsimoni JM, Dohan D. Platelet concentrates. Part 3: clinical applications. Implantodontie. 2004;13:3-11.
- Dvorak HF, Harvey VS, Estrella P, Brown LF, McDonagh J, Dvorak AM. Fibrin containing gels induce angiogenesis. Implications for tumor stroma generation and wound healing. Lab Invest. 1987;57:673-686.
- van Hinsbergh VW, Collen A, Koolwijk P. Role of fibrin matrix in angiogenesis. Ann NY Acad Sci. 2001;936:426-437.
- Loike JD, Sodeik B, Cao L, Leucona S, Weitz JI, Detmers PA, et al. CD11c/CD18 on neutrophils recognizes a domain at the N terminus of the A alpha chain of fibrinogen. Proc Natl Acad Sci. 1991;88:1044-1048.
- Gray AJ, Bishop JE, Reeves JT, Laurent GJ. A alpha and B beta chains of fibrinogen stimulate proliferation of human fibroblasts. J Cell Sc. 1993;104:409-413.
- Krebs EE, Carey TS, Weinberger M. Accuracy of the pain numeric rating scale as a screening test in primary care. J Gen Intern Med. 2007;22:1453-1458.
- 26.https://openlibrary.org/works/OL11281110W/Effectiveness_of_benzydamine_HC1_in_the_treatment_of_periodontal_post-surgical_patients.
- Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-Rich Fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e37-e44.
- Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-Rich Fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e45-e50.
- Peters E, Gardner DG. A method of distinguishing between amalgam and graphite in tissue. Oral Surg Oral Med Oral Pathol. 1986;62:73-76.
- Chacko LN, Abraham S. Gingival melanin de-pigmentation for aesthetic correction. Case Reports. 2014;2014:bcr2014205711.
- Debnath K, Chatterjee A. Clinical and histological evaluation on application of platelet concentrates on depigmented gingival epithelium. J Indian Soc Periodontol. 2018;22:150-157.
- Bansal M, Kumar A, Puri K, Khatri M, Gupta G, Vij H. Clinical and histologic evaluation of platelet-rich fibrin accelerated epithelization of gingival wound. J Cutan Aesthet Surg. 2016;9:196-200.
- Basha MI, Hegde RV, Sumanth S, Sayyed S, Tiwari A, Muglikar S. Comparison of Nd:YAG laser and surgical stripping for treatment of gingival hyperpigmentation: A clinical trial. Photomed Laser Surg. 2015;33:424-436.
- Esen E, Haytac MC, Öz İA, Erdoğan Ö, Karsli ED. Gingival melanin pigmentation and its treatment with the CO2laser. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:522-527.
Citation: Ansari WN, Muglikar SD, Ghodke PS, Hegde RV, Sheikh S, Badaam H. Gingival Depigmentation Using CO2 Laser and Scalpel Technique with PRF Membrane-A Clinical and Histological Study . Dentistry 10: 563. doi: 10.35248/2161-1122.20.10.563
Copyright: © 2020 Ansari WN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

