Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
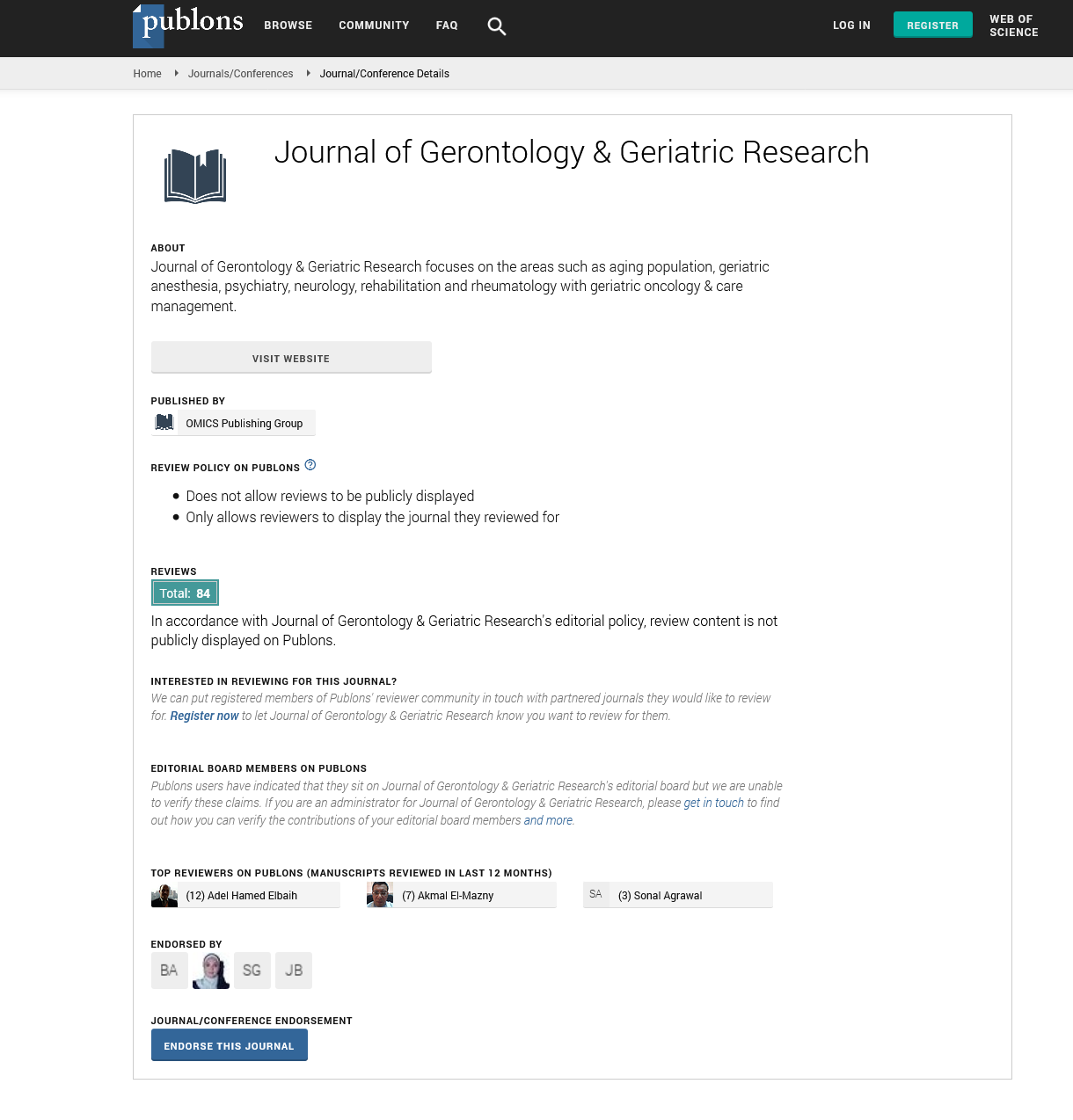
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Brief Report - (2023) Volume 12, Issue 3
Geriatric Syndromes: Diagnosis and Management
Rasinek Eskmik*Received: 01-Jun-2023, Manuscript No. jggr-23-22248; Editor assigned: 03-Jun-2023, Pre QC No. P-22248; Reviewed: 16-Jun-2023, QC No. Q-22248; Revised: 21-Jun-2023, Manuscript No. R-22248; Published: 28-Jun-2023, DOI: 10.35248/2167-7182.2023.12.678
Introduction
As the global population continues to age, geriatric syndromes have become an increasingly significant concern for healthcare professionals, caregivers, and policymakers. Geriatric syndromes are a collection of common clinical conditions that occur in older adults, which go beyond specific diseases and are typically characterized by their multifactorial nature. These syndromes often interact with one another, leading to complex presentations in older individuals. In this comprehensive review, we will delve into the diagnosis and management of some key geriatric syndromes, including falls, frailty, delirium, urinary incontinence, and pressure ulcers, with a focus on addressing their unique challenges and implementing effective strategies for optimizing care and improving the quality of life for older adults.
Description
Frailty is a state of increased vulnerability to stressors, leading to adverse health outcomes in older adults. It is a multidimensional syndrome characterized by reduced physiological reserves and functional decline. The diagnosis of frailty involves various tools, such as the Fried Frailty Criteria, the Clinical Frailty Scale, and the Rockwood Frailty Index, which help identify individuals at different levels of frailty. Managing frailty requires a holistic approach, addressing physical, psychological, and social aspects. Exercise interventions, particularly resistance training and balance exercises, have shown promise in improving physical function and reducing frailty. Nutritional support, including protein supplementation, can help counteract muscle loss and malnutrition. Additionally, addressing cognitive and emotional well-being through cognitive training and mental health support can contribute to better overall outcomes in frail older adults [1].
Delirium is an acute and fluctuating disturbance of consciousness and cognitive function, commonly affecting older adults during hospitalization or in long-term care settings. It is often precipitated by underlying medical conditions, medication use, and environmental factors. The diagnosis of delirium involves a thorough evaluation of cognitive function and behavior, along with the identification and management of potential trigger. Management of delirium centers on treating the underlying causes, minimizing environmental stressors, and optimizing supportive care. Non-pharmacological interventions, such as orientation techniques, sensory aids, and early mobilization, play a critical role in preventing and managing delirium. In cases where pharmacological management is necessary, low-dose antipsychotic medications can be considered for short-term use. However, the emphasis should always be on addressing the root causes and providing patient-centered care [2].
Urinary incontinence is a prevalent geriatric syndrome characterized by the involuntary loss of urine. It can significantly impact an older adult's quality of life, leading to social isolation and functional decline. To diagnose urinary incontinence effectively, a comprehensive assessment, including a medical history, physical examination, and voiding diary, is essential to identify the type and severity of incontinence.
The management of urinary incontinence involves a combination of behavioral, pharmacological, and surgical approaches. Behavioral interventions, such as bladder training, pelvic floor exercises, and fluid management, can be highly effective, particularly for stress and urge incontinence. Medications, such as anticholinergics and beta-3 agonists, may be prescribed in specific cases. For refractory cases or anatomical abnormalities, surgical interventions, such as sling procedures or artificial urinary sphincters, may be considered. A personalized approach tailored to the individual's needs and preferences is crucial for successful management`. Pressure ulcers, also known as bedsores, are localized injuries to the skin and underlying tissue, primarily caused by prolonged pressure on bony prominences. Older adults are particularly susceptible to pressure ulcers due to reduced mobility, decreased tissue tolerance, and comorbidities. Proper diagnosis involves a thorough assessment of the wound's size, depth, and characteristics [3].
As the global population continues to age, it is imperative that healthcare systems prioritize palliative care services for older patients. Adequate training and education should be provided to healthcare professionals to enhance their skills in delivering palliative care to the elderly population. Additionally, interdisciplinary collaboration among healthcare providers is crucial to ensure comprehensive and coordinated care Moreover, public awareness and education about palliative care and its benefits for geriatric patients need to be increased. Addressing misconceptions and stigmas associated with palliative care can encourage earlier utilization of services and better patient outcomes. The prevention of pressure ulcers is paramount and involves a proactive approach, including regular skin assessments, frequent repositioning, the use of support surfaces, and optimizing nutrition and hydration. For existing pressure ulcers, wound care management, including proper cleansing, debridement, and dressings, is necessary for healing and prevention of infection. Multidisciplinary teams, involving nurses, physicians, nutritionists, and physical therapists, must collaborate to provide comprehensive care to prevent and treat pressure ulcers effectively [4,5].
Conclusion
Geriatric syndromes pose significant challenges to the aging population and healthcare systems worldwide. To effectively address these syndromes, a comprehensive and interdisciplinary approach is crucial, encompassing early diagnosis, prevention, and tailored management strategies. Healthcare providers must stay informed about the latest evidence-based practices and continually adapt their approaches to meet the evolving needs of older adults. By prioritizing proactive and patient-centred care, we can improve the overall health and well-being of the aging population and foster a society that values and supports the unique needs of its elderly members.
Acknowledgement
None.
Conflict of Interest
None.
References
- Wang Y, Tang B, Long L, Luo P, Xiang W, Li X, et al. Improvement of obesity-associated disorders by a small-molecule drug targeting mitochondria of adipose tissue macrophages. Nat Commun 2021; 12:102.
- Pfleger J, He M, Abdellatif M. Mitochondrial complex II is a source of the reserve respiratory capacity that is regulated by metabolic sensors and promotes cell survival. Cell Death Dis 2015; 6: 1835-.
- Heidorn-Czarna M, Heidorn HM, Fernando S, Sanislav O, Jarmuszkiewicz W, Mutzel R, et al. Chronic activation of AMPK induces mitochondrial biogenesis through differential phosphorylation and abundance of mitochondrial proteins in dictyostelium discoideum. Int J Mol Sci 2021;22:11675.
- Brandauer J, Andersen MA, Kellezi H, Risis S, Frøsig C, Vienberg SG, et al. AMP-activated protein kinase controls exercise training-and AICAR-induced increases in SIRT3 and MnSOD. Front Physiol 2015;6:85.
- Mohammadi M, Gozashti MH, Aghadavood M, Mehdizadeh MR, Hayatbakhsh MM. Clinical significance of serum IL-6 and TNF-α levels in patients with metabolic syndrome. Rep Biochem Mol Biol 2017; 6:74.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Eskmik R (2023) Geriatric Syndromes: Diagnosis and Management. J Gerontol Geriatr Res. 12: 678.
Copyright: © 2023 Eskmik R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.