Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
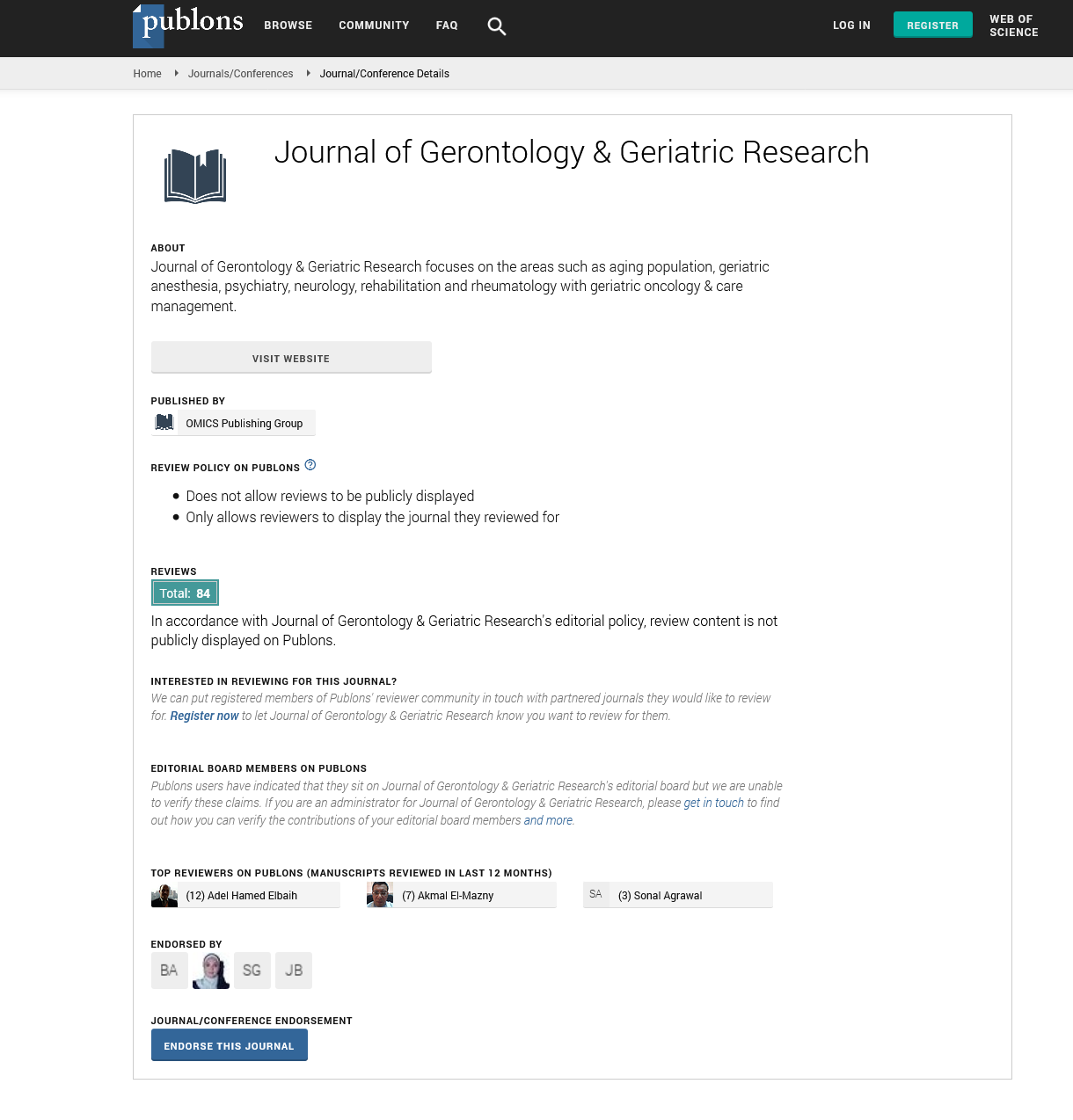
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary Article - (2023) Volume 12, Issue 3
Geriatric Pharmacotherapy: Optimal Medication Use
Kercia Srenni*Received: 01-Jun-2023, Manuscript No. jggr-23-22245; Editor assigned: 03-Jun-2023, Pre QC No. P-22245; Reviewed: 16-Jun-2023, QC No. Q-22245; Revised: 21-Jun-2023, Manuscript No. R-22245; Published: 28-Jun-2023, DOI: 10.35248/2167-7182.2023.12.675
Description
Geriatric pharmacotherapy refers to the branch of medicine that focuses on the use of medications in older adults. As people age, their bodies undergo various physiological changes that can affect the way drugs are metabolized and their overall response to treatment. Optimal medication use in the geriatric population is crucial to ensure safety, effectiveness, and improved quality of life. This article explores the challenges and considerations involved in geriatric pharmacotherapy and highlights strategies for optimizing medication use in older adults.
With advancing age, several physiological changes occur in the body that can influence the pharmacokinetics of These changes include a decline in renal function, reduced hepatic metabolism, altered gastrointestinal absorption, and changes in body composition. These age-related changes can lead to prolonged drug half-life, increased drug accumulation, and a higher risk of adverse drug reactions. Therefore, it is essential to consider these changes when prescribing medications to older adults and adjust the dosage accordingly [1,2].
Polypharmacy, defined as the concurrent use of multiple medications, is a common concern in the geriatric population. Older adults often have multiple chronic conditions that require multiple medications, leading to an increased risk of drug interactions, adverse effects, and medication non-adherence. Polypharmacy can also contribute to cognitive impairment and functional decline. Healthcare providers need to carefully evaluate the risks and benefits of each medication and prioritize the most essential treatments. Regular medication reviews and communication among healthcare providers are vital in identifying and resolving drug-related problems in older adults.
The Beers Criteria is a widely recognized tool developed by the American Geriatrics Society (AGS) to identify potentially inappropriate medications in older adults. It provides a list of medications that should be avoided or used with caution in the geriatric population due to their potential for harm or lack of effectiveness. The Beers Criteria is regularly updated to incorporate new evidence and is an essential resource for healthcare providers when prescribing medications to older adults. Adhering to the Beers Criteria helps minimize the risk of adverse drug events and improve patient outcomes. Sleep disturbances, such as insomnia and sleep pane, are common in individuals with mental health disorders, including depression, anxiety, and bipolar disorder. Conversely, chronic sleep deprivation or poor sleep quality can contribute to the development or exacerbation of mental health issues. Adequate and restorative sleep is vital for emotional regulation, mood stability, and overall mental well-being across all age.
DE prescribing is the process of reducing or stopping medications that are no longer necessary, have limited benefits, or pose potential harm to the patient. It is an important strategy in geriatric pharmacotherapy to optimize medication use. Many older adults are prescribed medications that may have been necessary in the past but are no longer needed or may even be contributing to their health issues. Deprescribing requires a thorough assessment of the patient's medical history, reviewing current medications, and considering the patient's goals of care. Shared decision-making between the healthcare provider and the patient is crucial in deprescribing to ensure patient satisfaction and adherence to the medication plan. Medication adherence is a significant challenge in geriatric pharmacotherapy. Older adults may face various barriers to adherence, including cognitive decline, physical limitations, medication complexity, and financial constraints. Healthcare providers can promote adherence by simplifying medication regimens, providing clear instructions, and addressing potential barriers. The use of adherence aids such as pill organizers, reminder apps, and family involvement can also support medication adherence in older adults. Regular follow-ups and medication reviews are important to assess adherence and address any issues that may arise [3-5].
Geriatric pharmacotherapy plays a vital role in promoting optimal medication use in older adults. Understanding the physiological changes associated with aging, considering the principles of polypharmacy, and adhering to tools like the Beers Criteria are essential in ensuring medication safety and efficacy. Deprescribing, medication adherence strategies, and addressing special considerations like cognitive impairment and renal function are crucial in optimizing geriatric pharmacotherapy. By incorporating these strategies into clinical practice, healthcare providers can improve medication outcomes, minimize adverse drug events, and enhance the overall well-being of older adults. Sensory Changes: Older adults may experience sensory changes, such as visual and hearing impairments, which can affect their ability to read labels or understand verbal instructions. Healthcare providers should consider these sensory changes when communicating medication information and provide appropriate aids if needed.
Acknowledgement
None.
Conflict of Interest
None.
References
- Baysal BE, Maher ER. 15 YEARS OF PARAGANGLIOMA: Genetics and mechanism of pheochromocytoma–paraganglioma syndromes characterized by germline SDHB and SDHD mutations. Endocr Relat Cancer 2015; 22:T71-82.
- Benn DE, Gimenez-Roqueplo AP, Reilly JR, Bertherat J, Burgess J, Byth K, et al. Clinical presentation and penetrance of pheochromocytoma/paraganglioma syndromes. J Clin Endocrinol Metab 2006; 91:827-836.
- Mannelli M, Castellano M, Schiavi F, Filetti S, Giacchè M, Mori L, et al. Clinically guided genetic screening in a large cohort of Italian patients with pheochromocytomas and/or functional or nonfunctional paragangliomas. J Clin Endocrinol Metab 2009; 94:1541-1547.
- Anttila T, Häyry V, Nicoli T, Hagström J, Aittomäki K, Vikatmaa P, et al. A two-decade experience of head and neck paragangliomas in a whole population-based single centre cohort. Eur Arch Oto-Rhino-Laryngology 2015; 272:2045-2053.
- Wojtovich AP, Smith CO, Haynes CM, Nehrke KW, Brookes PS. Physiological consequences of complex II inhibition for aging, disease, and the mKATP channel. Biochim Biophys Acta (BBA)-Bioenerg2013; 1827:598-611.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Srenni K (2023) Geriatric Pharmacotherapy: Optimal Medication Use. J Gerontol Geriatr Res.12: 675.
Copyright: © 2023 Srenni K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.