Indexed In
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Access to Global Online Research in Agriculture (AGORA)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- SWB online catalog
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review - (2020) Volume 11, Issue 7
Foodborne Pathogens Dilemma in the Mediterranean Diet: Case of Lebanon
Caline Harb*, Emilio Mouannes, Marc Bou Zeidan, Afif M Abdel Nour and Lara Hanna-WakimReceived: 01-Jun-2020 Published: 06-Jul-2020, DOI: 10.35248/2157-7110.20.11.832
Abstract
Mediterranean food has been known for its positive health impact however, a huge concern regarding its safety still remains.
We reviewed the literature on food safety and foodborne illnesses particularly those caused by bacteria over the past 20 years in Lebanon.
Food safety practice has major gaps in Lebanon where several food types of dairy products, meat, poultry, vegetables, and water have been reported to be contaminated by Brucella species, Campylobacter jejuni, Escherichia coli, Listeria monocytogenes, Salmonella species, Staphylococcus aureus, and Yersinia species. Furthermore, the majority of these reported bacterial foodborne infections have shown resistance to several antibiotics.
Food safety practice needs substantial efforts from public and private sector to protect consumers and help maintain a decent socio-economic status. This can only be implemented by new laws regulating the food chain, from farm to fork. Consumers as well need to become more aware about good food hygiene practices.
Keywords
Food safety; Foodborne bacteria; Mediterranean food; Lebanon
Introduction
Food safety is a major global public health concern and also a basic human right [1]. Foodborne Illness (FI) is the result of consuming contaminated food that leads to an infection. It is mainly due to food contamination by bacteria, viruses, and parasites [2] that can occur at any point along the food chain during production, processing, distribution, or preparation. Common symptoms of FI are diarrhoea, vomiting, abdominal cramps, bloating, fever, reactive arthritis, and headache. The development of these signs and symptoms can occur between few hours and 1-8 days after the exposure to the pathogen [3]. Although foodborne illnesses may affect anyone, vulnerable people are more likely to endure severe food poisoning which may lead to hospitalization or even death [2]. That is why, it is essential to apply the 5 keys to safer food, set by the World Health Organization (WHO) [4].
The aim of this review was therefore to gather several research studies related to the microbiological quality of the Mediterranean food in order to evaluate the food safety situation in this region.
The Impact of Foodborne Illnesses on Human Health
Foodborne diseases have been a problematic health and economic hazard for all communities. However, there is a continuously changing trend in the types, severity and impacts of these diseases through the ages across regions and communities. Yet, surveillance challenges are considered to be common to all countries where only some people who get foodborne diseases do seek medical care. Furthermore, less numbers are reported to public health officers and recorded in official illness epidemiology as food poisoning cases [5].
According to the WHO in the Eastern Mediterranean Region, foodborne illnesses have reached an estimate of 100 million cases causing 37,000 mortalities. Diarrheal diseases are responsible for 70% of this burden. Particularly, 32 million children, aged below five, are suffering from foodborne illnesses [6]. Because of the severity of the impact of the FI, food safety has become necessary to protect consumer health.
Food Safety in Arab Countries
Microbial food safety persists as a major economic and public health concern. Foodborne illnesses not only impact consumers’ health but also the economy of exporting countries where any microbiological or chemical proven food contamination can result in rejection of exported goods and economic loss. In 2003, a 27% of rejection rate was reported from several Arab countries (Egypt, Jordan, Lebanon, and Syria) by the United States Food and Drug Administration due to the lack of efficient food safety programs [7]. This issue is multifactorial; Rolle (2006) indicated the lack of sufficient resources, proper transportation, infrastructure, and handling. This multi-level gap as well as the irregular electrical power supply increase the losses of food that need proper storage condition such as fish and milk during transportation. As consequence of the above, the importation or distribution of the products gets rejection or destroyed after testing [8].
Over the past several years many Arab countries have tried revising and upgrading food quality control and surveillance programs; however, variable program scope and effectiveness were reported [1]. The underreporting of foodborne diseases and the underestimation of seriousness of these health threats in Arab countries is due to the ineffective implementation of proper hygienic policies and the inaccurate surveillance systems (Jordan, Lebanon, Libya, Oman, Saudi Arabia, and Somalia) [7]. Also, the consumption of raw products’ (meat, milk, and salads), unpasteurized dairy products and the change in food habits and lifestyle, in Arab countries, have resulted in increased exposure to contaminated food, thus increased the impact of health hazard [7,9,10]. Unfortunately, due to the lack of accurate data in Arab countries, the incidence of foodborne illnesses remains not determined [7].
Food Safety in Lebanon
Lebanese traditional diet
The Lebanese traditional diet is a cultural heritage and has always been perceived as a healthy and balanced eating pattern. This heritage goes back to the historical mix of the following cultures: Babylonians, Phoenicians, Egyptians, Greeks, Romans, Persians, Byzantines, and Turks [11]. The components of this diet have a positive health impact where it includes considerable amount of plant based food: cereals, fruits, vegetables, potatoes, legumes, nuts and seeds. Also, the Lebanese desserts include minimally processed fresh fruit and olive oil as the principle source of fat. Added to the above, dairy products are also considered huge heritage where they are several products still processed through traditional and home-based methods. As for animal-based food: fish, poultry and red meat also constitute a major ingredient in the daily Lebanese dishes. These ingredients all reflect the Mediterranean Middle Eastern diet that has a positive influence on the consumers’ wellbeing [11].
Food safety laws and regulations
One of the major concerns in food safety in Lebanon is that the Ministry of Public Health is still following out-dated decrees and regulations [12]. These regulations do not follow evidence based literature and need extensive work and research to be able to improve local practices of food safety. This concern is further complicated by the presence of several food related agencies, since there is sometimes overlap in duties and poor coordination among the ministries dealing with food safety issues. It is also confusing for consumers and industries for their exact roles [12].
Another crucial issue is that several food industries do not apply food safety practices where Food Inspection and Compliance Monitoring System’s effectiveness and function are still absent [13]. Though several trials to implement food safety law for the past 13 years and several contamination scandals have reached public awareness. Instead of reporting practices and emphasizing the proper handling and production of food, the Ministry of Public Health has published a list of restaurants, supermarkets and other food provider services that did not meet the food regulation standards set by the ministry. Furthermore, it was also reported an estimate of 1926 cases of food and waterborne illnesses (Ministry of Public Health 2010), the presence of spoiled/expired food, the use of prohibited preservatives (Natamycin) in "Labneh" (dairy product) and the presence of infectious pathogenic (Escherichia coli, Salmonella spp., Staphylococcus aureus, and Listeria monocytogenes) in levels exceeding international standards of safety [12]. Therefore, the reported misconduct of food safety in the Lebanese practice has marvellously affected the local community’s trust as well as the exporting market. This distrust resulted in a local approach to prefer imported food products.
Consumer awareness and perception of food safety
The modern daily lifestyle has led to increased fast food consumption. This trend has been reflected by the large distribution of fast food restaurants and street vendors among all community areas [14]. Thus increasing further exposure to diseases due to the hazardous food. In Lebanon, consumer awareness about food safety practice was studied [14]. The findings have highlighted several gaps at the consumer level regarding food safety knowledge and practices of significant differences among education levels. Further consumers’ confusion about basic food safety is reported by another study conducted by Jaroudi [15]. This proves that the Lebanese population do not have enough awareness about certain safety issues, hence they are alarmed by the word "bacteria". However, people may only become concerned about risks if they have associated these with a prior negative experience. Hassan and Dimassi [16] reported an estimate of 54 ± 16% and 45 ± 14% on food safety knowledge and food handling, respectively among 1172 Lebanese university students who answered their questionnaire. These results confirm the need for continuous educational approaches to improve little food awareness among Lebanese young adults groups.
Faour-Klingbeil et al. through a survey study on 80 food handlers in 50 food service establishments, showed substantial gaps in food safety knowledge and practices associated with critical temperature of foods and cross contamination. These findings further verify the seriousness of the imposed health risks on the consumer. Other findings have shown a significant higher awareness among food handlers in corporate managed food outlets. Thus, the managerial element is an integral part to influence food safety practices among food handlers. The authors recommend a synergistic participation of both private and public sector in food safety educational intervention and technical guidance are needed [17].
Bou-Mitri et al. found that food handlers in Lebanese hospitals have scored 59.2%, 83.7% and 83.2% on the knowledge, attitudes and practices questions, respectively and 75.4% on the overall Knowledge, Attitude, Practice (KAP) score. The authors highlighted the need for on-going food safety measures, practice sessions and hygiene policies to improve food handlers’ knowledge and thus food safety in hospitals [18].
Hassan et al. found out that the average scores for the Lebanese food handlers in households were respectively 55.6%, 51.3%, 67.4% and 89.1% on food handling, storage, usage of kitchen facilities and personal hygiene while the passing rates were 64.5%, 69.9%, 90.5% and 99.1% respectively. However, several significant factors (gender, area of residence, income status) were identified. The authors highlights the gap in the food safety knowledge and the need for continuing educational plan to improve practice among Lebanese food handlers in Lebanese households [19].
Abebe et al. went from the micro-level of food handlers to the governance mechanisms-Governance Structures (GSs) and Food Safety Management Systems (FSMSs), suggesting that, the implementation of the prior food safety is influenced by formality of the contract, herd size, trading partner choice, and experience. They also recommend empowering farmers by introducing incentives and facilitating loans and education [20].
Major Food Poisoning Bacteria
The most commonly incriminated bacteria in foodborne illnesses are: Brucella species, Campylobacter jejuni, Escherichia coli, Listeria monocytogenes, Salmonella species, Staphylococcus aureus, and Yersinia species. Table 1 includes these different organisms along with the major food sources linked to these bacterial infections. Each species of bacteria has different method of transmission, sources, and incubation period in different food types [21]. Relevant articles dealing with food safety in Lebanon were sorted according to the following food categories: dairy products (Table 2), meat products (Table 3), and fruits and vegetables, and other food products (Table 4).
| Organism | Associated foods |
|---|---|
| Brucella spp. Small, Gram-negative, short, non-sporeforming coccobacillus | Exposure usually through veterinarian occupation or ingestion of raw animal products |
| Campylobacter jejuni Non-sporeforming, Gram-negative rod with a curved- to S-shaped morphology | Raw and undercooked poultry, unpasteurized milk, contaminated water |
| Escherichia coli Highly motile, Gram-negative, rod-shaped bacteria | Enterotoxigenic E. coli (ETEC): Water or food contaminated with human feces |
| Listeria monocytogenes Gram-positive, rod-shaped, facultative bacterium, motile by means of flagella | Inadequately pasteurized milk and dairy products, raw meat |
| Salmonella spp. Motile, non-sporeforming, Gram-negative, rod-shaped bacterium | Contaminated eggs, meats, poultry, unpasteurized milk or juice, contaminated raw fruits and vegetables, spices, chocolate |
| Staphylococcus aureus Gram-positive, non-motile, catalase-positive, small, spherical bacteria (cocci) | Unrefrigerated or improperly refrigerated meats, potato and egg salads, cream pastries |
| Yersinia enterocolytica Small, rod-shaped, Gram-negative bacteria. | Meat, undercooked pork, unpasteurized milk, contaminated water |
Table 1: Foods associated with organisms.
| Food type | Author | Pathogen | Major findings |
|---|---|---|---|
| Darfiyeh cheese | Serhan et al. [22] | Bacilli | Contamination by Lactococcus lactis subsp. lactis, L. lactis subsp. cremoris, Lactobacillus plantarum, Lactobacillus curvatus |
| Raw cheese | Al-Shaar et al. [23] | Brucella | Consumption of raw cheese is a significant brucellosis risk factor |
| Kishk, Shankleesh and Baladi cheese | Alwan et al. [24] | Brucella | High number of antimicrobial resistance (n=4 out of 6 for Streptomycin and Ciprofloxacin; n=3 out of 6 for Gentamicin) |
| Kishk and Baladi cheese | Gilbert et al. [25] | Escherichia coli | 14.4% Kishk and 66.4% Baladi unfit for human consumption |
| Kishk, Shankleesh and Baladi cheese | Saleh et al. [10] | Escherichia coli |
|
|
|||
| Qishta | Kassaify et al. [26] | Escherichia coli | 32% of the selected samples contaminated by E. coli |
| Darfiyeh cheese | Serhan et al. [22] | Escherichia coli | E. coli detected with a variable inconsistent percentage of colonization within the samples, beyond the accepted national microbiological standards |
| Serhan and Mattar [27] | |||
| Qishta | Kassaify et al. [26] | Listeria monocytogenes | 42% of selected samples contaminated by Listeria monocytogenes |
| Kishk, Shankleesh and Baladi cheese | Harakeh et al. [28] | Listeria monocytogenes |
|
|
|||
| Goat milk cheeses (Darfiyeh, Aricheh, Shankleesh and Serdale) | Serhan and Mattar [27] | Staphylococcus aureus | Most of these samples contaminated by S. aureus beyond their accepted national microbiological levels |
| Kishk, Shankleesh and Baladi cheese | Zouhairi et al. [29] | Staphylococcus aureus |
|
|
|||
| Kishk, Shankleesh and Baladi cheese | Harakeh et al. [30] | Yersinia | High rates of resistance to used antimicrobials, highest resistance to kanamycin (81.2%) and streptomycin (87.5%) |
| Dairy products | Loukieh et al. [31] | Escherichia coli | 60% of dairy products were contaminated |
| Listeria spp. | |||
| Salmonella spp. | |||
| Staphylococcus aureus |
Table 2: Dairy products.
| Food type | Author | Pathogen | Major findings |
|---|---|---|---|
| Poultry | El-Rami et al. [32] | Escherichia coli | Predominance of E. coli isolates in poultry along with significant resistance to tetracycline and gentamicin |
| Lahm-bi-Ajeen and Shawarma | Harakeh et al. [33] | Escherichia coli |
|
|
|||
| Chicken noodles | Hanna et al. [34] | Salmonella | Hospitalization due to severe gastroenteritis |
| Lahm-bi-Ajeen and Shawarma | Harakeh et al. [33] | Salmonella |
|
|
|||
| Meat products | Loukieh et al. [31] | Escherichia coli | 45% of meat products were contaminated |
| Listeria spp. | |||
| Salmonella spp. | |||
| Staphylococcus aureus |
Table 3: Meat products.
| Food type | Author | Pathogen | Major findings |
|---|---|---|---|
| Fresh vegetables | Faour-Klingbeil et al. [35] | Escherichia coli | Fresh vegetables contained STEC and E. coli strains found to be multi-drug resistant (60%) |
| Food products | Haidar-Ahmad et al. [36] | Listeria monocytogenes |
|
|
|||
| Fresh vegetables | Faour-Klingbeil et al. [37] | Listeria monocytogenes | Listeria spp. levels statistically significant with cross-contamination and cleaning components |
| Tahini (sesame and seed products) | Unicomb et al. [38] | Salmonella |
|
|
|||
| Hummus (nuts and seeds) | Crowe et al. [39] | Salmonella | 23 illnesses in multistate Salmonella outbreak due to Lebanese imported Hummus |
| Fresh vegetables | Faour-Klingbeil et al. [37] | Staphylococcus aureus | Staphylococcus aureus was detected in 45.5% of fresh produce and Salmonella spp. in 6.7% of the raw vegetables |
| Fruits and vegetables | Loukieh et al. [31] | Escherichia coli | 60% of fruits and vegetables products were contaminated |
| Listeria spp. | |||
| Salmonella spp. | |||
| Staphylococcus aureus |
Table 4: Fruits and vegetables and other food products.
Brucella spp., is a Gram-negative, non-spore-forming coccobacillus, causing the Brucellosis. The latter is commonly transmitted from animals to human [21]. Several studies testing the food contaminated by Brucella were conducted in Lebanon. Since the early 1990s, Araj and Azzam showed that there was a high exposure to brucellosis among butchers, farmers, laboratory technicians, abattoir workers and veterinarians in high-risk occupations [40]. After the brucellosis infection outbreak that invaded Chouf district of Lebanon in 2009, Al-Shaar, Chaaya, Ghosn, and Mahfoud, conducted a study showing poor knowledge and furthermore misconceptions about human-human transmission. The major findings were presented in Table 2. In addition, the authors recommended educating people on proper food preparation by both correct ways of milk pasteurization and handling meat products, and elevating food safety monitoring threshold. Also, animal vaccination was cornerstone as prevention strategy so there are no further animal-human transmissions [23]. As shown in Table 2, Alwan et al. had isolated Brucella species from raw Lebanese dairy-based food products and reported a high number of antimicrobial resistances. Thus, the authors emphasized on the need for incorporating proper hygienic standards and proper antibiotic use to be able to limit Brucella contamination and their resistance level in the environment [24]. Campylobacter jejuni, is a non-spore-forming, Gram-negative rod, with a flagellum at one or both of the polar ends of this bacterium for function of motility. In order to avoid this bacterial infection, a proper handling and cooking of raw food is crucial [21]. Dabboussi et al. studied the prevalence of Campylobacter in childhood diarrhoea in North Lebanon and reported through PCR the huge infectious reason due to Campylobacter species (11.1%). The studied population was children (1 month to 10 years) admitted for diarrhoea to five hospitals in North Lebanon. The findings are serious hazard especially that it is affecting the early ages to be admitted to the hospital [41].
Escherichia coli (E. coli), a Gram-negative, rod-shaped bacteria, is predominantly present as normal intestinal flora in the humans. However, this bacterium may exist as pathogenic groups [21].
In fact, in Lebanon, Loukieh et al. reported that different food products showed, as indicated in Tables 2-4, unsatisfactory levels of foodborne pathogens. Particularly, 20% of fruits and vegetables and dairy products were respectively infected with E. coli. These results correlate with inappropriate hygiene practice, hand washing, food preparation, refrigeration, storage conditions, and lack of clean water [31].
Because enteric infections are considered a leading cause of pediatric morbidity and mortality particularly in the developing regions, Hamze et al. have conducted a study investigating the antibiotic susceptibility of several pathogens including Enteropathogenic Escherichia coli (EPEC) isolated from hospitalized diarrheic children (n=172) in North Lebanon over a period of 7 years. Bacterial contamination rates were illustrated in Figure 1. Furthermore, this study revealed a relatively high antibiotic resistance rate 50% to ampicillin and 25% to extended-spectrum cephalosporin, of EPEC, Shigella spp. and Non-Typhoid Salmonella isolates among the studied population. These findings reflect the need to develop effective health.
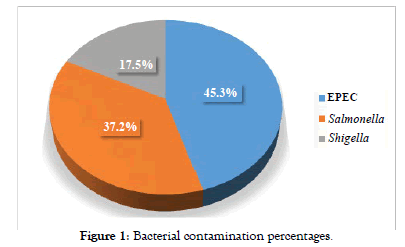
Figure 1: Bacterial contamination percentages.
Extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBLPE) has not been only reported in hospitalized children but was also shown by Hijazi et al. to reach a prevalence of 24.8% (31 of 125) in healthy children aged from 1 to 5 years old. The study was conducted by using combination-disc method test and multiplex PCR, showing a significant association between ESBL-PE and consumption of meat, chicken, but not with dairy products. Furthermore, bathroom hygiene habits were found also to be affecting the carriage rate. These findings show the drastic need to perform further investigations evaluating and routinely screening ESBLPE carriage with various food consumption, and the high antimicrobial resistance profile highlights the need to implement proper antibiotic use especially among paediatrics [43].
Food contaminated with pathogens is a major concern when the pathogens acquire the characteristic of drug resistance. This emergence has been correlated to the excessive uncontrolled antibiotic use for both human and veterinary medicine especially in Lebanon [44]. Resistant bacteria may colonize the environment (soil, sewage, and surface water), food, and the intestinal tracts of humans or animals [45]. In fact, E. coli is known to develop drug resistance in several ways through the production of β-lactamase and the exchanging of plasmids [46,47]. That is why studying the antimicrobial resistance methodologies is important in both clinical and environmental isolates to be able to limit the outbreak of multidrugresistant bacterial strains, [48] and E. coli has been studied in several food products in Lebanon (dairy products, meat and poultry, and vegetables).
Saleh et al. studied the presence of E. coli and their strains in three dairy products in the Beqaa Valley by using McConkey and sorbitol-McConkey agar and PCR-based assays [10]. The findings presented in Table 2 show that some popular dairy products pose a public-health hazard; contributing to the transmission of drug-resistant pathogens. In terms of microbiological quality, according to Gilbert et al. (Table 2), the Kishk appeared to be the best of the dairy products [25]. Qishta, another dairy product, studied by Kassaify et al. has been reported to be contaminated by E. coli (Table 2). In fact, Qishta is prepared using a traditional heating and skimming process, it is considered to have high counts of spoilage and threat to the community [26].
As shown in Table 2, E. coli was also detected in Darfiyeh cheese. This is in concordance with the high prevalence of diseases associated with the consumption of raw goat milk cheeses [22,27].
Other than dairy products, poultry and meat based food were reported to be contaminated by E. coli. As shown in Table 3, El-Rami et al. reported the predominance of E. coli isolates in poultry [32]. Harakeh et al. studied through PCR and susceptibility testing the contamination of two-famous meat based Lebanese fast foods: Lahm-bi-Ajeen and Shawarma. The findings, presented in Table 3, show that these meat-based fast foods are public health hazard and risky vehicle for antibiotic resistant E. coli strains and the need for aggressive protective measure to implement hygienic practice and standards [33].
The third food product, regarded by the general public as "a healthy option", is ready-to-eat salads. However, several outbreaks were reported caused by Shiga toxin-producing E. coli (STEC) that were detected in vegetables, used to prepare these salads. In fact, contamination is possible at any stage of the food chain. Faour-Klingbeil et al. reported E. coli strains on fresh vegetables (Table 4). It also showed that inadequate post-harvest washing contributed to transmission of antimicrobial-resistant E. coli at wholesale and retail levels, and reports an increasing trend from fields to the markets indicating potential sources of fecal contamination throughout the food chain [35]. Finally, the contamination of aquatic Lebanese environments was reported by Harakeh et al. were 94.7% of the samples were contaminated with resistant E. coli and/or Salmonella through PCR detection method and disk diffusion susceptibility testing [49].
Listeria monocytogenes (L. monocytogenes), a Gram-positive, rod-shaped, facultative bacterium, is considered to be among the leading causes of death from foodborne illness. It is the agent of listeriosis, a life threatening foodborne disease for immunocompromised patients and pregnant women [21]. This bacterium is not routinely screened for in Lebanon and a lack of data exist, about the prevalent strains and their potential pathogenicity. Haidar-Ahmad et al., conducted a study to characterize L. monocytogenes at the strain level, to assess their virulence potential, and detect there in vitro biofilm forming ability in the Lebanese market. Samples collected in 2012-2013 from the Lebanese Agriculture Research Institute (local and imported food products in the Lebanese market) were tested for L. monocytogenes through PCR, Pulsed Field Gel Electrophoresis (PFGE) and BIONUMERICS analysis. The major findings are shown in Table 4. This study stresses the need for proper surveillance and the implementation of strict regulations on local and imported food [36].
A diary product: Qishta was studied by Kassaify et al. and 42% of selected samples have been reported to be contaminated by L. monocytogenes [26]. Harakeh et al. detected through PCR the presence of L. monocytogenes in traditionally consumed dairy-food products in Lebanon as shown in Table 2. These results provide an indication of the contamination levels and antimicrobial resistance of Listeria and emphasize the dangers associated with the emergence of multi-drug resistant Listeria in the environment resulting from the improper hygienic standards and indiscriminate use of antimicrobials [28].
Because ready-to-eat salads outside homes has become an increasing trend in the current lifestyles, Faour-Klingbeil et al., conducted a study aiming to determine microbiological quality of fresh-cut salads vegetables in small and medium sized foodservice establishments. Listeria spp. levels were statistically significant with cross-contamination and cleaning components (Table 4) [37].
Salmonella species, a motile, non-spore-forming, Gram-negative, and rodshaped bacterium belongs to the family Enterobacteriaceae and the tribe Salmonellae [21].
An outbreak that occurred in May 2004, as reported by bank employees in Beirut, had resulted in severe gastroenteritis after consumption of chicken noodles at a single excellent serving restaurant in Beirut. The central laboratory reported that this dish contamination was due to the presence of Salmonella enterica serovar Enteritidis (Table 3) [34]. Centre for Disease Control and Prevention (CDC) consider foodborne Salmonella outbreaks a huge threat for the public health [50].
In Lebanon, out-dated laws since 1930 are still governing the reporting process of "food poisoning". It is a mandatory for public health officers to eradicate outbreak from spreading by destruction of contaminated food and closing the corresponding facilities. The gaps of proper law enforced management of food poisoning will thus stimulate the needed changes for proper investigation, control and prevention for future outbreaks in Lebanon [34]. A study conducted by Kanj et al. investigating the epidemiology and the clinical manifestation of Typhoid fever strains in Lebanon from 2006-2007 among 120 patients suffering from Salmonella typhi, showed that most of these strains are susceptible to various antibiotic.
However, testing performed on these cases, the mode of transmission was not attributed to drinking water, thus spotting the light on food contamination [51].
A study conducted by Harakeh et al. on meat-based Lebanese fast food reported contamination by Salmonella paratyphi (serogroup A) along by E. coli by the confirmatory testing of PCR. Antibiotic susceptibility testing results were reported in Table 3. These results are alarming public health hazard where these fast food products are spreading resistant pathogenic organism [33].
As shown in Table 4, several reported international outbreaks have been documented in different countries due to imported Lebanese products since 2003. Unicomb et al. have reported several outbreaks outside Lebanon. Thus this calls for further control and quality management of basic preparation during handling these products at the manufacturing Lebanese industry and the need for local policies and procedures monitoring their effectiveness [38]. In 2011, a multistate Salmonella outbreak led to products recalls from market and thus further loss for Lebanese importing profits and the international market trust in Lebanese products [39].
Faour-Klingbeil et al. recommended strict temperature control and avoiding pre-wash chopping during handling of parsley for the optimal elimination of pathogenic microorganisms (Salmonella typhimurium) [52]. In another research studying also Salmonella typhimurium and conducted by the same authors, vigilant cleaning and sanitation procedures on cutting surfaces after use with fresh produce were highly required [53].
Staphylococcus aureus (S. aureus), a Gram-positive, non-motile, ubiquitous microorganism, is abundant in foods due to environmental, human, and animal contamination [21]. Naja and Mallat have shown that 39% of workers (n=196) in a Lebanese pastry factory had nasal carriage of Staphylococcus aureus with various resistance patterns. Added to the above further positive tuberculin test was found positive in 16.3% of the workers (n=301) [54]. As shown in Table 2, Serhan and Mattar studied Lebanese traditional artisanal goat milk cheeses and reported their physico-chemical and microbiological characteristics due to the high prevalence of diseases associated with the consumption of raw goat milk [27]. Zouhairi et al. evaluated the antimicrobial resistance of S. aureus and S. saprophyticus isolated from 3 Lebanese dairy-based food products. The results, in Table 2, indicate that locally made dairy-based foods might be alarming vehicles for the transmission of resistant Staphylococcus spp [29]. The third food product that is exposed to Staphylococcus aureus’ contamination is the ready-to-eat salads outside home. As indicated in Table 4, Faour-Klingbeil et al. reported the presence of Staphylococcus aureus and Salmonella spp. The authors concluded that inadequate post-harvest washing contributed to transmission of pathogens at wholesale and retail levels. These findings showed the uncontrolled usage of washing water, improper transporting and storing conditions, and further risks of cross-contamination [37].
Yersinia is small rod-shaped, Gram-negative coccibacilli that causes foodborne infection manifested as intestinal and systemic diseases (yersiniosis) [21]. It has been reported that Yersinia might be transmitted by eating contaminated dairy foods that is why Harakeh et al. evaluated the presence and antimicrobial profile of Yersinia enterocolitica in three Lebanese dairy based foods. 69% of identified isolates were from Baladi cheese, 19% from Shankleesh and 12% from Kishk. Susceptibility testing results are indicated in Table 2. The reported antibiotic resistances exceeded by far all the levels reported elsewhere [30]. Serhan et al. conducted a study about another diary product: Darfiyeh cheese. Through Polymerase Chain Reaction-Temporal Temperature Gel Electrophoresis (PCR-TTGE), classical PCR and quantitative PCR, several bacilli were identified (Table 2). These findings show that Lebanese dairy products’ contaminations by pathogens are highly alarming public health hazard and they are not prepared under proper hygienic practices. It is recommended to implement strict conditions in cheese and dairy products processing to prevent the hazards that may be involved with its consumption [22].
Conclusion
This paper reviewed the food safety situation in the Mediterranean region and showed that foodborne diseases remain an important problem in different countries and especially in Lebanon. The massive prevalence of pathogenic bacteria in Lebanese food industry shows that food safety practice in Lebanon is still in process and still far away from international standards. This is a major concern not only for local and international communities as a major health risk factor, but also for local industries in terms of economic loses in losses. Furthermore, the presence of resistant strains among most common food consumed in Lebanon especially among paediatrics highlights the desperate need for changes in health policies monitoring proper hygiene practices. Moreover, the Lebanese laws regulating food safety are out of date and need proper revision and embracing standardized proper hygiene practice and surveillance. These laws should regulate and monitor all food chain from harvesting, to washing, to production, to consumption. Also, the awareness, practice and attitudes should be addressed in local communities in both consumers and handlers. The standards should embrace Good Agriculture Practice (GAP), Good Hygiene Practice (GHP), Good Manufacturing Practice (GMP), Good Educational Practice (GEP), and Good Training Practice (GTrP). Though consumers are not directly related to food chain, however they need further education on awareness, behaviour and attitudes toward food safety. This should include reporting to health authorities to improve local surveillance on food safety practice. However, this step needs local efforts of ministries to provide guidelines for reporting process that will yield proper investigations and recommendations to improve the food industries practice instead of closing down.
Foodborne infections, due to bacterial contamination, need further research in the Mediterranean region and especially in Lebanon to be able to achieve comprehensive data and track the trace of contamination in food in order to protect the health of the consumers and ensure prosperity of the Lebanese food industry.
Conflict of Interest
The authors declare that they have no conflict of interest.REFERENCES
- Kamleh R, Jurdi M, Annous BA. Management of microbial food safety in Arab countries. J Food Prot. 2012;75:2082-2090.
- Food Safety: Importance for At-Risk Groups. Food and Drug Administration. 2018. https://www.fda.gov/Food/FoodborneIllnessContaminants/PeopleAtRisk/ucm352830.htm
- Gamarra RM. Food poisoning. Mescape. 2018. https://emedicine.medscape.com/article/175569-overview
- World Health Organization. Five Keys to Safer Food Manual. WHO Department of Food Safety, Zoonoses and Foodborne Diseases, Geneva, Switzerland. 2006.
- World Health Organization. WHO estimates of the global burden of foodborne diseases: foodborne disease burden epidemiology reference group 2007-2015. 2015.
- World Health Organization. Food safety. infographics: Estimates of the global burden of foodborne diseases. 2015. http://www.who.int/foodsafety/
- Food and Agriculture Organization of the United Nations, World Health Organization. FAO/WHO regional meeting on food safety for the near east. 2005. Amman, Jordan: FAO. http://www.fao.org/tempref/docrep/fao/Meeting/009/y6024e/y6024e00.pdf
- Badran A, Murad S, Baydoun E, Daghir N. Water, energy & food sustainability in the middle east. Springer International Publishing, New York; 2017.
- Elmi M. Food safety. East Mediterr Health J. 2008;14:143-149.
- Saleh I, Zouhairi O, Alwan N, Hawi A, Barbour E, Harakeh S. Antimicrobial resistance and pathogenicity of Escherichia coli isolated from common dairy products in the Lebanon. Ann Trop Med Parasitol. 2009;103:39-52.
- Hwalla N, El Khoury DTD. Lebanese Traditional Diets and Health Effects. In: De Meester F., Watson R.R. (eds) Wild-Type Food in Health Promotion and Disease Prevention. Humana Press. 2008.
- El-Jardali F, Hammoud R, Kamleh R, Jurdi M. K2P Briefing Note: Protecting Consumers in Lebanon: The need for effective food safety system. Knowledge to Policy (K2P) Centre. American University of Beirut, Lebanon. 2014.
- United Nations Industrial Development Organization. The integrated program for Lebanon to enhance the competitiveness of the Lebanese industry and its integration in the global market. Beirut, Lebanon. 2002.
- Hanna L, Karam M, Srour G. Consumers and food safety: Trust and understanding of Lebanese standards. J Food Sci Eng. 2011;1:390.
- Jaroudi SS. Assessment of food safety knowledge of the Lebanese consumers. 2009.
- Hassan HF, Dimassi H. Food safety and handling knowledge and practices of Lebanese university students. Food Control. 2014;40:127-133.
- Klingbeil DF, Kuri V, Todd E. Investigating a link of two different types of food business management to the food safety knowledge, attitudes and practices of food handlers in Beirut, Lebanon. Food Control. 2015;55:166-175.
- Mitri CB, Mahmoud D, El Gerges N, Jaoude MA. Food safety knowledge, attitudes and practices of food handlers in lebanese hospitals: A cross-sectional study. Food Control. 2018;94:78-84.
- Hassan HF, Dimassi H, Karam ZN. Self-reported food safety knowledge and practices of Lebanese food handlers in Lebanese households. Br Food J. 2018;120:518-530
- Abebe GK, Chalak A, Abiad MG. The effect of governance mechanisms on food safety in the supply chain: Evidence from the Lebanese dairy sector. J Sci Food Agric. 2017;97:2908-2918.
- Food and Drug Administration. Bad Bug Book, Foodborne Pathogenic Microorganisms and Natural Toxins. Second Edition. 2012.
- Serhan M, Grimal CC, Borges F, Junelles AMR, Hosri C, Fanni J. Bacterial diversity of Darfiyeh, a Lebanese artisanal raw goat's milk cheese. Food Microbiol. 2009;26:645-652.
- Al Shaar L, Chaaya M, Ghosn N, Mahfoud Z. Brucellosis outbreak in Chouf district of Lebanon in 2009: a case-control study. East Mediterr Health J. 2014; 20?:250-256.
- Alwan N, Saleh I, Beydoun E, Barbour E, Ghosn N, Harakeh S. Resistance of Brucella abortus isolated from Lebanese dairy-based food products against commonly used antimicrobials. Dairy Sci Technol. 2010;90:579-588.
- Gilbert RJ, De Louvois J, Donovan T, Little C, Nye K, Ribeiro CD, et al. Guidelines for the microbiological quality of some ready-to-eat foods sampled at the point of sale. PHLS Advisory Committee for Food and Dairy Products. Commun Dis Public Health. 2000;3:163-167.
- Kassaify ZG, Najjar M, Toufeili I, Malek A. Microbiological and chemical profile of Lebanese qishta [heat-coagulated milk]. East Mediterr Health J. 2010;16:926-931.
- Serhan M, Mattar J. Characterization of four Lebanese artisanal goat milk cheeses: Darfiyeh, Aricheh, Shankleesh and Serdale by physico-chemical, microbiological and sensory analyses. J Food Agric Environ. 2013;11:97-101.
- Harakeh S, Saleh I, Zouhairi O, Baydoun E, Barbour E, Alwan N. Antimicrobial resistance of Listeria monocytogenes isolated from dairy-based food products. Sci Total Environ. 2009;407:4022-4027.
- Zouhairi O, Saleh I, Alwan N, Toufeili I, Barbour E, Harakeh S. Antimicrobial resistance of Staphylococcus species isolated from Lebanese dairy products. East Mediterr Health J. 2010;16:1221-1225
- Harakeh S, Saleh I, Barbour E, Shaib H. Highly resistant Yersinia enterocolitica isolated from dairy based foods in Lebanon. Int Arab J Antimicrob Agents. 2012;2.
- Loukieh M, Mouannes E, Jaoudeh CA, Wakim LH, Fancello F, Zeidan MB. Street foods in Beirut city: An assessment of the food safety practices and of the microbiological quality. J Food Saf. 2018;38:e12455.
- El-Rami FE, Sleiman FT, Abdelnoor AM. Identification and antibacterial resistance of bacteria isolated from poultry. Pol J Microbiol. 2012;61:323-326.
- Harakeh S, Yassine H, Gharios M, Barbour E, Hajjar S, El-Fadel M, et al. Isolation, molecular characterization and antimicrobial resistance patterns of Salmonella and Escherichia coli isolates from meat-based fast food in Lebanon. Sci Total Environ. 2005;341:33-44.
- Hanna NM, Adib SM, Daoud Z. Food-borne salmonella outbreak at a bank cafeteria: an investigation in an Arab country in transition. East Mediterr Health J. 2009;15:470-474.
- Klingbeil DF, Kuri V, Fadlallah S, Matar GM. Prevalence of antimicrobial-resistant Escherichia coli from raw vegetables in Lebanon. J Infect Dev Ctries. 2016;10:354-362.
- Ahmad NH, Kissoyan KA, Fadlallah SM, El-Hajj R, Saleh M, Ghosn N, et al. Genotypic and virulence characteristics of Listeria monocytogenes recovered from food items in Lebanon. J Infect Dev Ctries. 2016;10:712-717.
- Klingbeil DF, Todd EC, Kuri V. Microbiological quality of ready-to-eat fresh vegetables and their link to food safety environment and handling practices in restaurants. LWT-Food Sci Technol. 2016;74:224-233.
- Unicomb LE, Simmons G, Merritt T, Gregory J, Nicol C, Jelfs P, et al. Sesame seed products contaminated with Salmonella: three outbreaks associated with tahini. Epidemiol Infect. 2005;133:1065-1072.
- Crowe SJ, Mahon BE, Vieira AR, Gould LH. Vital signs: multistate foodborne outbreaks—United States, 2010–2014. Morb Mortal Wkly Rep. 2015;64:1221-1225.
- Araj GF, Azzam RA. Seroprevalence of brucella antibodies among persons in high-risk occupation in Lebanon. Epidemiol Infect. 1996;117:281-288.
- Dabboussi F, Alam S, Mallat H, Hlais S, Hamze M. Preliminary study on the prevalence of Campylobacter in childhood diarrhoea in north Lebanon. East Mediterr Health J. 2012;18:1225-1228.
- Hamze M, Osman M, Mallat H, Achkar M. Antibiotic Susceptibility of Salmonella spp., Shigella spp. and enteropathogenic Escherichia coli strains isolated from diarrheic children in Tripoli, North Lebanon. Int Arab J Antimicrob Agents. 2016;6.
- Hijazi SM, Fawzi MA, Ali FM, Abd El Galil KH. Prevalence and characterization of extended-spectrum beta-lactamases producing Enterobacteriaceae in healthy children and associated risk factors. Ann Clin Microbiol Antimicrob. 2016;15:3.
- Cižman M. The use and resistance to antibiotics in the community. Int J Antimicrob Agents. 2003;21:297-307.
- Reinthaler FF, Posch J, Feierl G, Wüst G, Haas D, Ruckenbauer G, et al. Antibiotic resistance of E. coli in sewage and sludge. Water Res. 2003;37:1685-1690.
- Källman O, Fendukly F, Karlsson I, Kronvall G. Contribution of efflux to cefuroxime resistance in clinical isolates of Escherichia coli. Scand J Infect Dis. 2003;35:464-470.
- Soto SM, Lobato MJ, Mendoza MC. Class 1 integron-borne gene cassettes in multidrug-resistant Yersinia enterocolitica strains of different phenotypic and genetic types. Antimicrob Agents Chemother. 2003;47:421-426.
- Van Duijkeren E, Wannet WJ, Houwers DJ, Van Pelt W. Antimicrobial susceptibilities of Salmonella strains isolated from humans, cattle, pigs, and chickens in the Netherlands from 1984 to 2001. J Clin Microbiol. 2003;41:3574-3578.
- Harakeh S, Yassine H, El-Fadel M. Antimicrobial-resistant patterns of Escherichia coli and Salmonella strains in the aquatic Lebanese environments. Environ Pollut. 2006;143:269-277.
- Centers for Disease Control and Prevention (CDC). Preliminary FoodNet data on the incidence of foodborne illnesses--selected sites, United States, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:325.
- Kanj SS, Kanafani ZA, Shehab M, Sidani N, Baban T, Baltajian K, et al. Epidemiology, clinical manifestations, and molecular typing of salmonella typhi isolated from patients with typhoid fever in Lebanon. J Epidemiol Glob Health. 2015;5:159-165.
- Klingbeil DF, Kuri V, Todd EC. The influence of pre-wash chopping and storage conditions of parsley on the efficacy of disinfection against S. Typhimurium. Food Control. 2016;65:121-131.
- Klingbeil DF, Kuri V, Todd E. The transfer rate of Salmonella Typhimurium from contaminated parsley to other consecutively chopped batches via cutting boards under different food handling scenarios. Food Res Int. 2016;89:495-503.
- Naja M, Mallat H. Biological analysis of workers in the food sector in north Lebanon. East Mediterr Health J. 2008;14:1425-1434.
Citation: Harb C, Mouannes E, Zeidan MB, Nour AMA, Wakim LH (2020) Foodborne Pathogens Dilemma in the Mediterranean Diet: Case of Lebanon. J Food Process Technol 11:832. doi: 10.35248/2157-7110.20.11.832.
Copyright: © 2020 Harb C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.