Indexed In
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Access to Global Online Research in Agriculture (AGORA)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- SWB online catalog
- Publons
- Euro Pub
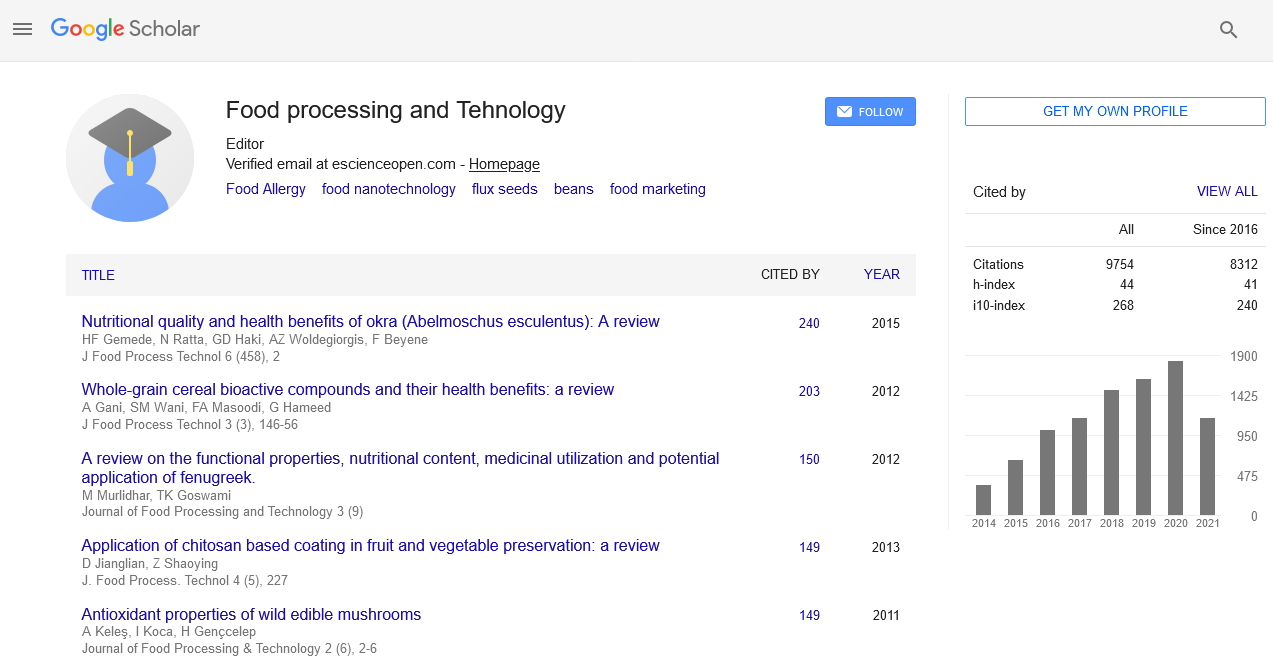
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2022) Volume 13, Issue 11
Food Allergy: Identification of T-Cell Epitope and Single-Cell Technology
Shimin Yang*Received: 04-Nov-2022, Manuscript No. JFPT-22-18948; Editor assigned: 07-Nov-2022, Pre QC No. JFPT-22-18948 (PQ); Reviewed: 21-Dec-2022, QC No. JFPT-22-18948; Revised: 28-Dec-2022, Manuscript No. JFPT-22-18948 (R); Published: 05-Dec-2022, DOI: 10.35248/2157-7110.22.13.965
Description
In developed nations, food allergies are common (affecting 5%-10% of the population), and their frequency has increased recently. Food allergy is an atopic condition brought on by an unwarranted immunologic reaction to a normally benign foodstuff. The most prevalent food allergens in the United States include peanut, milk, shellfish, tree nuts, egg, fin fish, wheat, and soy. Accidental consumption of these allergens is the main cause of anaphylaxis in this country. Double-blind placebocontrolled food challenge, an oral food challenge technique that has the potential to be harmful and needs to be carried out by highly qualified specialists, is the gold standard diagnostic approach for determining food allergy to date. Measurement of IgE antibody levels and skin prick tests are further diagnostic techniques, although they are not consistently predictive of clinical reaction and may be harmful. The clinical reactivity cannot be accurately predicted by antibody levels or skin prick testing, which may simply indicate allergen sensitization. The most popular course of action is allergy avoidance, which carries the danger of unintentional exposure. The US Food and Drug Administration has authorized oral immunotherapy (OIT) for peanut allergy; nevertheless, the patient population for this potential therapy is only those with milder forms of the condition. To effectively detect and treat food allergies, we thus need to understand the immunologic mechanisms at play, which will necessitate new methods.
IgE-mediated, non-IgE-mediated, or combined IgE and non-IgE-mediated are the three main categories used to describe food allergies. Evidently, in both IgE and non-IgE-mediated types of illness, antigen-specific T lymphocytes play a role in both sensitization and tolerance to dietary allergens. Antigen-specific CD4+ T cells have been found to be skewed toward a TH2 phenotype during IgE-mediated food allergy. These TH2 cells can release cytokines (IL-4, IL-5, and IL-13) that trigger mast cell, basophil, and eosinophil degranulation as well as B-cell synthesis of IgE, resulting in allergy symptoms and, in extreme cases, anaphylaxis. Although less frequent, non-IgE-mediated food allergies are believed to have mechanisms that are mediated by allergen-specific T cells. The underlying causes of the development and subsequent participation of these T-cell diseases in any type of food allergy are yet unknown. There may be prospects for improved food allergy diagnosis and therapy if the phenotypic markers of allergen-specific T lymphocytes that contribute to disease are understood and characterised. This necessitates the development of well-defined T-cell epitopes for dietary antigens. This brief review will highlight recent developments and new technologies in the study of T-cells and Tcell epitope discovery in food allergy while also highlighting areas for future study.
Food allergy and OIT: Single-cell technology and Tcell epitope
The low frequencies of these cells in blood and the lack of techniques able to classify them place restrictions on the study of allergen-specific T lymphocytes. New research opportunities have been made possible by the introduction of an experimental paradigm that combines antigen-specific cell selection assays (activation-induced marker, antigen-reactive T-cell enrichment, MHC class II tetramers, and cytokine secretion) with single-cell genomic, epigenomic, and immune repertoire sequencing. Based on their reactivity to specific antigens, these techniques enable the identification, isolation, and high-resolution Characterisation of low-frequency T-cell populations accountable for disease state. The best molecularly defined antigens, then, are those that can be administered as individual peptides, peptide pools, or as the payload of MHC-multimers and that can be reliably manufactured. Studies of infectious illness and non-food allergies have shown the advantage of employing peptide epitopes over crude extracts when describing antigen-specific Tcell responses since it enables us to separate T-cell populations responding to various targets. Large data sets and a wealth of knowledge can be produced by combining these tried-and-true methods with downstream genomics applications and antigenspecific cell selection. Food allergens have fewer known epitopes, but the field has been expanding. There are currently 21 known antigens and 496 T-cell epitopes that have been confirmed using various assays based on cell proliferation and cytokine production. The recognition we will be able to better understand the antigen-specific T cell profiles with the availability of more T-cell epitopes for various dietary allergies. The similarities and differences of T-cell phenotypes in food allergies may be further compared with phenotypes from other allergic and infectious illnesses by comparing antigen-specific Tcell profiles with various specificities and connecting them to an individual's allergic disease.
Citation: Yang S (2022) Food Allergy: Identification of T-Cell Epitope and Single-Cell Technology. J Food Process Technol. 13:965.
Copyright: © 2022 Yang S. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.