Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2020) Volume 11, Issue 5
Finding a Permanent Cure for Endometriosis Proving to be An Impossible Task Over Years of Evaluation
Kulvinder Kochar Kaur1*, Gautam Allahbadia1 and Mandeep Singh22Department of Neurology, Swami Satyanand Hospital, Baradri, Jalandhar, Punjab, India
Received: 27-Jul-2020 Published: 17-Aug-2020, DOI: 10.35248/2155-9627.20.11.360
Description
Endometriosis represents an enigmatic disease where following decades of studying and trying to find a permanent medical cure has eluded us just like Socrates quoted-I neither know nor think that I know. By definition it is presence of endometrial like tissue outside the uterus and associated with a chronic inflammatory reaction. Cellular proliferation, invasion, and neoangiogenesis are key to the establishment, progression and recurrence of the disease. Lot of etio pathophysiology have been proposed over years with newer therapies developed but practically all therapies are suppressive, not curative, with high recurrence. Deep infiltrating endometiosis is a subtype involving, rectovaginal septum, bowel, ureters or bladder. For hormone suppression GnRH agonists are usually the 1st agents because they suppress ovarian hormone production and inhibit the growth of the extra pelvic endometrial tissue [1-3]. Central sensitization is being increasingly recognized as an important factor in the pathogenesis of endometriosis associated pain, besides the peripheral nociceptive effects of endometriotic lesions. Central sensitization amplifies pain signaling from the periphery. It is associated with myofascial trigger point and psychological comorbidities. Clinically tricyclics and antiepileptics can be used although there are no clinical trials in endometriosis. Endometriosis as a major cause of CPP acts as a cyclic source of peripheral nociceptive input. Recent data supports the hypothesis that changes in the central pain system also play an important role in the development of chronic pain, regardless of the presence of endometriosis. Multidisciplinary approaches to the sensitized patient should also be considered, such as physiotherapy, and cognitive treatment although more clinical trials specifically in endometriosis is required [4-6].
Treatment choices for symptomatic endometriosis are based on patient preferences, treatment goals, the side effect, efficacy, cost, associated comorbidities and availability. Recent discoveries in neuroendocrinology, endocrinology, tumorigenesis and genomics point that A group of hypothalamic neurons colocalized in the arcuate nucleus involving 3 neuropeptides-kisspeptins, neurokinin B/Dynorphin inhibit the pulsatile release of GnRH. This has led to the establishment of kisspeptin, NKB/Dynorphin (KNDy) hypothesis which suggests that KNDy neuronsin the arcuate nucleus may interact to control the release and pulsatility of GnRH. Kisspeptin is differentially expressed at the level of endometrium in patients with and without endometriosis. In addition kp expression was statistically significantly lower in deep infiltrating endometriosis compared to superficial peritoneal disease. This has important implications not only for improving our understanding of the pathogenesis but also for optimizing novel hormonal agents to treat different disease phenotype (Figure 1) [7].
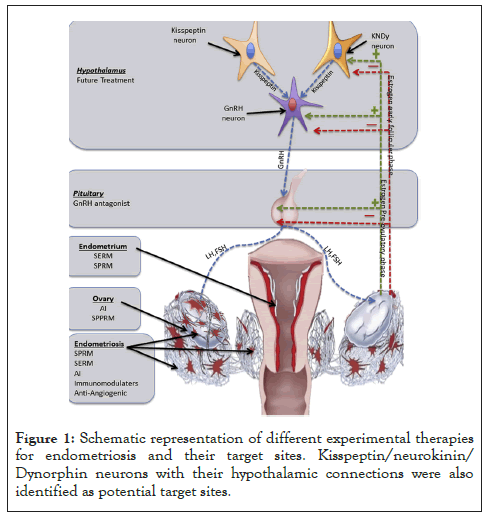
Figure 1: Schematic representation of different experimental therapies for endometriosis and their target sites. Kisspeptin/neurokinin/ Dynorphin neurons with their hypothalamic connections were also identified as potential target sites.
Trying to get methods of blocking this angiogenesis might help in innovative ways of tackling Endometriosis. Bone Marrow (BM)- derived endothelial cells aid in vasculogenesis, that includes the ones for Endometriosis as well as uterus at the time of pregnancy. In view of their part in Endometriosis lesions as well as recruitment during active disease, these endothelial progenitor cells are good
Trying to get methods of blocking this angiogenesis might help in innovative ways of tackling Endometriosis. Bone Marrow (BM)- derived endothelial cells aid in vasculogenesis, that includes the ones for Endometriosis as well as uterus at the time of pregnancy. In view of their part in Endometriosis lesions as well as recruitment during active disease, these endothelial progenitor cells are good targets for therapeutic intervention [8].
Shigesi evaluated the association between endometriosis and autoimmune diseases. They found an association between endometriosis and several autoimmune diseases, including Systemic Lupus Erythematosus (SLE), Sjögren's Syndrome (SS), Rheumatoid Arthritis (RA), autoimmune thyroid disorder, Coeliac Disease (CLD), Multiple Sclerosis (MS), Inflammatory Bowel Disease (IBD), and Addison's disease. However poor quality of evidence seen due to bias in the majority of the chosen study designs and statistical analyses. Only 4 of the 26 studies could provide high- quality evidence, and supported a statistically significant association between endometriosis and at least 1 autoimmune disease: SLE, SS, RA, CLD, MS, or IBD. The observed associations between endometriosis and autoimmune diseases suggest that clinicians need to be aware of the potential coexistence of endometriosis and autoimmune diseases when either is diagnosed. Scientists interested in research studies on endometriosis or autoimmune diseases should consider the likelihood of comorbidity when studying these two types of conditions. Well-designed large prospective cohort studies with confounding control and mediation quantification, as well as genetic and biological studies, are needed to generate further insights into whether endometriosis is a risk factor for, or a consequence of, autoimmune diseases, and whether these two types of disorders share pathophysiological mechanisms even if they arise independently. Such insights may offer opportunities for the development of novel non-hormonal medications such as immuno- modulators or repurposing of existing immunomodulatory therapies for endometriosis [9].
Denisa Capraş tried to study if studies on therapy evaluation integrate high-quality scientific evidence in daily practice, aiming to assess whether Randomized Controlled Trials (RCTs) on endometriosis therapy follow methodological criteria corresponding to the RCTs’ specific level in the None of the evaluated RCTs met all the methodological criteria, none had only a low risk of bias and provided sufficient details on methods and randomization to allow for the reproduction and replication of the study. Consequently, the appropriate level of scientific evidence (level 1, degree 1b) could not be granted. On endometriosis therapy, this study evaluated the quality of reporting in RCTs and not the quality of how the studies were performed [10]. Further COX-2 inhibitors, telmesartan, natural agents resveratrol, are getting evaluated yet no permanent answer is in sight.
REFERENCES
- Kulvinder KK, Allahbadia GN, Singh M. An update on pathophysiology and medical management of endometriosis. Adv Repr Sci. 2016; 4(2): 53-73.
- Kulvinder kk, Allahbadia GN, Singh M. Meeting the challenges of endometriosis associated pain-newer options for future and research directions. BAOJ Bio info. 2017; 12(1): 1- 9.
- Kulvinder KK, Allahbadia GN, Singh M. Kisspeptins in human reproduction-future therapeutic potentials. J Assist Reprod Genet. 2012; 29(10): 999-1011.
- Abdelkareem A, Ait-Allah A, Rasheed S, Helmy J ,Yong P, Bedaiwy M. Differential expression of kisspeptin in patients with and without endometriosis. Fertil Steril. 2016; 106: e274.
- SanIes AS, Harris RE, Napadow V, Kim J, Neshewat G, Kairys A, et al. Changes in regional gray matter volume in women with chronic pelvic pain : A voxel based morphometry study. Pain. 2012; 153: 1006-14.
- Williams C, Hoang L, Yosef A, Alotaibi F, Allaire C, Brotto L, et al. Nerve bundles and deep dyspareunia in endometriosis. Rep rod Sci. 2016; 23: 892-901.
- Bedaiwy MA, Alfaraj S, Yong P, Casper R. New developments in the medical treatment of endometriosis. Fertil Steril. 2017; 107(3): 555-565.
- Kulvinder KK, Allahbadia GN, Singh M. Developing therapies that prevent progenitor cell migration for preventing the development and further growth of endometriotic lesions-future prospects-A Short Communication. Perc Rep Med. 2020; 3(5): 121-125
- Shigesi N, Kwaskoff M, Kirtkley S, Feng Q, Fang H. The association between endometriosis and autoimmune diseases: A systematic review and meta-analysis. Hum Reprod Update. 2019; 25(4): 486-503.
- Denis CR, Urda EA, Bolboaca SD. Is scientific medical literature related to endometriosis treatment evidence-based? A systematic review on methodological quality of randomized clinical trials. Med Kau. 2019; 55(7): 372.
Citation: Kaur KK, Allahbadia G, Singh M (2020) Finding a Permanent Cure for Endometriosis-Proving to be An Impossible Task Over Years of| Evaluation. J Clin Res Bioeth. 11:360.
Copyright: © 2020 Kaur KK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

