Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
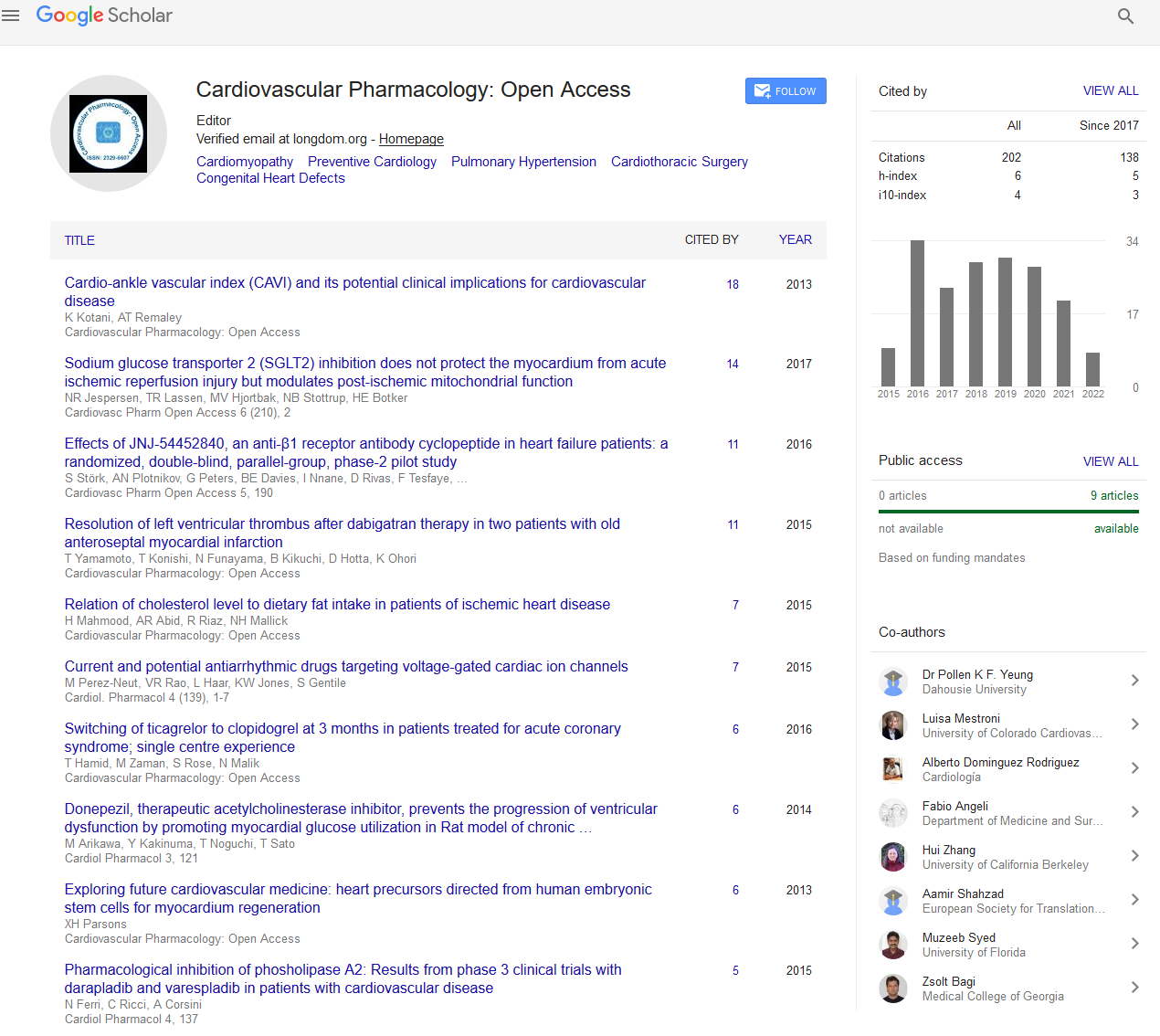
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2022) Volume 11, Issue 7
Factors Affecting Cardiac Output and Blood Pressure
David R Canestro*Received: 04-Jul-2022, Manuscript No. CPO-22-17630; Editor assigned: 07-Jul-2022, Pre QC No. CPO-22-17630 (PQ); Reviewed: 21-Jul-2022, QC No. CPO-22-17630; Revised: 28-Jul-2022, Manuscript No. CPO-22-17630 (R); Published: 04-Aug-2022, DOI: 10.35248/2329-6607.22.11.293
Description
Cardiac output, expressed in liters/minute, is the amount of blood the heart pumps in 1 minute. Cardiac output is logically equal to the product of the stroke volume and the number of beats per minute (heart rate). Easy enough, one may think, but the term cardiac in cardiac output is potentially misleading with clinician's sometimes assuming that to interpret cardiac output they must focus on the heart. The heart is just one part of the much larger cardiovascular system, however, and the amount of blood it pumps is dependent on both cardiac and extra cardiac factors.
The cardiac output is the amount of blood pumped out from each ventricle per minute. In a resting, supine man, it averages about 5.5 L/min (80 mL x 70 beats/min). The cardiac index is the cardiac output/minute/square meter of body surface area. It averages about 3.2 L/min/m2. The cardiac output represents the volume of blood that is delivered to the body, and is therefore an important factor in the determination of the effectiveness of the heart to deliver blood to the rest of the body, (i.e., determining heart failure, inadequate circulation, etc). By definition, two major factors contribute to the cardiac output: the heart rate, which is the number of times a given volume of blood is ejected per unit of time, and the stroke volume, which is effectively the volume of blood that the heart can fill with, which will be ejected upon contraction. Increasing the heart rate effectively increases the cardiac output by increasing the number of cardiac volumes of blood released into the system. As long as the heart is given a long enough diastole (resting phase), the effective volume of heart outputs will increase. The stroke volume can be increased by three different factors: the preload, the afterload, and the myocardial contractility.
Preload-The initial length of the cardiac muscle fibers also has an effect on the force of contraction. When the ventricles are filled with more blood, the muscle fibers are stretched so that there is maximal overlap of actin and myosin fibers, increasing the strength of contraction. Therefore, when more venous blood returns to the heart, the force of cardiac muscle contraction is automatically increased. During exercise, for example, there is dilation of blood vessels in the skeletal muscles, with resultant reduction in peripheral resistance and increased flow of blood back to the heart via veins. This relationship between the end diastolic volume and force of contraction during systole is known as the Frank-Starling law of the heart.
Contractility- The force of contraction of individual fibers (contractility) can be increased by various agents that facilitate entry of calcium into the myocardial fibers. Stimulation of sympathetic nerves to the heart, presence of adrenaline, noradrenaline in the blood, and increased calcium levels in the blood are some factors that increase contractility. Contractility is decreased by parasympathetic stimulation, inhibition of sympathetic activity, in-creased potassium levels in the blood, acidosis, and presence of drugs that decrease calcium into the myocardial fibers, among others.
Afterload- Increased arterial blood pressure will interfere with the force of contraction. This causes an initial decrease in the stroke volume and cardiac output. Indeed, the end-diastolic volume of the next beat increases. This leads to increased force of contraction and stroke volume and cardiac output.
The heart rate- Increased heart rate within limits increases cardiac output. The heart rate is primarily affected by autonomic nerves, with sympathetic stimulation increasing the rate and parasympathetic decreasing it.
Blood volume and blood viscosity-Increased blood volume helps the venous return, while hemorrhage decreases the venous return and cardiac output. On the other hand, increased blood viscosity retards the venous return, but in conditions of low blood viscosity such as anemia, the venous return and cardiac output are increased.
Citation: Canestro RC (2022) Factors Affecting Cardiac Output and Blood Pressure. Cardiovasc Pharm. 11:293
Copyright: © 2022 Canestro RC. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.