Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
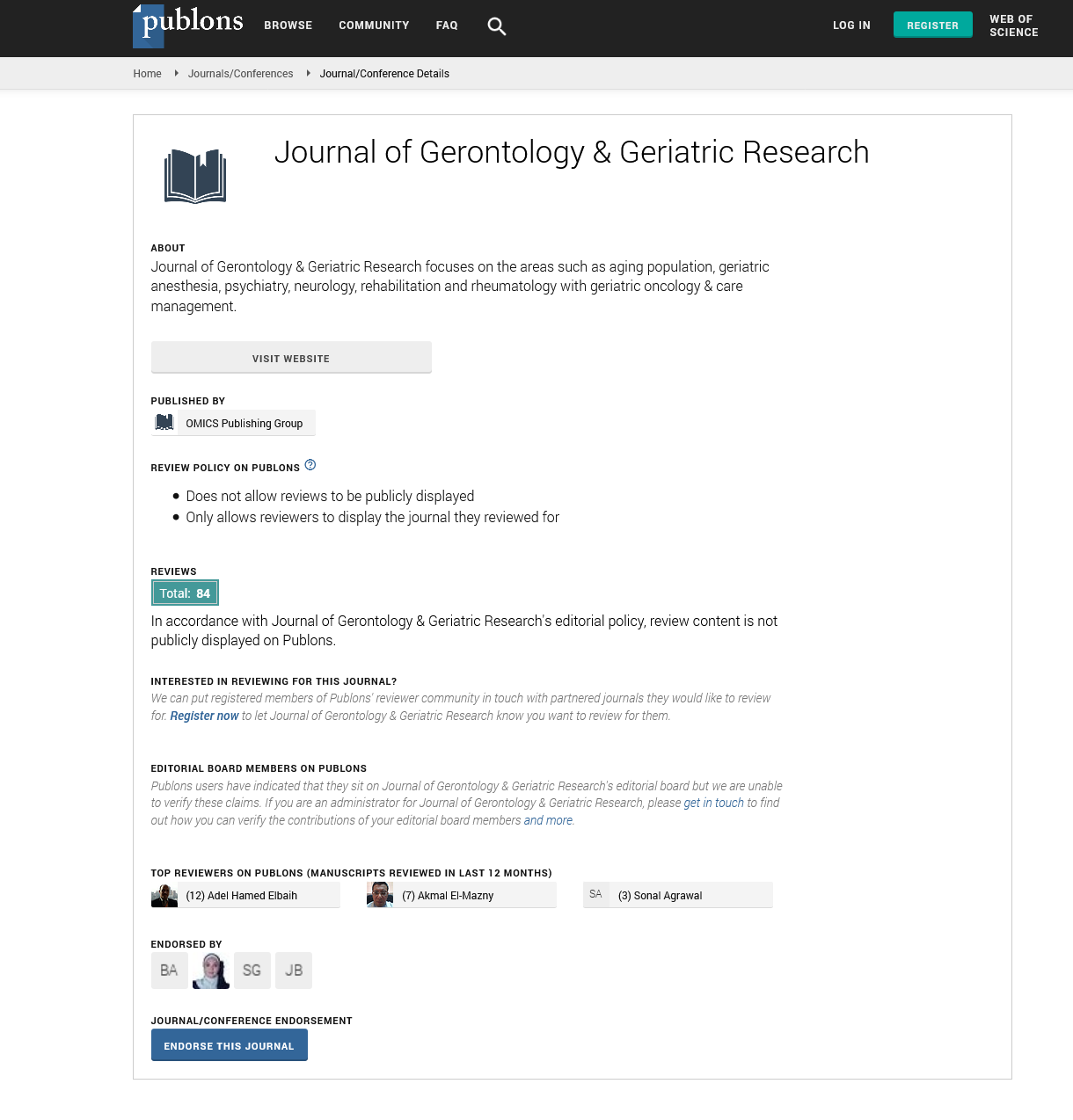
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2024) Volume 13, Issue 1
Exploring the Prevalence of Dysphagia in Individuals Residing in Residential Aged Care Facilities
Nicole Aaron*Received: 01-Feb-2024, Manuscript No. jggr-24-25273; Editor assigned: 02-Feb-2024, Pre QC No. P-25273; Reviewed: 16-Feb-2024, QC No. Q-25273; Revised: 22-Feb-2024, Manuscript No. R-25273; Published: 29-Feb-2024, DOI: 10.35248/2167-7182.2024.13.714
Introduction
Dysphagia, the medical term for difficulty swallowing, is a prevalent issue among older adults, particularly those residing in residential aged care facilities. This article aims to explore the prevalence of dysphagia in individuals living in RACFs, its impact on their health and quality of life, contributing factors, assessment methods, and strategies for management and prevention. Dysphagia is a common and often overlooked problem in RACFs, affecting a significant proportion of residents.
Studies indicate that up to 50-75% of older adults in RACFs experience some degree of dysphagia, making it a major health concern in this population [1-3]. The prevalence varies depending on factors such as age, comorbidities, cognitive function, and the presence of neurological conditions like dementia and stroke. Dysphagia can have profound consequences on the health and quality of life of individuals in RACFs. It can lead to malnutrition, dehydration, aspiration pneumonia, weight loss, and social isolation. Moreover, dysphagia-related complications often result in hospitalizations, increased healthcare costs, and decreased overall well-being among residents. Several factors contribute to the development of dysphagia in RACF residents.
Description
Early identification and assessment of dysphagia are crucial for effective management. Various screening tools and assessment protocols are used in RACFs to evaluate swallowing function. These may include bedside swallowing assessments, standardized swallowing questionnaires, videofluoroscopic swallow studies, fiberoptic endoscopic evaluations of swallowing, and comprehensive clinical evaluations by speech-language pathologists. Management of dysphagia in RACFs involves a multidisciplinary approach, including dietary modifications, swallowing rehabilitation exercises, assistive feeding techniques, medication management, and environmental modifications. Speech-language pathologists play a central role in developing individualized care plans and providing training to staff and caregivers on safe swallowing practices.
These include age-related changes in swallowing function, neurological conditions (e.g., stroke, Parkinson's disease), cognitive impairment, medication side effects, oral health problems, and structural abnormalities of the oropharyngeal area. Additionally, environmental factors such as inadequate staffing, improper feeding techniques, and limited access to specialized dysphagia management services can exacerbate the problem. Preventive measures are equally important in addressing dysphagia in RACFs [4,5]. These may include routine oral care, promoting hydration and proper nutrition, optimizing medication regimens, implementing dysphagia-friendly dining environments, and regular monitoring of swallowing function. Education programs for staff, residents, and families can also raise awareness and facilitate early detection and intervention. Dysphagia is a prevalent and serious issue affecting individuals living in residential aged care facilities.
Conclusion
Its impact on health and quality of life underscores the importance of proactive identification, comprehensive assessment, and effective management strategies. By addressing contributing factors, implementing preventive measures, and fostering interdisciplinary collaboration, RACFs can enhance the wellbeing and outcomes of residents with dysphagia. Further research is needed to explore novel interventions and best practices for optimizing swallowing function in this vulnerable population.
Acknowledgement
None.
Conflict of Interest
None.
References
- Baxa MC, Haddadian EJ, Jumper JM, Freed KF, Sosnick TR. Loss of conformational entropy in protein folding calculated using realistic ensembles and its implications for NMR-based calculations. Proc Natl Acad Sci 2014;111:15396-401.
- Trbovic N, Cho JH, Abel R, Friesner RA, Rance M, Palmer III AG. Protein side-chain dynamics and residual conformational entropy. J Am Chem Soc 2009;131:615-622.
- Faraggi E, Dunker AK, Jernigan RL, Kloczkowski A. Entropy, fluctuations, and disordered proteins. Entropy 2019; 21:764.
- Dyakin VV, Lajtha A, Dyakina‐Fagnano NV. Racemization Hypothesis of Neurodegeneration (RHND) developing topics. Alzheimer’s Dement 2020; 16:e047697.
- Balchin D, Hayer‐Hartl M, Hartl FU. Recent advances in understanding catalysis of protein folding by molecular chaperones. FEBS Let 2020; 594:2770-81.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Aaron N (2024). Exploring the Prevalence of Dysphagia in Individuals Residing in Residential Aged Care Facilities. J Gerontol Geriatr Res. 13: 714.
Copyright: © 2024 Aaron N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.