Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
- Google Scholar
- Quality Open Access Market
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2025) Volume 11, Issue 1
EXPLORING INTRATHECAL THERAPY IN CANCER PAIN: A REVIEW WITH CASE STUDY PERSPECTIVES
Vahid Mohabbati1*, Parsa Mohabbati2 and Mohammadkazem Papan32Department of Medicine, Pain Management Centre, Sydney, Australia
3Department of Medicine, Macquarie University, Sydney, Australia
Received: 23-Jan-2025, Manuscript No. JPMME-25-28325 ; Editor assigned: 27-Jan-2025, Pre QC No. JPMME-25-28325 (PQ); Reviewed: 10-Feb-2025, QC No. JPMME-25-28325 ; Revised: 17-Feb-2025, Manuscript No. JPMME-25-28325(R); Published: 26-Feb-2025, DOI: 10.35248/2684-1320.25.11.306
Abstract
Background: Intrathecal therapy, involving the direct administration of medications into the spinal canal, presents a targeted approach for managing diverse medical conditions, particularly cancer-related pain and neurological disorders. This review explores the historical evolution, rationale and efficacy of intrathecal therapy across various medical contexts and cancer pain.
Objectives: Beginning with a definition and mechanistic overview, the review demonstrates the localized drug delivery advantages of intrathecal therapy. It traces the historical trajectory, from early use of intrathecal morphine and baclofen to contemporary intrathecal drug delivery systems, highlighting the foundational studies that propelled its development. Central to the review is the examination of intrathecal therapy’s role in cancer pain management. Emphasizing the multidimensional impact of cancer-related pain, the review evaluates evidence supporting the superiority of intrathecal opioids and non-opioids over conventional delivery methods. Despite its proven efficacy, barriers to wider acceptance and utilization in refractory cancer pain management are discussed.
Methods: We present a series of case studies showcasing the clinical utility and therapeutic efficacy of IDDS in managing complex cancer-related pain. Each case highlights the role of intrathecal therapy in optimizing pain management, improving functionality and enhancing quality of life.
Results: All patients experienced meaningful pain relief and enhanced quality of life with intrathecal therapy. Common adverse effects, including pruritus and nausea, were managed effectively through dose adjustments and adjunctive treatments. The interventions also reduced hospital admissions, allowing patients to spend more time in community settings.
Conclusion: Intrathecal analgesia offers a valuable alternative for patients with refractory cancer pain, addressing the limitations of systemic therapies. Tailored intrathecal interventions, supported by multidisciplinary care, can achieve optimal pain control, improve functionality and enhance patient comfort in advanced disease stages.
Keywords
Intrathecal therapy; Cancer pain management; Interventional pain management; Drug delivery; Analgesia
Introduction
Intrathecal therapy refers to the administration of medications directly into the intrathecal space, which is the space surrounding the spinal cord and filled with Cerebrospinal Fluid (CSF). This route of drug delivery allows for targeted and localized treatment of various conditions, including pain management, spasticity and certain neurological disorders [1]. Intrathecal therapy is commonly used for the long-term management of intractable cancer and non-cancer pain, as well as spasticity. It is considered when other treatment options, such as oral medications or spinal cord stimulation, have failed to provide adequate relief [2].
Intrathecal therapy, specifically Intrathecal Drug Delivery (ITDD) involves the administration of analgesic drugs directly into the intrathecal space, providing superior pain relief with smaller doses of analgesics compared to other routes of administration. ITDD has been used for over 100 years; with newer technology using reservoirs to deliver medication [3]. Opiates such as morphine, dilaudid fentanyl and sufentanil are commonly administered via ITDD for cancer-related and non-malignant pain. Studies have shown that ITDD can significantly improve the quality of life for patients with chronic and cancer pain [4]. In a study evaluating the outcome of intrathecal opioids in chronic non-cancer pain, patients who received intrathecal opioid therapy reported global pain relief and improved physical activity [5]. Another study comparing intrathecal morphine administration with oral or transdermal treatment found better pain control and fewer side effects with intrathecal opioids.
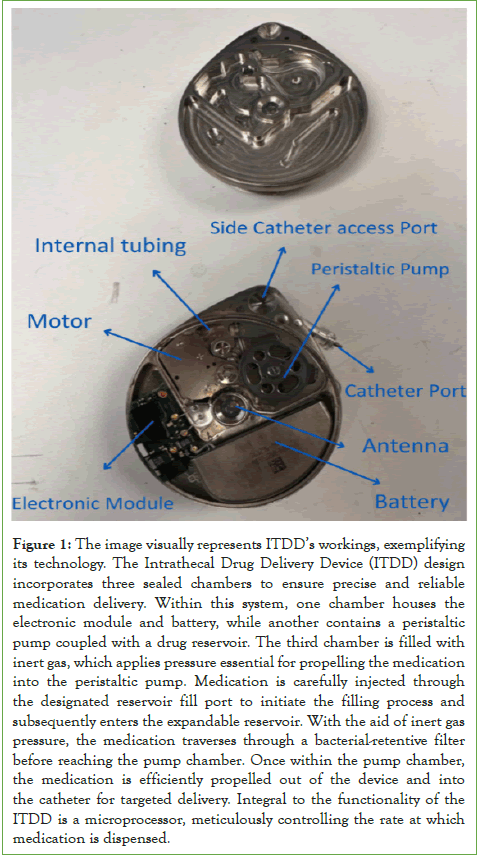
Intrathecal ziconotide, a non-opioid analgesic, has also been investigated as a treatment option for refractory chronic pain. The efficacy of intrathecal ziconotide for severe chronic refractory non-cancer pain was demonstrated in placebo-controlled trials [6]. Intrathecal therapy is not limited to pain management. It can also be used in the treatment of certain neurological disorders. For example, in the management of Chediak-Higashi syndrome, intrathecal therapy with methotrexate and prednisone is recommended for patients with evidence of central nervous system disease progression (Figure 1) [7].
Figure 1: The image visually represents ITDD’s workings, exemplifying its technology. The Intrathecal Drug Delivery Device (ITDD) design incorporates three sealed chambers to ensure precise and reliable medication delivery. Within this system, one chamber houses the electronic module and battery, while another contains a peristaltic pump coupled with a drug reservoir. The third chamber is filled with inert gas, which applies pressure essential for propelling the medication into the peristaltic pump. Medication is carefully injected through the designated reservoir fill port to initiate the filling process and subsequently enters the expandable reservoir. With the aid of inert gas pressure, the medication traverses through a bacterial-retentive filter before reaching the pump chamber. Once within the pump chamber, the medication is efficiently propelled out of the device and into the catheter for targeted delivery. Integral to the functionality of the ITDD is a microprocessor, meticulously controlling the rate at which medication is dispensed.
Literature Review
Prevalence, impact on quality of life and challenges in management of cancer-related pain
Cancer pain can have a significant impact on a patient’s performance status, mood states and level of hope. Patients with cancer pain often report lower levels of performance status and higher levels of total mood disturbance compared to cancer patients without pain. The multidimensional nature of the cancer pain experience is supported by the findings of a study that investigated the impact of cancer pain on patient’s performance status, emotional state and level of hope [8]. Studies have shown that more than 50% of cancer patients in the United States of America experience pain, with pain being most prevalent among patients with a high disease burden [9].
The prevalence of cancer-related pain is high and it is considered a top priority in comprehensive cancer care. To address these challenges, various guidelines and standards have been developed for the management of cancer-related pain. European Society for Medical Oncology (ESMO) Clinical Practice Guidelines is an essential resource for healthcare professionals in oncology. These guidelines provide evidence-based recommendations for the diagnosis, treatment and follow-up of various cancer types [10,11]. The European Pain Federation (EFIC) task force on cancer pain has also developed standards for cancer-related pain management across Europe. These guidelines and standards aim to reduce pain and its impact on daily living through tailored treatment and increase patient’s self-management ability [12].
There are barriers that compromise pain management effectiveness in cancer pain patients, such as poor pain communication, fear of addiction and tolerance, fear of drug side effects, anxiety, depression and socio-demographic factors. These barriers significantly compromise pain management effectiveness and affect cancer patient’s quality of life [13]. Self-management of cancer pain is a vital aspect of pain management. It involves patients making decisions to manage their pain. It also involves enhancing their self-efficacy by solving pain problems and incorporating pain-relieving strategies into daily life through interactions with healthcare professionals. Self-management of cancer pain includes interaction with healthcare professionals, decision-making in pain management, a process for solving pain-related problems, selfefficacy and incorporating strategies for pain relief into daily life [14].
Pain assessment should be based on patient-reported outcomes, as this is considered standard practice when assessing cancerrelated pain management outcomes [15]. Healthcare professional’s perspectives show knowledge gaps and impediments to successful cancer pain management. Nurses and oncology professionals plays an important role in managing cancer pain. However, their knowledge, perceived barriers and practices regarding cancer pain management need improvement [16]. There is a need for ongoing education and training for healthcare professionals to undertake basic pain assessment, initiate basic pain management and correctly refer for more specialist support [17].
Rationale for intrathecal therapy in cancer pain management
The use of intrathecal drug delivery for cancer pain management dates back several decades. Early studies described the use of intrathecal morphine for cancer pain analgesia and subsequent research examined the application of intrathecal analgesia for specific types of cancer pain, such as pancreatic cancer pain. These studies laid the foundation for the development and advancement of intrathecal drug delivery systems for cancer pain management [18]. Several studies have demonstrated the effectiveness of ITDD in providing pain relief for cancer patients. A randomized controlled trial found that intrathecal ziconotide relieved pain in patients with cancer or Acquired Immunodeficiency Syndrome (AIDS) over a short follow-up period.
Another study showed that intrathecal drug delivery alleviated cancer pain in patients whose standard analgesic measures failed [19,20]. Intrathecal morphine infusion therapy has been found to be effective in managing refractory cancer pain without serious complications. Additionally, intrathecal morphine infusion therapy has been shown to provide effective cancer pain management in Chinese patients [21]. Intrathecal drug delivery is increasingly used in cancer pain management. It has been advocated for wider application in cancer pain patients [22].
A Cochrane review published in 2005 included a randomized controlled trial comparing intrathecal morphine with conventional delivery of morphine in patients with cancer pain. The study concluded that ITDD was more effective in controlling pain and reducing adverse effects compared to conventional delivery methods [23]. One study evaluated the outcome of intrathecal opioids in 88 patients with chronic non-cancer pain and found that intrathecal opioid therapy provided global pain relief and improved physical activity.
Earlier methods and medications used
One of the earliest intrathecal medications is baclofen, a muscle relaxant. In 1991, intrathecal baclofen was first used in children with spastic cerebral palsy. Baclofen remains a mainstay of intrathecal therapy for spasticity and is FDA-approved for this indication [24]. Another commonly used intrathecal medication is morphine, an opioid analgesic. Morphine is the most commonly used intrathecal opioid and evidence suggests that the formation of granulomatous masses is related to higher doses [25]. In addition to baclofen and morphine, other medications have been used for intrathecal therapy. Ziconotide, an omega-conotoxin, is a nonopioid analgesic that has been studied for intrathecal use in the treatment of severe chronic pain [26]. Rituximab, a monoclonal antibody, has been used for intrathecal therapy in patients with Central Nervous System (CNS) disease failing to respond to intrathecal chemotherapy [27]. Methotrexate, either alone or in combination with other drugs, has been used for intrathecal therapy in the prevention of CNS leukemia [28,29]. Gabapentin, an anticonvulsant, has also been studied for its potential use in intrathecal pain management [30,31].
Anatomy and physiology of the intrathecal space
The intrathecal space is a significant central nervous system component, playing a vital role in various physiological processes. Contrast-enhanced Magnetic Resonance Imaging (MRI) studies have revealed that Cerebrospinal Fluid (CSF) recirculates through the brain parenchyma along paravascular spaces and exchanges with Interstitial Fluid (ISF). This process, known as CSF-ISF exchange, challenges the traditional model of CSF secretion and reabsorption. Additionally, Magnetic Resonance Imaging (MRI) imaging of intrathecally-administered contrast agents has shown that CSF flows along pathways resembling the glymphatic system, which is involved in waste clearance in the brain. These findings highlight the dynamic nature of CSF flow within the intrathecal space and its interaction with the brain parenchyma [32,33].
Intrathecal administration is commonly used in various medical procedures, such as myelography and drug delivery. Myelography involves the intrathecal injection of contrast agents to visualize the intradural/subarachnoid space and detect epidural metastases [34]. Intrathecal drug delivery is utilized for pain management, anesthesia and therapeutic interventions. For example, in the context of cesarean delivery, the spread of intrathecal local anesthetic can be influenced by the volume of the epidural space. This is due to the constriction of epidural veins. Understanding the anatomy of the intrathecal space is essential for optimizing drug delivery and achieving desired therapeutic outcomes [35]. Ultrasoundguided procedures have limitations in visualizing the real-time propagation of injectables in the epidural or intrathecal space due to limited resolution at deep levels and near bony surfaces. However, advancements in ultrasound technology may overcome these limitations and enhance intrathecal space visualization during procedures [36].
Intrathecal access is essential for the administration of continuous intrathecal drug delivery systems, such as baclofen pumps for spasticity management [37]. The implantation of a catheter in the intrathecal space allows for the continuous delivery of drugs directly to the central nervous system, bypassing systemic circulation [38]. The anatomy and physiology of the intrathecal space are complex and dynamic. It plays a significant role in CSF circulation, waste clearance and drug delivery. Understanding the complications of the intrathecal space is essential for optimizing medical procedures and achieving desired therapeutic outcomes.
Pharmacokinetics and pharmacodynamics of drugs delivered intrathecally
The pharmacokinetics of drugs delivered intrathecally involves the absorption, distribution, metabolism and elimination of drugs within the CSF and the Central Nervous System (CNS). When drugs are administered intrathecally, they penetrate the brain parenchyma and exert therapeutic effects. However, the penetration of drugs into the brain parenchyma can be influenced by various factors, including the Blood-Brain Barrier (BBB) and efflux transporters. Efflux transporters, such as ATP-Binding Cassette (ABC) transporters, can actively pump drugs out of the brain, limiting their distribution [39].
Pharmacodynamics of drugs delivered intrathecally involves the interaction of drugs with their target receptors in the CNS. For example, opioids such as morphine, dilaudid, fentanyl and sufentanil are commonly administered intrathecally for cancerrelated and non-malignant pain. These opioids exert their analgesic effects by binding to opioid receptors in the spinal cord, inhibiting pain signal transmission [4]. The BBB acts as a protective barrier that restricts the entry of certain substances from the blood into the brain and other drugs, such as protein therapeutics, can also be delivered intrathecally to target specific receptors or pathways in the CNS [40].
Mechanisms underlying pain relief
Pain relief with intrathecal therapy is multifactorial. One of the main mechanisms is the activation of opioid receptors in the spinal cord. Opioid drugs, such as morphine and sufentanil, are commonly used in intrathecal therapy. They bind to opioid receptors in the dorsal horn of the spinal cord, inhibiting pain signals transmission. The efficacy of intrathecal drug delivery has been extensively studied in patients with various types of pain, including cancer pain and neuropathic pain [41]. The activation of opioid receptors also leads to the release of endogenous opioids, such as endorphins, which further contribute to pain relief [42]. In addition to opioid receptors, other receptors in the spinal cord modulate pain. For example, the activation of GABA-A receptors by drugs like baclofen can inhibit pain signals [43]. The release of oxytocin in the spinal cord has also been implicated in pain relief, as it activates GABAergic inhibitory pathways [44]. The use of intrathecal therapy allows for the delivery of analgesic drugs directly to the site of pain perception, bypassing the blood-brain barrier and minimizing systemic side effects. This targeted approach can result in more effective pain relief with smaller doses of medication than systemic administration. Intrathecal therapy also provides continuous and stable delivery of medication, ensuring consistent pain relief [45].
It is important to note that the selection of the appropriate medication for intrathecal therapy depends on the type of pain being treated. Opioid drugs, such as morphine and hydromorphone, are commonly used for the management of cancer pain and neuropathic pain [46,47]. Other medications, such as baclofen and clonidine, may be used for the treatment of specific types of pain, such as central pain and neuropathic pain [48,49]. The combination of different medications, such as opioids and ziconotide, may also be used to enhance pain relief [50,51]. In conclusion, the mechanisms underlying pain relief with intrathecal therapy involve the activation of opioid receptors, modulation of other receptors in the spinal cord and the release of endogenous opioids. This approach allows for effective pain relief with smaller doses of medication and minimizes systemic side effects. The selection of the appropriate medication depends on the type of pain being treated. Further research is needed to better understand the mechanisms underlying pain relief with intrathecal therapy and to optimize its use in clinical practice.
Indications and patient selection
Patient selection is an essential aspect of intrathecal drug therapy. Appropriate patient selection is necessary to ensure the effectiveness of the treatment [52]. Guidelines have been published to aid in the selection of patients for intrathecal drug therapy. Discontinuation of intrathecal therapy may be undesirable in terminally ill cancer patients, as uncontrolled pain is likely to result [53]. The main indications for intrathecal drug therapy in chronic pain, both benign and cancer-related, include neuropathic pain, post herpetic neuralgia, peripheral neuropathy and mixed nociceptive-neuropathic pain syndromes [6]. It is also considered for the management of refractory cancer pain that has failed to respond to treatment with the World Health Organization (WHO) pain ladder [21].
Intrathecal drug therapy is generally considered for patients with non-neuropathic pain or widespread cancer pain, such as bone pain, axial spine pain and visceral pain. It may be an alternative to spinal cord stimulation for select patients [54]. Intrathecal drug delivery systems have been shown to provide effective pain relief for patients with difficult-to-control cancer pain, leading to sustained reductions in pain severity scores over a 6-month period [55]. The use of intrathecal therapy has expanded beyond cancer patients to chronic pain conditions. However, support for intrathecal drug administration is stronger for managing cancer pain than for noncancer pain [56]. It is known that intrathecal drug delivery systems can offer both survival benefits and pain reduction in patients with advanced cancer [57]. Intrathecal therapy has an established role in the management of refractory cancer pain [58].
Intrathecal therapy has advantages over systemic pharmacotherapy for cancer-related pain. By delivering opioids and other agents directly to the central nervous system, intrathecal drug administration can offer superior pain relief with less toxicity at a fraction of the systemic dose [59]. It provides pain relief with reduced systemic concerns, which is particularly important in patients with cancer-related pain who may already receive multiple systemic medications [60]. Intrathecal therapy is generally considered when other forms of pain management, such as oral or transdermal analgesics, provide insufficient pain relief or produce unacceptable side effects. It is important for patients to undergo multidisciplinary evaluation and drug trailing before considering intrathecal pump implantation.
Morphine and ziconotide are commonly used drugs for intrathecal analgesia in cancer patients [61]. Studies have shown that intrathecal morphine infusion therapy is effective in providing pain relief for cancer patients without causing serious complications. The median interval required to achieve cost equivalence for Intrathecal Morphine Infusion Therapy Pump Placement (IMITPP) was found to be 11.44 months, with shorter intervals observed for patients receiving very high doses or high doses of systemic opioids prior to IMITPP [21].
Drugs and medications
The drugs used in intrathecal drug delivery systems can vary depending on the specific condition being treated. For the treatment of bacterial and fungal infections in the central nervous system, intrathecal antibiotics such as aminoglycosides, colistin, daptomycin, tigecycline and vancomycin are commonly used. These antibiotics are essential for effective intrathecal therapy against bacterial and fungal infections [62]. Intrathecal opioid therapy is widely used for cancer-related and non-malignant pain. Opiates such as morphine, hydromorphone, fentanyl and sufentanil are commonly administered via intrathecal drug delivery systems for pain relief. These opioids have been shown to be effective in providing analgesia for various types of pain.
In addition to opioids, other medications commonly administered intrathecally include baclofen, a muscle relaxant used for spasticity treatment, local anesthetics for pain relief and adjuvant medications to enhance the effects of opioids and other analgesics. These medications are often used in combination to provide comprehensive pain management [63]. Ziconotide, a non-opioid analgesic, is another drug that can be administered intrathecally for chronic pain. It is a calcium channel blocker that acts on N-type calcium channels in the spinal cord to inhibit pain neurotransmitter release. Ziconotide has been shown to be effective in the management of severe chronic pain, particularly in patients unresponsive to other treatments [64].
Intrathecal gene therapy is an emerging field that holds promise for the treatment of various pain conditions. For example, intrathecal administration of adenoviral or adeno-associated viral vectors containing cDNA encoding Interleukin-10 (IL-10) has been shown to prevent and/or reverse mechanical allodynia induced by intrathecal administration of paclitaxel, an antineoplastic agent. This suggests that gene therapy targeting specific pain pathways in the spinal cord may provide a novel approach to pain management [65]. Local anesthetics, such as bupivacaine and ropivacaine, are commonly used for intrathecal administration and in intrathecal pumps for various medical procedures. Intrathecal administration involves the injection of medications directly into the spinal canal, providing localized anesthesia and pain relief. The addition of intrathecal opioids, such as fentanyl, to anesthetics has been shown to potentiate the effect of spinal anesthesia for intra-abdominal surgeries [66].
The use of intrathecal local anesthetics in combination with other drugs, such as opioids and adjuvants, has been shown to improve the quality and duration of sensory blockade. This has been shown to prolong postoperative analgesia. However, it is essential to consider the potential side effects and interactions of these combinations [67]. Studies have investigated the use of different combinations, including bupivacaine with fentanyl, dexmedetomidine, magnesium sulfate and clonidine [68,69].
Dosages, titration and considerations for continuous infusion
Dosages, titration and considerations for continuous infusion for intrathecal pump in cancer patients are important factors to ensure effective pain management and minimize adverse effects. Several studies provide insights into these aspects of intrathecal pump therapy. One study by Winkelmüller examined the long-term effects of continuous intrathecal opioid therapy in 120 patients with chronic, non-malignant pain syndromes. The study found that individualized dosages were necessary to achieve optimal pain relief while minimizing side effects. The mean morphine dosage initially administered was 2.7 mg/day, increasing to 4.7 mg/day after an average of 3.4 years; 64.3% of patients had a constant dosage, while 35.7% required an increase to more than 6 mg/day; tolerance developed in seven cases, with four patients managing it through "drug holidays" and three requiring pump system removal [70].
Another study by Lin et al. compared Intravenous Patient- Controlled Analgesia (IPCA) with continuous infusion plus rescue dose or bolus-only dose to conventional oral extended-release morphine for maintaining analgesia in patients with severe cancer pain [69]. The study found that individualized titration of opioid doses was necessary to achieve adequate pain control. Patients with persistent severe cancer pain were randomly assigned to three treatment arms: IPCA hydromorphone with a bolus-only dose, IPCA hydromorphone with continuous infusion and oral extendedrelease morphine. Arm B (oral morphine maintenance) resulted in higher pain scores and lower patient satisfaction compared to arms A1 and A2 (IPCA hydromorphone). IPCA hydromorphone without continuous infusion may require less opioid consumption and effectively control severe cancer pain after successful titration. Patients in the IPCA groups had better pain control and lower opioid consumption compared to the oral morphine group. IPCA hydromorphone without continuous infusion may be a more efficient option for pain management in severe cancer patients and no severe adverse events were reported in any of the treatment arms [71].
Bhatia et al. conducted a review on intrathecal drug delivery systems for cancer pain. The review emphasizes the importance of individualized dosing and titration to achieve optimal pain control [4]. Several studies reported that individualized dosing and careful titration are necessary for optimal pain relief and spasticity control in patients receiving intrathecal injections and continuous infusions of morphine and baclofen, respectively [72- 74]. In summary, the dosages, titration and considerations for continuous infusion for intrathecal pump in cancer patients require individualized approaches to achieve optimal pain control while minimizing adverse effects. Studies on intrathecal opioid therapy, intrathecal baclofen infusion and intrathecal drug delivery systems provide valuable insights into the dosing and titration strategies for managing cancer pain and spasticity. Individualized dosing, careful titration and infection prevention are significant considerations in the management of intrathecal pump therapy.
Surgical considerations and post-operative management
Implantation of an intrathecal drug delivery system involves several surgical considerations and requires post-operative management to ensure optimal outcomes. When implanting an intrathecal drug delivery system, it is imperative to consider the individual patient's pathology and the specific variables involved. The procedure outcomes can vary depending on these factors. Successful outcomes of intrathecal drug delivery systems depend on factors such as disseminated pain, pharmacokinetics, lipid solubility and catheter tip positioning. These factors vary among patients with different pathologies. Therefore, it is important to have a comprehensive understanding of the patient's condition and tailor the implantation technique accordingly [75].
There are different techniques for implanting intrathecal drug delivery systems. The choice of technique depends on various factors, such as the patient's anatomy, the type of medication being delivered and the desired outcomes. Continuous infusion techniques and intrathecal boluses are two commonly used methods for evaluating the effectiveness of the drug delivery system prior to implantation. These techniques allow for the assessment of the patient’s response to the medication and help determine the appropriate dosage and delivery method. Post-operative management plays an essential role in intrathecal drug delivery. Close monitoring of the patient's pain levels and response to medication is essential for optimal pain relief. Regular follow-up visits are necessary to assess the effectiveness of the drug delivery system and make any necessary adjustments to the medication dosage or delivery method [76].
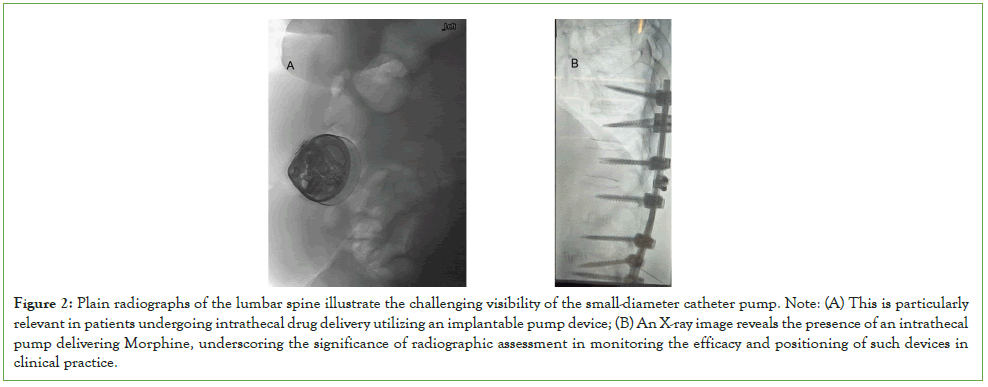
During the implantation procedure, it is imperative to ensure proper placement of the catheter and pump. This will optimize drug delivery and minimize complications risk. The Polyanalgesic Consensus Conference (PACC) provides recommendations for improving intrathecal drug delivery safety and reducing risks. These guidelines emphasize the importance of proper surgical technique, including accurate catheter placement and secure pump fixation. The choice of implantation technique should be tailored to the individual patient’s pathology. Close monitoring is necessary to ensure optimal pain relief and minimize complications. The PACC provides guidelines for improving the safety and efficacy of intrathecal drug delivery. Further research is needed to elucidate best practices for implantation and utilization (Figure 2) [77].
Figure 2: Plain radiographs of the lumbar spine illustrate the challenging visibility of the small-diameter catheter pump. Note: (A) This is particularly relevant in patients undergoing intrathecal drug delivery utilizing an implantable pump device; (B) An X-ray image reveals the presence of an intrathecal pump delivering Morphine, underscoring the significance of radiographic assessment in monitoring the efficacy and positioning of such devices in clinical practice.
Maintenance and refilling protocols
Maintenance and refilling protocols are essential for IDD system’s success and safety. The Polyanalgesic Consensus Conference (PACC) provides recommendations for improving safety and mitigating IDD risks. Routine inpatient monitoring after initiation of IDD therapy, catheter revision, or re-initiation of therapy is recommended to reduce the risk of mortality and other complications. Additionally, guidelines are provided for reducing morbidity and mortality in IDD [78]. There are various techniques and technologies that can aid in IDD system maintenance and refilling. For example, fluoroscopy and ultrasound can help identify the reservoir fill port for refilling. This study aimed to assess the accuracy of manually identifying the Reservoir Fill Port (RFP) for Intrathecal Drug Delivery Systems (IDDSs) with a raised RFP and compare it to previous data on IDDSs with a recessed RFP. The results showed that the identification accuracy of the raised RFP was lower than the clinically relevant difference in almost half of the instances. In addition, the number of attempts and procedural time were correlated with needle deviation [79,80]. Various techniques and technologies, such as fluoroscopy, ultrasound and virtual reality, can aid in the maintenance and refilling of IDD systems. However, it is important to be aware of potential complications and to implement strategies to minimize their risk.
Efficacy and outcomes
One systematic review and meta-analysis by Perruchoud et al. in 2023 evaluated cancer-related pain management with intrathecal drug delivery. The study included clinical studies that assessed intrathecal drug delivery systems for cancer pain. The authors found that intrathecal drug delivery was effective in pain relief for cancer patients. They also reported that morphine was the most commonly used drug in intrathecal drug delivery systems for cancer pain management [77]. Another systematic review and meta-analysis in 2023 by Duarte et al [78]. Focused on the effectiveness and safety of intrathecal drug delivery systems for cancer pain management. The study included clinical studies that evaluated intrathecal drug delivery systems in cancer patients. The authors concluded that intrathecal drug delivery systems were effective at reducing pain intensity and improving quality of life in cancer patients. They also reported that intrathecal drug delivery systems were generally safe, with a low incidence of adverse events [81].
In a critical review of refractory cancer pain and intrathecal therapy, the analysis focused on papers included in the systematic review that assessed the effectiveness and safety of intrathecal drug delivery systems for cancer pain management. The analysis of 21 studies showed a lack of proper assessment before implantation. This included optimistic interpretation of outcomes, poor consideration of complications and inclusion of patients with short survival. In this critical review, the indication of intrathecal therapy for patients unresponsive to multiple therapies has been disregarded, potentially discouraging its use in a selective population. These findings highlight the need for a more moderate palliative care approach, considering patient survival and opioid expertise before recommending spinal therapy [82]. In addition to systematic reviews and cohort studies, there are case reports and case series. These reports provide information into intrathecal therapy for cancer-related pain. For example, Tashiro et al. reported a case of successful intrathecal neurolytic block for cancer pain in a 10-year-old child. The case report demonstrated the effectiveness of intrathecal neurolytic block in neuropathic cancer pain [80].
An observational study evaluated the effects of an intrathecal drug delivery system connected to a subcutaneous port on pain, mood and quality of life in end-stage cancer patients. The study found that intrathecal combination therapy delivered by an intrathecal drug delivery system with a subcutaneous port could effectively control cancer-related symptoms, including pain, depression, anxiety and sleep disturbance [83,84]. Intrathecal therapy can be delivered using different medications, including opioids and other analgesics. Morphine administered intrathecally has been shown to be effective in treating postoperative pain following large joint arthroplasties. This study compared the effectiveness of intrathecal morphine (ITM) and single-shot femoral nerve block (SSFNB) in managing postoperative pain after knee replacement surgery. The total morphine dose and pain management effectiveness were similar in both groups. However, patients treated with SSFNB had a lower incidence of nausea and pruritus. Intrathecal morphine is effective for pain management after knee replacement surgery. However, it has a higher risk of side effects such as nausea and pruritus than a femoral nerve block [85].
Cost-effectiveness and implications for healthcare systems
In terms of cost-effectiveness, intrathecal therapy has been shown to be a cost-effective method for treating chronic nonmalignant pain caused by failed back syndrome [4]. However, more research is needed to evaluate the cost-effectiveness of Intrathecal Morphine Infusion Therapy via a Percutaneous Port (IMITPP) for refractory cancer pain. Intrathecal morphine infusion therapy via a percutaneous port has been used widely for its relatively low initial cost and has been shown to provide effective cancer pain management without causing serious complications. However, there is limited knowledge about this therapy and additional research is needed to evaluate its efficacy and safety [21]. Intrathecal analgesia is increasingly accepted as an alternative to medical management for moderate-to-severe cancer pain, with the availability of a wide variety of pharmacological agents allowing for individualized treatment regimens that provide effective analgesia with potentially fewer adverse effects than traditional opioid-based therapies [86]. In terms of cost-effectiveness, ITDD has been shown to be most costeffective for cancer patients between 3 and 6 months. Although the initial cost of ITDD is higher, maintenance costs over time are significantly lower than conventional routes of administration. Cost analyses have concluded that ITDD is the most cost-effective route of opioid administration for patients who require long-term management of cancer pain [23].
Safety and adverse effects
Serious complications associated with intrathecal catheters used in cancer pain patients are rare and the potential benefits of intrathecal catheters likely outweigh the potential for serious complications. However, there is a risk of infection associated with intrathecal drug delivery systems and the incidence of infectious complications varies [87]. However, the overall rate of infectious complications following implantation of ITDD systems in cancer patients is relatively low. Infections at the implantable pulse generator or pump pocket site are the most common infectious complications. It is important to carefully monitor and manage infectious complications associated with intrathecal drug delivery systems, as they can occur [88]. While ITDD systems offer a relatively safe and effective mechanism of drug delivery, there are still challenges and areas for improvement. Optimization and utilization of ITDD techniques still lag behind other modalities for pain control.
Variability in surgical technique, medication usage and education may contribute to this lag. Further research is needed to elucidate current and best practices for ITDD system trials, implantations and utilization [89]. While intrathecal drug delivery systems have shown promise in cancer-related pain management, it is important to consider potential complications and side effects. Chung reported a case of epidural granuloma following intrathecal pump implantation. This highlighted the need for careful monitoring and management of IDDS patients. However, overall, the literature suggests that IDDS is a valuable treatment option for cancer-related pain, with potential benefits for patients and healthcare systems [90].
Common side effects: respiratory depression, pruritus and urinary retention, etc.,
One of the main advantages of intrathecal therapy is the reduction in systemic side effects compared to systemic administration of medications. When medications are administered systemically, they circulate throughout the body and can cause side effects in various organs and systems. However, with intrathecal therapy, the medications act locally in the spinal fluid, resulting in a lower systemic exposure and a decreased risk of systemic side effects. Several studies have investigated the side effects of intrathecal therapy, particularly with the use of intrathecal opioids such as morphine. These studies have reported that the most common side effects of intrathecal opioids include nausea, vomiting, pruritus (itching), urinary retention and respiratory depression [91,92]. However, it is important to note that the incidence and severity of these side effects can vary depending on the specific medication, dose and patient population.
In a meta-analysis of randomized controlled studies, found that intrathecal morphine was associated with a mild increase in side effects compared to placebo. However, they also noted that with a dose of less than 0.3 mg, there were no more episodes of respiratory depression than in placebo patients who received systemic opioid analgesia [93]. It is worth mentioning that while intrathecal therapy can minimize systemic side effects, it is not without its own potential complications. Some of the complications associated with intrathecal therapy include infection, catheter-related issues, pump malfunction and neurological complications. These complications can occur due to various factors, including the invasive nature of the procedure and the long-term use of intrathecal devices [94- 97]. The effectiveness of IDDS can be affected by various factors. One study found that corrosion of the implanted drug delivery system can lead to loss of effectiveness. Corrosion at the pumpcatheter connection site is a rare cause of morphine leakage from IDDS implants and if IDDS therapy becomes ineffective, pump and catheter malfunction should be investigated, especially with a suture-less pump connection [98].
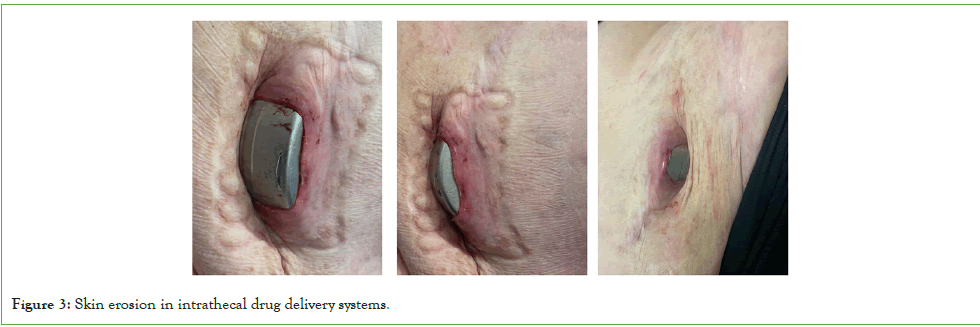
Catheter tip granulomas
Intrathecal drug delivery is an effective method for treating intractable pain, but it can lead to the development of Intrathecal Catheter Tip Granuloma (ICTG), particularly in patients receiving high doses or concentrations of intrathecal drug infusions; various factors contribute to ICTG formation, but no specific patient factors have been identified. Catheter tip granulomas are a rare but serious complication of intrathecal drug delivery systems, which can lead to devastating consequences [99]. Continuous intrathecal infusion of opioids for chronic pain and spasticity can lead to the formation of inflammatory masses at the catheter tip, causing neurological complications. The polyanalgesic consensus conference provides recommendations for the prevention, diagnosis and management of intrathecal granulomas based on literature analysis and clinical experience. It is significant to consider the prevention, early detection and successful treatment of intraspinal granulomas when offering intrathecal drug therapy to patients with chronic intractable pain [100]. The benefits of intrathecal therapy must be weighed against the risks of internal pump and catheter placement [101]. Catheter tip granulomas are a rare but potentially devastating complication of intrathecal drug delivery systems, associated with various medications used in intrathecal therapy. The formation of these granulomas can lead to symptoms of spinal cord compression and reduced therapeutic effects, emphasizing the importance of careful monitoring and management of intrathecal therapy. Complications such as skin erosion can arise due to the use of intrathecal drug delivery systems, leading to the need for pump relocation and resolution of associated problems [102].
Intrathecal pump site erosion
There are potential complications associated with these systems, such as skin erosion, which can lead to a loss of effectiveness. There have been instances where skin erosion necessitated the relocation of the pump to resolve the issue (Figure 3) [103].
Figure 3: Skin erosion in intrathecal drug delivery systems.
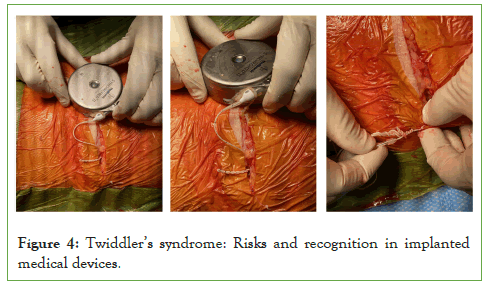
Twiddler's syndrome
Twiddler's syndrome, a rare but serious complication of implanted medical devices, involves the spontaneous or deliberate manipulation of the device by the patient, leading to hardware malfunction. This syndrome has been reported in various medical contexts, including cardiac pacemakers, deep brain stimulation devices and spinal cord stimulators. The manipulation of the implanted device can result in lead dislodgment, coiling of catheters and rotation of the pulse generator, ultimately causing device malfunction. It is important for healthcare providers to be aware of this syndrome and its potential complications, as early recognition and appropriate management are crucial in preventing adverse outcomes for patients with implanted medical devices (Figure 4).
Figure 4: Twiddler’s syndrome: Risks and recognition in implanted medical devices.
Intrathecal drug therapy and respiratory depression for cancer pain patient
One of the main concerns with intrathecal drug therapy, particularly when opioids such as morphine are used, is the risk of respiratory depression. Respiratory depression is a potentially serious side effect of intrathecal morphine administration. Studies have reported varying incidence rates of respiratory depression in patients receiving intrathecal morphine. However, it is important to note that the incidence of respiratory depression may vary depending on the dose of intrathecal morphine administered. With a dose of less than 0.3 mg, there were no more episodes of respiratory depression than in placebo patients who received systemic opioid analgesia.
The incidence of these side effects may also vary depending on the dose of intrathecal morphine administered. They reported that a higher dose of intrathecal morphine resulted in an increased risk of pruritus, but not nausea or vomiting. It is worth noting that the side effects of intrathecal morphine may be dose-dependent and higher doses may increase the risk of side effects. In some cases, the use of a low-dose naloxone infusion has been investigated as a potential strategy to reduce the incidence of respiratory depression without compromising pain control. However, it is important to consider the potential impact of naloxone on pain scores, as one study found that maximum pain scores were greater in patients who received a low-dose naloxone infusion.
There are indications that intrathecal use of opioids, including morphine, may lead to neurotoxicity in both animals and humans. Neurotoxicity has been observed in both animals and humans and physicians should carefully consider the potential risks and benefits of intrathecal drug therapy.
Recent advances in drug discovery for intrathecal therapy
Intrathecal drug delivery is increasingly used in cancer pain management. It has been associated with improved pain reporting, reduced opioid requirements and enhanced pain management in patients with refractory cancer pain. Furthermore, intrathecal targeted drug delivery techniques, such as gadolinium-based MR cisternography, have been developed to evaluate the distribution pattern of intrathecal drugs in pain management, specifically for orofacial cancer pain. Gadolinium-based MR cisternography is used for clinical evaluation of cerebrospinal fluid leaking and intrathecal targeted drug delivery. A case study showed successful attenuation of severe orofacial pain using prepontine cisternal analgesic agents’ administration. A postoperative MRI image revealed that intrathecal drugs were distributed around the catheter tip and concentrated on the sides of the catheter. Another innovation is the development of programmable pumps for intrathecal morphine delivery to the cisterna magna. This approach has been shown to be effective in treating refractory cancer pain above the middle thoracic vertebrae level. By delivering morphine directly to the cisterna magna, this system provides targeted pain relief and can be adjusted to meet individual patient needs.
Discussion
In addition to its role in pain management, IDDS has also been examined for drug delivery to the brain. The Cerebrospinal Fluid (CSF) has been identified as a potential route for delivering biological therapies to the brain, including antibodies, nucleic acidbased therapeutics and gene therapy. This approach could have implications for brain tumours and other neurological conditions.
There is evidence to suggest that IDDS can impact the place of care for patients with cancer-related pain. A service evaluation study found that IDDS allowed patients to spend more time in community settings, reducing hospital admissions. This finding highlights the potential of IDDS to improve patient access to care by enabling treatment in a more convenient and comfortable environment. Patients with advanced cancer who received intrathecal analgesia had more time in the community and lower morphine doses at the end of life compared to those receiving medical management, suggesting that the initial inpatient investment may be beneficial.
Case study 1: Complex pain management in a patient with metastatic melanoma and Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) with intrathecal pump
This case report details the comprehensive palliative care provided to patient, a 72-year-old male with metastatic melanoma, CIDP and complex neuropathic and chest pain. The patient underwent a thorough medical history review, revealing an extensive list of comorbidities and medications. Pain management included the use of a syringe driver pump delivering Hydromorphone and Haloperidol. The report also discusses the patient's candidacy for an Intra-Thecal Pump (ITP) implant, emphasizing the need for careful consideration of risks in light of the complex medical background. This case report examines into the difficult management of chronic pain in a patient utilizing the SynchroMed™ II intrathecal pump. The report details the patient's device information, reservoir status, drug settings, infusion details, myPTM™ (Personal Therapy Manager) setup and alarm settings.
Clinical consultations, including nurse consultations and patient reviews, are outlined, highlighting adjustments in medication, management of side effects and successful outcomes, such as improved pain scores and enhanced quality of life. The report discusses adjustments in doses, procedures performed and outcomes during several consultations. The patient's history, presenting problems, diagnoses, treatments and plans are meticulously documented, showcasing the multidisciplinary approach to addressing complex pain issues. This case report highlights the comprehensive care provided, including diagnostic blocks, therapeutic injections, dose adjustments and the collaborative efforts of clinicians. The SynchroMed™ II intrathecal pump is a valuable tool in managing chronic pain. This case report explores the utilization of this device in a patient, presenting device information, treatment settings and clinical consultations.
Male patient presented with multi-site global pain, primarily stemming from bilateral arms, legs, neck, groin and severe chest pain related to metastatic melanoma and CIDP. The patient's complex medical history included autoimmune diseases, Deep Vein Thrombosis (DVT) and recent diagnoses such as constipation, insomnia and neuropathic pain. The patient’s past medical history revealed autoimmune diseases, DVT, metastatic melanoma and paraneoplastic syndrome. Documented symptoms included constipation, insomnia, nausea, neuropathic pain, diabetes, angina and gastro-oesophageal reflux disease. The patient had a history of agitation and was under palliative care. The extensive medication list included apixaban, betamethasone valerate, coloxyl with senna, frusemide, haloperidol, hydromorphone, levothyroxine, lyrica, macrogol, nexium, normacol plus, novomix 30 flexpen, nystatin, panadol osteo, prednisone, rivotril and spiractin.
During the consultation, Patient presented with complaints of nausea, loss of taste and smell and global pain affecting various body parts. Notably, the patient had been given a prognosis of 3-4 months to live and internal bleeding in the sinuses was identified. Given the patient's extensive medical history and complex pain presentation, a syringe driver pump delivering Hydromorphone and Haloperidol was initiated. Further, considering the patient’s Intra-Thecal Pump (ITP) candidacy, a detailed discussion regarding the procedure, associated risks and consent took place. The patient was advised to discontinue Eliquis 3-4 days before the scheduled procedure. The reservoir volume was 40.0 mL and the low reservoir alarm was set at 2.0 mL. The primary drug administered was Hydromorphone (1,000.0 mcg/mL), with secondary drugs including Ropivacaine (2,500.0 mcg/mL) and Clonidine (75.0 mcg/mL). The infusion was set to a minimum rate (6 mcL/day) and specific infusion details were provided based on a 24-hour schedule.
The patient reported notable improvements, including reduced pain levels, enhanced activity participation and successful adjustments to the intrathecal pump settings. The patient’s intrathecal pump dose was increased to 400 mcg and myPTM™ settings were adjusted for optimal pain control. Detailed nurse consultations, highlighted adjustments in continuous Hydromorphone dosage, myPTM™ setup, management of side effects and wound care. Patient reported improved pain, especially in the neck and bowel movements. However, he still experienced left-sided pain and occasional severe pain leading to nausea. The therapeutic block showed positive outcomes, allowing consideration for an RFA procedure. The intrathecal pump dose was increased to 600 mcg per 24 hours, with adjustments to MyPTM boluses. A nurse consultation highlighted Patient's positive response to the increased dose. The intrathecal pump was refilled and the background dose was further increased to 700 mcg/24hr. MyPTM remained at 30 mcg with a maximum of 7 doses per 24 hours. This case report highlights the intricate pain management required for a patient with metastatic melanoma, CIDP and various comorbidities. The utilization of a syringe driver pump and consideration of an intra-thecal pump exemplify the complexity of palliative care in such cases. Close collaboration between healthcare providers are necessary for ensuring comprehensive and patient-centered care. This case illustrates the successful utilization of the SynchroMed™ II intrathecal pump in managing chronic pain. The meticulous adjustment of settings, thorough clinical consultations and positive patient outcomes highlight the significance of intrathecal pumps in optimizing pain management and improving the overall quality of life for patients with chronic pain conditions.
During treatment session, Patient reported a new-onset severe pain in the right parieto-temporal region of his head. The pain, diagnosed as arthritis in the C1/2 joint, was not responding to the current treatment. The patient continued to participate in golf and a therapeutic block of C1/C2 with Lignocaine was performed. The successful block paved the way for potential Radiofrequency Ablation (RFA) of C0/1 and C1/2 joints for longer therapeutic relief. The integration of diagnostic blocks, therapeutic interventions and meticulous dose adjustments using the SynchroMed™ II intrathecal pump has contributed to significant improvements in pain control and overall quality of life for Mr. Patient. The collaborative efforts among clinicians and the utilization of advanced pain management techniques showcase the effectiveness of a multimodal approach in addressing complex pain scenarios.
Case study 2: Intrathecal morphine infusion for intractable pain in metastatic colon carcinoma
A 43-year-old female presented with a past history of metastatic colon carcinoma and intractable pain. She was referred for a pain pump consult while currently managing her pain with Hydromorphone 4.0mg every 2 hours prn, Diazepam 1.0 mg every 8 hours as needed, Fentanyl patch 75 mcg (2 patches every 72 hours) and Naproxen 550 mg twice daily. The patient’s pain had become refractory to the current regimen, necessitating the consideration of continuous Intravenous (IV) infusion of Hydromorphone. Her life expectancy was estimated to be 6 months to 1 year. To assess the adequacy of pain relief, an Intrathecal (IT) trial of morphine (200 mcg) was initiated. If the trial proved effective, a permanent IT catheter and pump would be placed. The patient experienced greater than 90% pain relief during the IT Morphine trial. Subsequently, she underwent a successful SynchroMed II pump placement one week later. With the targeted drug delivery system in place, the patient maintained excellent pain relief. Medication titrations were performed intermittently, optimizing her pain management. Unfortunately, the patient succumbed to her metastatic cancer one year later.
In this case, the utilization of intrathecal drug delivery played a major role in the treatment algorithm for managing cancer-related pain. The successful IT morphine trial and subsequent SynchroMed II pump placement provided effective pain relief, allowing the patient to maintain a satisfactory quality of life until the progression of her metastatic disease. This case underscores the significance of individualized pain management strategies, particularly in the context of metastatic colon carcinoma with intractable pain.
Case study 3: Intrathecal morphine infusion for enhanced functionality in breast cancer patient with spinal metastases
A 52-year-old retired ballerina, previously diagnosed with breast cancer, presented with newly diagnosed polyostotic metastases involving the spine and pelvis. Despite being extremely independent, the patient was limited by severe pain. The initial analgesic regimen included a Duragesic patch (75 mcg), oral morphine sulfate exceeding 60 mg per day and Oxycodone 20 mg PRN every four hours, totaling more than 200 mg morphine equivalent. The patient complained of decreased activity, mental clouding and constipation. Despite the aggressive analgesic approach, the patient continued to report a Visual Analog Scale (VAS) score greater than 8, increasing Oswestry Disability Index (ODI) and a decreasing performance status.
To address the refractory pain, the patient underwent a continuous infusion trial. The pain log revealed 100% pain relief for 4 hours and effective pain relief for over 10 hours without the need for additional pain medications. Consequently, the patient was scheduled for an Intrathecal (IT) pump implant. Upon initiation of therapy, the patient started with 0.4 mg/day and before discharge, the dose was increased to 0.6 mg/day. At the one-week post-op visit, the patient was titrated up to 0.7 mg/day using patient-controlled analgesia with myPTM (personalized therapy manager). The dose included 0.1 mg every 6 hours with 4 boluses available per day.
The patient continued to respond well to the therapy and was further titrated up to 1.0 mg/day with 0.2 mg myPTM boluses every 4 hours, allowing a maximum of 6 boluses per day. Remarkably, the patient experienced significant improvement, returning to teaching, hiking and even shoveling her driveway. Importantly, the patient remained alive and functional one year later. This case highlights the successful application of intrathecal morphine infusion in a breast cancer patient with spinal metastases, achieving substantial pain relief and restoring the patient's ability to engage in daily activities. The personalized titration with myPTM played a significant role in optimizing the dosage and maintaining the patient's quality of life over an extended period.
Conclusion
Intrathecal drug delivery has emerged as a modality in managing complex cancer-related pain, offering significant advantages over conventional systemic therapies. This review demonstrates the clinical efficacy of intrathecal therapy in improving pain control, functionality and overall quality of life for patients with refractory cancer pain. The localized drug delivery mechanism minimizes systemic side effects while providing precise and targeted analgesia.
The pharmacokinetics and pharmacodynamics of intrathecal drugs, such as opioids, ziconotide and baclofen, highlight their ability to effectively manage chronic and cancer-related pain through the activation of specific receptors in the central nervous system, including opioid, GABA-A and oxytocin receptors. The efficacy of this method is further enhanced by the use of continuous infusion systems that allow for consistent pain relief with lower doses of medication compared to systemic administration. Appropriate patient selection, guided by established clinical guidelines, is essential for the success of intrathecal therapy. It is particularly indicated for patients with refractory cancer pain, neuropathic pain and other difficult-to-control pain conditions. Intrathecal drug delivery systems have proven to provide significant pain relief for cancer patients, offering advantages over traditional systemic medications by reducing toxicity and improving quality of life. Medications used in intrathecal therapy, including opioids, muscle relaxants, local anesthetics and emerging options such as gene therapy, allow for tailored treatment based on the specific pain type and patient needs.
Surgical considerations and post-operative management are critical to the success of intrathecal drug delivery systems. The implantation procedure requires careful consideration of the patient's individual pathology and the selection of the appropriate technique, such as continuous infusion or bolus methods. Postoperative management, including careful monitoring of pain relief and medication response, ensures the optimization of therapeutic outcomes. Further research into the pharmacokinetics, pharmacodynamics and optimization of medication selection and dosing will continue to enhance the clinical application of intrathecal drug delivery systems in managing chronic and refractory pain conditions. Despite its potential, barriers to wider adoption, including cost, accessibility and procedural expertise, needs to be addressed through multidisciplinary collaboration, patient education and policy advocacy.
Case studies presented in this review demonstrate the versatility and therapeutic value of Intrathecal Drug Delivery Systems (IDDS), highlighting improved patient outcomes, including reduced opioid dependency, enhanced activity levels and a shift toward communitybased care. By integrating advanced technologies and a personalized approach, intrathecal therapy has the potential to redefine pain management methods, particularly in advanced cancer care. Future research should focus on expanding the evidence base, investigating novel drug formulations and addressing implementation challenges to maximize the reach and impact of this promising intervention.
Declarations
• The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
• The authors declare the following financial interests/personal relationships which may be considered as potential competing interests.
References
- Maino P, van Kuijk SM, Koetsier E. Refill port identification of intrathecal drug delivery system devices with a raised fill port. Pain Pract. 2019;19(4):418-425.
[Crossref] [Google Scholar] [PubMed]
- Erdine S, De Andres J. Drug delivery systems. Pain Pract. 2006;6(1):51-57.
[Crossref] [Google Scholar] [PubMed]
- Warner L, Branstad A, Hunter Guevara L, Matzke Bitterman L, Pingree M, Nicholson W, et al. Malfunctioning sufentanil intrathecal pain pump: A case report. J Med Case Rep. 2020;14(1):1-4.
[Crossref] [Google Scholar] [PubMed]
- Bhatia G, Lau ME, Koury KM, Gulur P. Intrathecal Drug Delivery (ITDD) systems for cancer pain. F1000Res. 2014;2:96.
[Crossref] [Google Scholar] [PubMed]
- Roberts LJ, Finch PM, Goucke CR, Price LM. Outcome of intrathecal opioids in chronic non-cancer pain. Eur J Pain. 2001;5(4):353-361.
[Crossref] [Google Scholar] [PubMed]
- Ver Donck A, Vranken JH, Puylaert M, Hayek S, Mekhail N, Van Zundert J. Intrathecal drug administration in chronic pain syndromes. Pain Prac. 2014;14(5):461-476.
[Crossref] [Google Scholar] [PubMed]
- Lozano ML, Rivera J, Sanchez-Guiu I, Vicente V. Towards the targeted management of Chediak-Higashi syndrome. Orphanet J Rare Dis. 2014;9:1-132.
[Crossref] [Google Scholar] [PubMed]
- Lin CC, Lai YL, Ward SE. Effect of cancer pain on performance status, mood states and level of hope among Taiwanese cancer patients. J Pain Symptom Manage. 2003;25(1):29-37.
[Crossref] [Google Scholar] [PubMed]
- Fisch MJ, Lee JW, Weiss M, Wagner LI, Chang VT, Cella D, et al. Prospective, observational study of pain and analgesic prescribing in medical oncology outpatients with breast, colorectal, lung or prostate cancer. J Clin Oncol. 2012;30(16):1980-1988.
[Crossref] [Google Scholar] [PubMed]
- Powles T, Albiges L, Bex A, Grunwald V, Porta C, Procopio G, et al. ESMO clinical practice guideline update on the use of immunotherapy in early stage and advanced renal cell carcinoma. Ann Oncol. 2021;32(12):1511-9.
[Crossref] [Google Scholar] [PubMed]
- Jost L, Roila F, ESMO Guidelines Working Group. Management of cancer pain: ESMO clinical practice guidelines. Ann Oncol. 2010;21:v257-v2360.
[Crossref] [Google Scholar] [PubMed]
- Bennett MI, Eisenberg E, Ahmedzai SH, Bhaskar A, O’Brien T, Mercadante S, et al. Standards for the management of cancerâ?related pain across Europe-a position paper from the EFIC task force on cancer pain. Eur J Pain. 2019;23(4):660-668.
[Crossref] [Google Scholar] [PubMed]
- Ibrahim HD, Khraim F, Al-Tawafsheh A. Adult cancer patient’s barriers toward pain management: A literature review. J Nurs Educ Pract. 2020;10(12):38.
- Yamanaka M. A concept analysis of self-management of cancer pain. Asia Pac J Oncol Nurs. 2018;5(3):254-261.
[Crossref] [Google Scholar] [PubMed]
- Wada N, Handa S, Yamamoto H, Higuchi H, Okamoto K, Sasaki T, et al. Integrating cancer patient’s satisfaction with rescue medication in pain assessments. The Showa University Journal of Medical Sciences. 2020;32(3):181-191.
- Al-Atiyyat N. Knowledge, perceived barriers and practices of oncology nurses regarding cancer pain management. Indian J Palliat Care. 2022;19(6):1-9.
[Crossref] [Google Scholar] [PubMed]
- O'Connor L, Hassett A, Sheridan N. Pain assessment and registration in medical oncology clinics: Operationalized through the lens of health care professionals and patients. HRB Open Res. 2021;4:86.
[Crossref] [Google Scholar] [PubMed]
- Carvajal G. Pancreatic cancer related pain: Review of pathophysiology and intrathecal drug delivery systems for pain management. Pain Physician. 2021;24(5):E583.
[Google Scholar] [PubMed]
- Mitchell A, McGhie J, Owen M, McGinn G. Audit of intrathecal drug delivery for patients with difficult-to-control cancer pain shows a sustained reduction in pain severity scores over a 6-month period. Palliat Med. 2015;29(6):554-563.
[Crossref] [Google Scholar] [PubMed]
- Vissers KC, Besse K, Wagemans M, Zuurmond W, Giezeman MJ, Lataster A, et al. Pain in patients with cancer. Evidenceâ?Based Interventional Pain Medicine: According to Clinical Diagnoses. 2011:173-90.
[Crossref] [Google Scholar] [PubMed]
- Qin W, Li Y, Liu B, Liu Y, Zhang Y, Zhang X, et al. Intrathecal morphine infusion therapy via a percutaneous port for refractory cancer pain in China: An efficacy, safety and cost utilization analysis. J Pain Res. 2020:231-7.
[Crossref] [Google Scholar] [PubMed]
- Kim JH, Jung JY, Cho MS. Continuous intrathecal morphine administration for cancer pain management using an intrathecal catheter connected to a subcutaneous injection port: A retrospective analysis of 22 terminal cancer patients in Korean population. Korean J Pain. 2013;26(1):32-38.
[Crossref] [Google Scholar] [PubMed]
- Bottros MM, Christo PJ. Current perspectives on intrathecal drug delivery. J Pain Res. 2014:615-626.
[Crossref] [Google Scholar] [PubMed]
- Harbaugh RE, Shaffrey C, Couldwell WT, Berger MS. 49 Intrathecal Baclofen Therapy. In: Neurosurgery Knowledge Update. Georg Thieme Verlag; 2015.
- Miele VJ, Price KO, Bloomfield S, Hogg J, Bailes JE. A review of intrathecal morphine therapy related granulomas. Eur J Pain. 2006;10(3):251-261.
[Crossref] [Google Scholar] [PubMed]
- Pope JE, Deer TR. Intrathecal pharmacology update: Novel dosing strategy for intrathecal monotherapy ziconotide on efficacy and sustainability. Neuromodulation: Technology at the Neural Interface. 2015;18(5):414-420.
[Crossref] [Google Scholar] [PubMed]
- Oyekunle A, Haferlach T, Kroger N, Klyuchnikov E, Zander AR, Schnittger S, et al. Molecular diagnostics, targeted therapy and the indication for allogeneic stem cell transplantation in acute lymphoblastic leukemia. Adv Hematol. 2011;2011(1):154745.
[Crossref] [Google Scholar] [PubMed]
- Bleyer WA, Coccia PF, Sather HN, Level C, Lukens J, Niebrugge DJ, et al. Reduction in central nervous system leukemia with a pharmacokinetically derived intrathecal methotrexate dosage regimen. J Clin Oncol. 1983;1(5):317-325.
[Crossref] [Google Scholar] [PubMed]
- Blaney SM, Poplack DG. Pharmacologic strategies for the treatment of meningeal malignancy. Invest New Drugs. 1996;14:69-85.
[Crossref] [Google Scholar] [PubMed]
- Bennett G, Deer T, Du Pen S, Rauck R, Yaksh T, Hassenbusch SJ. Future directions in the management of pain by intraspinal drug delivery. J Pain Symptom Manage. 2000;20(2):S44-S50.
[Crossref] [Google Scholar] [PubMed]
- Hassenbusch SJ, Portenoy RK, Cousins M, Buchser E, Deer TR, Du Pen SL, et al. Polyanalgesic consensus conference 2003: An update on the management of pain by intraspinal drug delivery-report of an expert panel. J Pain Symptom Manage. 2004;27(6):540-563.
[Crossref] [Google Scholar] [PubMed]
- Iliff JJ, Lee H, Yu M, Feng T, Logan J, Nedergaard M, et al. Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J Clin Invest. 2013;123(3):1299-1309.
[Crossref] [Google Scholar] [PubMed]
- Rasmussen MK, Mestre H, Nedergaard M. The glymphatic pathway in neurological disorders. Lancet Neurol. 2018;17(11):1016-1024.
[Crossref] [Google Scholar] [PubMed]
- Rizvi T, Wintermark M, Schiff D. Imaging of epidural spinal cord compression. In Handbook of Neuro-Oncology Neuroimaging 2016:pp. 723-744.
- Xiao F, Drzymalski D, Liu L, Zhang Y, Wang L, Chen X. Comparison of the ED50 and ED95 of intrathecal bupivacaine in parturients undergoing cesarean delivery with or without prophylactic phenylephrine infusion: A prospective, double-blind study. Reg Anesth Pain Med. 2018;43(8):885-889.
[Crossref] [Google Scholar] [PubMed]
- Moreno B, Barbosa J. Ultrasound-guided procedures in the cervical spine. Cureus. 2021;13(12):e20361.
[Crossref] [Google Scholar] [PubMed]
- Simsek H, Zorlu E, Bakal O, Akarsu S, Guney SM. Continuous intrathecal baclofen delivery in severely disabling spasticity. Vojnosanit Pregl. 2018;75(11):1076-1082.
- Wolf DA, Hesterman JY, Sullivan JM, Orcutt KD, Silva MD, Lobo M, et al. Dynamic dual-isotope molecular imaging elucidates principles for optimizing intrathecal drug delivery. JCI insight. 2016;1(2):e85311.
[Crossref] [Google Scholar] [PubMed]
- Paris J, Angeli E, Bousquet G. The Pharmacology of xenobiotics after intracerebro spinal fluid administration: Implications for the treatment of brain tumors. Int J Mol Sci. 2021;22(3):1281.
[Crossref] [Google Scholar] [PubMed]
- Calias P, Banks WA, Begley D, Scarpa M, Dickson P. Intrathecal delivery of protein therapeutics to the brain: A critical reassessment. Pharmacol Ther. 2014;144(2):114-122.
[Crossref] [Google Scholar] [PubMed]
- Hassenbusch SJ, Stanton-Hicks M, Covington EC, Walsh JG, Guthrey DS. Long-term intraspinal infusions of opioids in the treatment of neuropathic pain. J Pain Symptom Manage. 1995;10(7):527-543.
[Crossref] [Google Scholar] [PubMed]
- Vissers KC, Besse K, Hans G, Devulder J, Morlion B. Opioid rotation in the management of chronic pain: Where is the evidence? Pain Pract. 2010;10(2):85-93.
[Crossref] [Google Scholar] [PubMed]
- Slonimski M, Abram SE, Zuniga RE. Intrathecal baclofen in pain management. Reg Anesth Pain Med. 2004;29(3):269-276.
[Crossref] [Google Scholar] [PubMed]
- Juif PE, Breton JD, Rajalu M, Charlet A, Goumon Y, Poisbeau P. Long-lasting spinal oxytocin analgesia is ensured by the stimulation of allopregnanolone synthesis which potentiates GABAA receptor-mediated synaptic inhibition. J Neurosci. 2013;33(42):16617-16626.
[Crossref] [Google Scholar] [PubMed]
- Smith TJ, Coyne PJ, Smith WR, Roberts JD, Smith V. Use of an implantable drug delivery system for refractory chronic sickle cell pain. Am J Hematol. 2005;78(2):153-154.
[Crossref] [Google Scholar] [PubMed]
- Anderson VC, Cooke B, Burchiel KJ. Intrathecal hydromorphone for chronic nonmalignant pain: A retrospective study. Pain Med. 2001;2(4):287-297.
[Crossref] [Google Scholar] [PubMed]
- de la Calle Gil AB, Pena Vergara I, Cormane Bornacelly MA, Pajuelo Gallego A. Intrathecal ziconotide and morphine for pain relief: A case series of eight patients with refractory cancer pain, including five cases of neuropathic pain. Neurol Ther. 2015;4(2):159-168.
[Crossref] [Google Scholar] [PubMed]
- Ackerman LL, Follett KA, Rosenquist RW. Long-term outcomes during treatment of chronic pain with intrathecal clonidine or clonidine/opioid combinations. J Pain Symptom Manage. 2003;26(1):668-677.
[Crossref] [Google Scholar] [PubMed]
- Webster LR, Fakata KL, Charapata S, Fisher R, MineHart M. Open-label, multicenter study of combined intrathecal morphine and ziconotide: Addition of morphine in patients receiving ziconotide for severe chronic pain. Pain Med. 2008;9(3):282-290.
[Crossref] [Google Scholar] [PubMed]
- Wallace MS, Kosek PS, Staats P, Fisher R, Schultz DM, Leong M. Phase II, open-label, multicenter study of combined intrathecal morphine and ziconotide: Addition of ziconotide in patients receiving intrathecal morphine for severe chronic pain. Pain Med. 2008;9(3):271-281.
[Crossref] [Google Scholar] [PubMed]
- Brogan SE, Winter NB. Patient-controlled intrathecal analgesia for the management of breakthrough cancer pain: A retrospective review and commentary. Pain Med. 2011;12(12):1758-1768.
[Crossref] [Google Scholar] [PubMed]
- Ghafoor VL, Epshteyn M, Carlson GH, Terhaar DM, Charry O, Phelps PK. Intrathecal drug therapy for long-term pain management. Am J Health Syst Pharm. 2007;64(23):2447-2461.
[Crossref] [Google Scholar] [PubMed]
- Pope JE, Deer TR, Bruel BM, Falowski S. Clinical uses of intrathecal therapy and its placement in the pain care algorithm. Pain Pract. 2016;16(8):1092-1106.
[Crossref] [Google Scholar] [PubMed]
- Mitchell A, McGhie J, Owen M, McGinn G. Audit of intrathecal drug delivery for patients with difficult-to-control cancer pain shows a sustained reduction in pain severity scores over a 6-month period. Palliat Med. 2015;29(6):554-563.
[Crossref] [Google Scholar] [PubMed]
- Kim EJ, Moon JY, Kim YC, Park KS, Yoo YJ. Intrathecal morphine infusion therapy in management of chronic pain: Present and future implementation in Korea. Yonsei Med J. 2016;57(2):475-481.
[Crossref] [Google Scholar] [PubMed]
- Mitchell A, Somerville L, Williams N, McGhie J, McConnachie A, McGinn G, et al. More time in a community setting: A service evaluation of the impact of intrathecal drug delivery systems on place of care of patients with cancer pain. Palliat Med. 2023;37(9):1461-1466.
[Crossref] [Google Scholar] [PubMed]
- Brogan SE, Sindt JE, Odell DW, Gulati A, Dupoiron D. Controversies in intrathecal drug delivery for cancer pain. Reg Anesth Pain Med. 2023;48(6):319-325.
[Crossref] [Google Scholar] [PubMed]
- Brogan SE. Intrathecal therapy for the management of cancer pain. Curr Pain Headache Rep. 2006;10:254-259.
[Crossref] [Google Scholar] [PubMed]
- Bruel BM, Burton AW. Intrathecal therapy for cancer-related pain. Pain Med. 2016;17(12):2404-2421.
[Crossref] [Google Scholar] [PubMed]
- Nau R, Blei C, Eiffert H. Intrathecal antibacterial and antifungal therapies. Clin Microbiol Rev. 2020;33(3):10-128.
[Crossref] [Google Scholar] [PubMed]
- Luciano P, Vicente V, Marcos AS, Gustavo FC. Role of catheter’s position for final results in intrathecal drug delivery. Analysis based on CSF dynamics and specific drugs profiles. Korean J Pain. 2013;26(4):336-346.
[Crossref] [Google Scholar] [PubMed]
- E Pope J, R Deer T, Amirdelfan K, P McRoberts W, Azeem N. The pharmacology of spinal opioids and ziconotide for the treatment of non-cancer pain. Curr Neuropharmacol. 2017;15(2):206-116.
[Crossref] [Google Scholar] [PubMed]
- Ledeboer A, Jekich BM, Sloane EM, Mahoney JH, Langer SJ, Milligan ED, et al. Intrathecal interleukin-10 gene therapy attenuates paclitaxel-induced mechanical allodynia and pro-inflammatory cytokine expression in dorsal root ganglia in rats. Brain Behav Immun. 2007;21(5):686-698.
[Crossref] [Google Scholar] [PubMed]
- Bogra J, Arora N, Srivastava P. Synergistic effect of intrathecal fentanyl and bupivacaine in spinal anesthesia for cesarean section. BMC anesthesiology. 2005;5(1):1-6.
[Crossref] [Google Scholar] [PubMed]
- Shah MS, Masoodi T, Hussain SY, Jain D. Nalbuphine as an Intrathecal Adjuvant to 0.5% Hyperbaric Bupivacaine in two different doses for post-operative analgesia after abdominal hysterectomy: A prospective, randomized, double-blind control study. Cureus. 2022;14(5):e25044.
[Crossref] [Google Scholar] [PubMed]
- Rastogi K, Bharti AK, Singh Y, Ranjan P. Comparison of dexmedetomidine and fentanyl as adjuvants to intrathecal levobupivacaine in lower segment cesarean section: A prospective, randomized double blind study. Anaesthesia, Pain & Intensive Care. 2020;24(4):383-388.
- Xiao F, Xu W, Feng Y, Fu F, Zhang X, Zhang Y, et al. Intrathecal magnesium sulfate does not reduce the ED 50 of intrathecal hyperbaric bupivacaine for cesarean delivery in healthy parturients: A prospective, double blinded, randomized dose-response trial using the sequential allocation method. BMC Anesthesiol. 2017;17(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- Winkelmuller M, Winkelmüller W. Long-term effects of continuous intrathecal opioid treatment in chronic pain of nonmalignant etiology. J Neurosurg. 1996;85(3):458-467.
[Crossref] [Google Scholar] [PubMed]
- Lin R, Zhu J, Luo Y, Lv X, Lu M, Chen H, et al. Intravenous patient-controlled analgesia versus oral opioid to maintain analgesia for severe cancer pain: A randomized phase II trial. J Natl Compr Canc Netw. 2022;20(9):1013-1021.
[Crossref] [Google Scholar] [PubMed]
- Deer T, Chapple I, Classen A, Javery K, Stoker V, Tonder L, et al. Intrathecal drug delivery for treatment of chronic low back pain: Report from the national outcomes registry for low back pain. Pain Med. 2004;5(1):6-13.
[Crossref] [Google Scholar] [PubMed]
- Atiyeh BS, Hayek SN, Skaf GS, Araj AA, Chamoun RB. Baclofen pump pocket infection: A case report of successful salvage with muscle flap. Int Wound J. 2006;3(1):23-28.
[Crossref] [Google Scholar] [PubMed]
- Gilmartin R, Bruce D, Storrs BB, Abbott R, Krach L, Ward J, et al. Intrathecal baclofen for management of spastic cerebral palsy: Multicenter trial. J Child Neurol. 2000;15(2):71-77.
[Crossref] [Google Scholar] [PubMed]
- Deer TR, Prager J, Levy R, Rathmell J, Buchser E, Burton A, et al. Polyanalgesic consensus conference 2012: Recommendations for the management of pain by intrathecal (intraspinal) drug delivery: Report of an interdisciplinary expert panel. Neuromodulation: Technology at the Neural Interface. 2012;15(5):436-466.
[Crossref] [Google Scholar] [PubMed]
- Hamza M, Doleys DM, Saleh IA, Medvedovsky A, Verdolin MH, Hamza M. A prospective, randomized, single-blinded, head-to-head long-term outcome study, comparing Intrathecal (IT) boluses with continuous infusion trialing techniques prior to implantation of Drug Delivery Systems (DDS) for the treatment of severe intractable chronic nonmalignant pain. Neuromodulation: Technology at the Neural Interface. 2015;18(7):636-649.
[Crossref] [Google Scholar] [PubMed]
- Deer TR, Pope JE, Hayek SM, Lamer TJ, Veizi IE, Erdek M, et al. The Polyanalgesic Consensus Conference (PACC): Recommendations for intrathecal drug delivery: guidance for improving safety and mitigating risks. Neuromodulation: Technology at the Neural Interface. 2017;20(2):155-176.
[Crossref] [Google Scholar] [PubMed]
- Maino P, Koetsier E. Reply to letter to the editor regarding sonographic assistance for intrathecal drugs delivery system refill. Pain Practice. 2019;19(6):677.
[Crossref] [Google Scholar] [PubMed]
- Perruchoud C, Dupoiron D, Papi B, Calabrese A, Brogan SE. Management of cancer-related pain with intrathecal drug delivery: A systematic review and meta-analysis of clinical studies. Neuromodulation: Technology at the Neural Interface. 2023;26(6):1142-1152.
[Crossref] [Google Scholar] [PubMed]
- Duarte R, Copley S, Nevitt S, Maden M, Al-Ali AM, Dupoiron D, et al. Effectiveness and safety of intrathecal drug delivery systems for the management of cancer pain: A systematic review and meta-analysis. Neuromodulation: Technology at the Neural Interface. 2023;26(6):1126-1141.
[Crossref] [Google Scholar] [PubMed]
- Mercadante S. Refractory cancer pain and intrathecal therapy: Critical review of a systematic review. Pain Ther. 2023;12(3):645-654.
[Crossref] [Google Scholar] [PubMed]
- Tashiro S, Godai K, Daitoku Y, Sato T, Enohata K, Kiyonaga N, et al. Successful intrathecal neurolytic block for the management of cancer pain in a 10-year-old child: A case report. JA Clin Rep. 2021;7:33.
[Crossref] [Google Scholar] [PubMed]
- Giglio M, Preziosa A, Mele R, Brienza N, Grasso S, Puntillo F. Effects of an intrathecal drug delivery system connected to a subcutaneous port on pain, mood and quality of life in end stage cancer patients: An observational study. Cancer Control. 2022;29:10732748221133752.
[Crossref] [Google Scholar] [PubMed]
- Janiak M, Kowalczyk R, Gorniewski G, Olczyk-Miiller K, Kowalski M, Nowakowski P, et al. Efficacy and side effect profile of intrathecal morphine versus distal femoral triangle nerve block for analgesia following total knee arthroplasty: A randomized trial. J Clin Med. 2022;11(23):6945.
[Crossref] [Google Scholar] [PubMed]
- Upadhyay SP, Mallick PN. Intrathecal Drug Delivery System (IDDS) for cancer pain management: A review and updates. Am J Hosp Palliat Care. 2012;29(5):388-398.
[Crossref] [Google Scholar] [PubMed]
- Aprili D, Bandschapp O, Rochlitz C, Urwyler A, Ruppen W. Serious complications associated with external intrathecal catheters used in cancer pain patients: A systematic review and meta-analysis. Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. 2009.
[Crossref] [Google Scholar] [PubMed]
- Engle MP, Vinh BP, Harun N, Koyyalagunta D. Infectious complications related to intrathecal drug delivery system and spinal cord stimulator system implantations at a comprehensive cancer pain center. Pain Physician. 2013;16(3):251-257.
[Crossref] [Google Scholar] [PubMed]
- Abd-Sayed A, Fiala K, Weisbein J, Chopra P, Lam C, Kalia H, et al. Intrathecal drug delivery systems survey: Trends in utilization in pain practice. J Pain Res. 2022:1305-1314.
[Crossref] [Google Scholar] [PubMed]
- Chung HT, Park SC, Kim BG, Kim NE. Epidural granuloma after intrathecal pump implantation in the spinal cord: A case report. Soonchunhyang Med Sci. 2022;28(2):145-149.
- Gehling M, Tryba M. Risks and side-effects of intrathecal morphine combined with spinal anaesthesia: A metaâ?analysis. Anaesthesia. 2009;64(6):643-651.
[Crossref] [Google Scholar] [PubMed]
- Ruan X. Drug-related side effects of long-term intrathecal morphine therapy. Pain Physician. 2007;10(2):357-366.
[Crossref] [Google Scholar] [PubMed]
- Reining M, Kretzschmar M. Loss of effectiveness with an implanted drug delivery system for intrathecal pain therapy due to corrosion. Pain Pract. 2023;23(4):459-462.
[Crossref] [Google Scholar] [PubMed]
- Staats PS. Complications of intrathecal therapy. Pain Med. 2008;9(suppl_1):S102-S107.
- Chauhan G, Khaja D, Salama-Hanna JM, Upadhyay A. Inadvertent spinal shock during an intrathecal drug delivery system refill-A case report and troubleshooting algorithm. Pain Management Case Reports. 2018;2(6):227-234.
- Narouze SN, Casanova J, Souzdalnitski D. Patients with a history of spine surgery or spinal injury may have a higher chance of intrathecal catheter granuloma formation. Pain Pract. 2014;14(1):57-63.
[Crossref] [Google Scholar] [PubMed]
- Deer TR, Prager J, Levy R, Rathmell J, Buchser E, Burton A, et al. Polyanalgesic Consensus Conference-2012: Consensus on diagnosis, detection and treatment of catheter-tip granulomas (inflammatory masses). Neuromodulation: Technology at the Neural Interface. 2012;15(5):483-496.
[Crossref] [Google Scholar] [PubMed]
- McCormick ZL, Chu SK, Binler D, Neudorf D, Mathur SN, Lee J, et al. Intrathecal versus oral baclofen: A matched cohort study of spasticity, pain, sleep, fatigue and quality of life. PM&R. 2016;8(6):553-562.
[Crossref] [Google Scholar] [PubMed]
- van Tilburg CW. Intrathecal analgesic drug delivery is effective for analgesia in a patient with post-poliomyelitis syndrome: A case report. Am J Case Rep. 2016;17:957-962.
[Crossref] [Google Scholar] [PubMed]
- Sobstyl MR, Zabek M, Brzuszkiewicz-Kuzmicka G, Pasterski T. Dual anchor internal pulse generator technique may lower risk of twiddler’s syndrome: A case series and literature review. Neuromodulation: Technology at the Neural Interface. 2017;20(6):606-612.
[Crossref] [Google Scholar] [PubMed]
- Massacesi C, Core A, Di Eusanio M, Di Francesco G, Di Saverio M, Marini L, et al. P190 Twiddler’s syndrome in a 96-year-old patient treated by repositioning the ventricular lead. Eur Heart J. 2023;25(Supplement_D):D113-D114.
- Gehling M, Tryba M. Risks and side-effects of intrathecal morphine combined with spinal anaesthesia: A metaâ?analysis. Anaesthesia. 2009;64(6):643-651.
[Crossref] [Google Scholar] [PubMed]
- Cosgrave D, Vencken S, Galligan M, McGuinness S, Soukhin E, McMullan V, et al. The effect of a low-dose naloxone infusion on the incidence of respiratory depression after intrathecal morphine administration for major open hepatobiliary surgery: A randomized controlled trial. Anaesthesia. 2020;75(6):747-755.
[Crossref] [Google Scholar] [PubMed]
- Zhou H, Zou D, Hong B, Hu R, Yang T, Li X, et al. Gadolinium-based MR cisternography with prepontine cisternal routine for evaluating distribution pattern of intrathecal targeted drug delivery in pain management. Drug Deliv. 2023;30(1):2189588.
[Crossref] [Google Scholar] [PubMed]
- Sun C, Wang YT, Dai YJ, Liu ZH, Yang J, Cheng ZQ, et al. Programmable pump for intrathecal morphine delivery to cisterna magna: clinical implications in novel management of refractory pain above middle thoracic vertebrae level utilizing a prospective trial protocol and review. Anesth Pain Med. 2021;11(3):e115873.
[Crossref] [Google Scholar] [PubMed]
- Sadekar SS, Bowen M, Cai H, Jamalian S, Rafidi H, Shatzâ?Binder W, et al. Translational approaches for brain delivery of biologics via cerebrospinal fluid. Clin Pharmacol Ther. 2022;111(4):826-834.
[Crossref] [Google Scholar] [PubMed]
Citation: Mohabbati V, Mohabbati P, Papan M (2025). Evaluating Intrathecal Therapy in Cancer Pain: A Review with Case Study Perspectives. J Pain Manage Med. 11:306.
Copyright: © 2025 Mohabbati V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.