Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
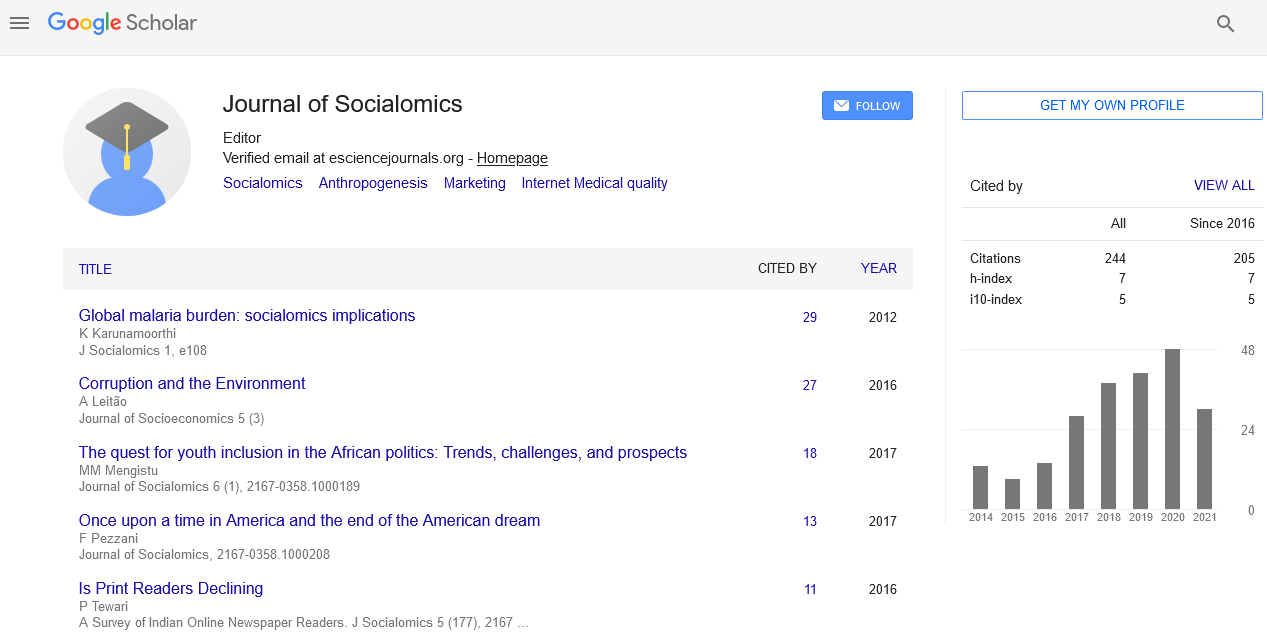
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2023) Volume 12, Issue 3
Exploring Alternatives to the Medical Quality Adjusted Price Index
Keyserlingk Ritter*Received: 02-May-2023, Manuscript No. JSC-23-21774; Editor assigned: 05-May-2023, Pre QC No. JSC-23-21774 (PQ); Reviewed: 19-May-2023, QC No. JSC-23-21774; Revised: 26-May-2023, Manuscript No. JSC-23-21774 (R); Published: 02-Jun-2023, DOI: 10.35248/2167-0358.23.12.189
Description
The Quality Adjusted Price Index (QAPI) has become an increasingly popular tool for measuring the cost of medical care. By taking into account the quality of care provided, QAPI can provide a more accurate picture of the costs associated with medical services. It is a method of evaluating health care by incorporating quality measures into price index calculations. QAPI was developed to help hospitals and other healthcare organizations better assess the value of their services. It is based on data from multiple sources such as patient surveys, claims data, and cost reports. By taking into account patient satisfaction and outcomes, QAPI helps organizations determine how much they should charge for their services without sacrificing quality. QAPI has become an important tool for evaluating the cost effectiveness of medical treatments and procedures. It allows providers to compare prices between different providers while still considering quality measures such as patient satisfaction or outcomes. This makes it easier to make decisions about which treatment options are most cost effective without sacrificing quality. QAPI is also used by insurers to determine what level of coverage they should offer for specific treatments or medications. By incorporating quality measures into their pricing models, insurers can ensure that they are providing coverage that meets their customers’ needs while keeping costs reasonable.
As medical costs continue to rise study are looking for costeffective alternatives to the traditional Quality-Adjusted Price Index (QAPI) when measuring medical care prices. QAPI is a measure of the prices of health services that takes into account the quality of those services. While it is effective in providing an accurate picture of health care prices, it can be expensive and time-consuming to use. Fortunately, there are several costeffective alternatives to QAPI that study can use in order to measure medical care prices. These include price indices based on relative value units (RVUs), surveys of providers, and data from administrative claims databases. Each of these methods has its own advantages and disadvantages, so it’s important for study to understand them in order to choose the best approach for their needs. Relative Value Units (RVUs) are a way of assigning values to different types of medical services based on their complexity and cost.
This allows study to compare the prices of different types of services more accurately than with QAPI. RVU-based price indices also provide more granular pricing information than QAPI, which can be useful when study specific treatments or procedures. However, RVUs do not take into account quality differences between providers, so they may not be as accurate as QAPI in certain cases. Surveys are another way study can measure medical care prices without using QAPI. Surveys allow study to collect pricing information directly from providers, which can provide a more accurate picture than using an index like RVU or QAPI. As the cost of medical care continues to rise, it has become increasingly important for healthcare providers and administrators to explore cost-effective alternatives to the traditional Quality-Adjusted Price Index (QAPI). QAPI is a measure of the overall cost of medical services including both quality and quantity factors. While this index can provide an accurate representation of overall costs, there are numerous benefits associated with using cost-effective alternatives. One benefit of using cost-effective alternatives is that they can help healthcare providers save money by reducing their costs. Alternatives such as the Resource-Based Relative Value Scale (RBRVS) or Activity Based Costing (ABC) can be used to identify areas where costs can be reduced without compromising quality. This is especially beneficial for organizations that are dealing with limited budgets and need to make cuts in order to remain financially viable. Another advantage of using costeffective alternatives is that they can help healthcare providers improve the quality of care they provide. By focusing on areas where costs can be reduced, healthcare administrators are able to ensure that resources are allocated in a more effective manner.
Citation: Ritter K (2023) Exploring Alternatives to the Medical Quality Adjusted Price Index. J Socialomics.12:189.
Copyright: © 2023 Ritter K. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.