Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 11, Issue 5
Evaluating the Spatial Mismatch Hypothesis: A Comprehensive Analysis of Access to Primary Care Physicians and Healthcare Disparities in Eastern Quebec
Christian Simoneau*Received: 18-Sep-2023, Manuscript No. HCCR-23-23078; Editor assigned: 21-Sep-2023, Pre QC No. HCCR-23-23078 (PQ); Reviewed: 04-Oct-2023, QC No. HCCR-23-23078; Revised: 11-Oct-2023, Manuscript No. HCCR-23-23078 (R); Published: 18-Oct-2023, DOI: 10.35248/2375-4273.23.11.371
Abstract
Objective: The primary objective of this study is to conduct a rigorous and comprehensive assessment of the relationship between the deficiency of medical care accessibility in rural areas, with a particular focus on the most susceptible and vulnerable segments of the population. In order to achieve this objective, the study employs the utilization of the Enhanced Two-Step Floating Catchment Area (E2SFCA) methodology, and examines its implications for the Spatial Mismatch Theory in line with the Central Place Theory. Through the application of this theoretical framework, this paper endeavors to elucidate and focus on the aforementioned deficiency, by explicating the observed incongruity between the requirements and needs of specific population segments, and the scarcity of available primary care services. By providing a detailed and nuanced analysis of these issues, this study aims to contribute to our understanding of the challenges facing rural populations in accessing essential medical care.
Method: In order to rigorously assess the validity and applicability of the Spatial Mismatch Hypothesis within the context of this investigation, a comprehensive and systematic approach was employed. This entailed the incorporation and analysis of a diverse range of data, including information pertaining to employment rates, educational attainment levels, and average commute durations, all of which were sourced from the 2016 Canadian Census. Furthermore, in order to ensure the highest degree of accuracy and reliability in our findings, an advanced two-step floating catchment area methodology was utilized as part of our analytical framework.
Results: The systematic investigation and scrutiny of the data concerning employment rates, levels of educational attainment, and average commute durations do not furnish conclusive evidence to substantiate the presence of a significant accessibility deficit among the population. Moreover, these observations serve to refute the validity of the Mismatch Spatial Hypothesis, specifically. In contrast, the Central Place Theory appears more suitable for elucidating access levels for the working population possessing a high school diploma or higher. It is apparent that the provision and accessibility of primary care services remain inextricably intertwined with, and dependent upon, the existence of sufficient road infrastructure. As a result, individuals residing at substantial distances from the primary road network may experience severely compromised access to such services.
Conclusions: This study has conducted a rigorous and comprehensive assessment of the relationship between the deficiency of medical care accessibility in rural areas, with a particular focus on the most susceptible and vulnerable segments of the population. Through the utilization of the Enhanced Two-Step Floating Catchment Area (E2SFCA) methodology, and the examination of its implications for the Spatial Mismatch Theory in line with the Central Place Theory, this paper has elucidated and shed light on the aforementioned deficiency. The findings of this study indicate that the Central Place Theory appears more suitable for elucidating access levels and that the provision and accessibility of primary care services remain inextricably intertwined with, and dependent upon, the existence of sufficient road infrastructure. As such, it is evident that individuals residing at substantial distances from the primary road network may experience severely compromised access to such services. This study has contributed to our understanding of the challenges facing rural populations in accessing essential medical care, and highlights the need for further research and policy interventions to address these issues.
Keywords
Spatial Mismatch Hypothesis (SMH), Central Place Theory (CPT), Enhanced Two-Step Floating Catchment Area (E2SFCA), Primary care physicians
Introduction
The discrepancy in the accessibility of healthcare between urban and rural populations has been thoroughly investigated in developed countries. Numerous studies have explored the availability of healthcare services in urban areas, including research conducted by Apparicio, et al., Fone, et al., Grumbach, et al., Luo and Qi and Shah, et al., [1-5]. Conversely, other studies have specifically examined the availability of healthcare services in rural areas, such as research by Arcury, et al., Laditka, et al. and McGrail, et al. [6-9]. Despite the existence of these studies, few have addressed the variations in the availability of healthcare services between urban and rural contexts.
The impact of geographical remoteness on healthcare access has received limited attention. For example, Hausdorf et al. observed that inhabitants of remote regions reported lower satisfaction with healthcare access [10]. Laditka et al. found that hospitalization rates increased with greater rurality [7]. Despite the generalized perspective that the health status of rural populations is inferior to that of their urban counterparts, urban researchers seldom regard these populations as vulnerable. In fact, Champagne, et al. discussed access issues for young and elderly patients or those with developmental mental health concerns in a study measuring access to primary medical services but did not consider challenges associated with distance within rural regions [11].
One study that does address this issue is that of Salze, et al. which were conducted in France [12]. This study highlights the importance of rurality as a factor that reduces access to healthcare services. Additionally, numerous other studies have confirmed the association between rural residence and decreased access to and utilization of healthcare services. These include research by Farrington, et al., Hausdorf, et al. and Al-Taiar, et al. [10,13,14]. These studies suggest that there are significant differences in access to healthcare services between urban and rural areas, and that more research is needed to understand these differences and develop effective policy solutions.
Sibley and Weiner conducted a comparative analysis of the likelihood of obtaining vaccinations, having a regular physician, and consulting a specialist between urban and rural regions [15]. Populations residing in these areas were found to encounter greater obstacles in accessing primary care and emergency departments [11]. The level of mobility affects proximity. If an area has a high mobility disadvantage, the population’s ability to transcend the distance between themselves and available services decreases. The reduced availability of healthcare services was primarily attributed to a shortage of clinicians, resulting in extended travel times. Other factors, such as transportation availability, can influence perceptions of access and consequently the utilization of health services [6,16]. Several studies have also established a correlation between rural residency and decreased access to or utilization of health services [10,13,14].
Literature Review
In recent years, concern over disparities in healthcare outcomes and access between urban and rural areas has intensified. Hospitals in urban centers are staffed by qualified practitioners and well-stocked with medications, enabling them to provide optimal care. When problems arise, they are efficiently addressed due to the availability of resources for resolving various challenges. In contrast, rural areas often struggle to effectively address issues such as poor road networks. This can result in inadequate healthcare provision and prompt patients to travel to urban centers in search of quality care [17]. Poor road networks and a shortage of skilled practitioners are persistent problems in rural areas that can persist for generations.
The development of healthcare services appears to occur in clusters, with patients gravitating towards specific poles to access required resources. In the context of healthcare, urban residents generally have access to higher quality care than their rural counterparts. Quality care is primarily concentrated in urban centers, necessitating that rural residents travel to these locations to receive optimal services. The provision of quality healthcare in rural areas is often centralized near hospitals, which is suboptimal given that many individuals are unable to access the services they require if they are located at a distance from such facilities. In contrast, urban residents are well-positioned to access the healthcare services they need due to the high quality of care and the abundance of healthcare units in these areas.
Rural residents often encounter obstacles such as extended travel distances and times, limited healthcare facilities and services, and a shortage of medical professionals when seeking healthcare services. These challenges have been associated with adverse health outcomes, including higher rates of chronic diseases, increased mortality rates, and diminished quality of life [18]. According to the SMH framework, inequities in healthcare service access arise from a mismatch between the spatial distribution of healthcare resources and the population. This mismatch is exacerbated in rural regions by the lack of primary care clinics, hospitals, and medical personnel, as well as the distance to healthcare facilities.
Adequate access to quality healthcare services is a crucial determinant of population health, particularly in rural regions where the availability and accessibility of such services are frequently constrained. The Spatial Mismatch Hypothesis (SMH) is a framework that could be employed to examine the relationships between geographical access to primary care services and general population health outcomes. Kain first introduced the theory in 1968 to elucidate the mismatch between employment opportunities’ location and individuals seeking employment opportunities, resulting in increased unemployment rates and social isolation [19].
An examination of the centrality concept outlined in the central place theory could also provide insight into the relationship between the provision of healthcare services in urban and rural areas. The quality of services available can help to explain the lack of optimal care in regions distant from urban centers. The level of medical care that patients receive, or the importance of a city in terms of healthcare provision, is determined by the availability of specialized services. For example, urban centers may offer psychiatry and cardiology services that are not commonly found in rural areas. In such cases, the urban region can be considered a hub for the distribution of these services, highlighting the challenges faced by rural patients who are unable to access such care locally and must travel to urban clusters to receive these services.
Given the pivotal role of primary care services in promoting health and preventing disease, it is essential to comprehend the impact of the Spatial Mismatch Hypothesis (SMH) on rural medical access to primary care, as well as the significance of central place theory and growth pole theory. The objective of this study is to contribute to the ongoing discourse on enhancing healthcare access and outcomes in rural areas by identifying the challenges faced by rural residents and proposing solutions to these issues.
Spatial mismatch hypothesis
The SMH has garnered considerable attention in the context of employment and labor markets. Recently, researchers have begun to apply this approach to healthcare access, particularly in rural regions. Previous research has demonstrated that spatial mismatch, defined as the discrepancy between health services’ location and those requiring such services, poses a significant barrier to rural healthcare access [20]. Coughlin, et al. investigated the spatial mismatch between the geographic distribution of primary care physicians and healthcare in the United States of America [21]. The study revealed that primary care physicians were less prevalent in rural areas compared to metropolitan regions, where there was a greater spatial mismatch. This study determined that rural counties in the United States of America have higher poverty rates, transportation challenges, lower educational attainment, a disproportionately larger elderly population, and accessibility issues for healthcare services. Due to these factors, many rural counties in the United States of America experience elevated mortality and morbidity rates. Rural patients have exhibited a higher prevalence of chronic diseases and difficulty receiving care for various mental health conditions. The authors concluded that this spatial mismatch contributed to reduced healthcare access and inferior health outcomes among rural populations.
Jensen, et al. observe that rural regions of the United States of America persist in reporting elevated rates of population aging and have documented disproportionate proportions of individuals in poor health compared to urban areas [22]. According to the authors, rural counties in the United States of America exhibit significant rural-urban disparities in mortality and health. These regions are also characterized by reduced life expectancy, which can be attributed to inadequate access to healthcare, resulting in adverse health outcomes. Additionally Jensen, et al. report that multidimensional and multilevel factors influence diverse population health trends, including population composition and local service, economic, natural, policy, and social environment [22]. The authors identified a spatial mismatch in access to medical services in rural areas based on these factors. In another study examining the relationship between access to primary healthcare and ethnic/racial residential segregation in rural regions, Caldwell, et al. determined that segregation significantly contributed to inadequate access to healthcare [23]. When the study expanded its unique segregation scale beyond urban regions, it revealed a complex interplay between spatial and social factors in rural areas.
Neely and Ponshunmugam employed a combination of household surveys, documentary analysis, and in-depth interviews to investigate instances when individuals accessed healthcare outside the standard government protocol [24]. Conducted in South Africa, the study revealed that transportation, resource scarcity, and kinship networks, rooted in the country’s economy and a history of segregation along racial lines, exerted the most significant impact on healthcare access, particularly in rural areas. In another study conducted by Shah, et al. in Ontario, Canada, the findings indicated that the Southwestern region exhibited superior geographic accessibility to healthcare providers compared to other regions experiencing provider shortages [5]. Additionally, the study demonstrated that the distribution of care providers was unequal across the region’s urban-rural continuum, with rural areas exhibiting the lowest accessibility. The study concluded that a mismatch exists between the region’s distribution of healthcare providers and high percentages of seniors, compelling many elderly individuals to travel extended distances to access primary healthcare.
The Spatial Mismatch Hypothesis (SMH) appears to be a suitable theoretical framework for elucidating the disparities in healthcare access observed in rural areas. Additionally, the application of central place theory and growth pole concepts, which are frequently employed in regional development, may provide further insight into this phenomenon.
Central place theory
The central place theory is a concept used to describe the distribution, size, and number of market services within human settlements. According to the central place theory, settlements are expected to function as “central places,” providing goods and services to their surrounding areas. However, the provision of these commodities is contingent upon their availability, and some “central places” may lack sufficient services to meet the needs of their residents. While urban “central places” are able to provide their residents with all necessary commodities, rural inhabitants often lack access to essential resources for leading an optimal life. This is also evident in the provision of quality healthcare, with rural residents frequently experiencing inadequate care and being forced to travel to urban centers to seek quality services, despite government intervention measures. This same framework can be applied to understand the relationship between primary care services offered in urban environments and the limited availability of quality care in rural areas.
The central place theory posits that all consumers possess equal purchasing power and are likely to frequent the nearest central place that can provide them with the services they require. As Xu, et al. note, when transportation systems and markets undergo restructuring, patients are likely to travel to the nearest city to procure essential commodities [25]. Cities are well-connected due to the development of high-quality transportation networks, in contrast to rural areas, which often lack adequate or efficient transport systems.
The implementation of advanced information technology systems has facilitated the exchange of data and improved the provision of services. This is also evident in the healthcare sector, where urban residents have access to high-quality primary care. The availability of a wide range of resources, coupled with advancements in technological systems, ensures that urban residents have access to all necessary materials and services. Healthcare facilities in urban areas are well-equipped and have an adequate supply of medicines. In contrast, rural centers often struggle to provide primary care due to various challenges, such as a shortage of skilled personnel and medications [26]. As a result, rural residents must travel to urban centers to access necessary services.
By utilizing the framework provided by the central place theory, it is possible to explain the spatial distribution of healthcare facilities in rural areas. The distribution of healthcare units in urban centers follows a pattern of decreasing density from central business districts towards peripheral areas. Within each region, there is a territorial distribution of clusters that are closely connected to traffic routes. The level of hospitalization and development in urban areas exhibits a high degree of coupling.
Urban healthcare facilities are dispersed throughout densely populated areas and strive to meet the needs of their patients. A comprehensive central system is created by hospitals located in close proximity to one another, which are connected to all surrounding areas, making them accessible to a large number of individuals. Several factors influence the spatial distribution of urban hospitals, including cost and cultural considerations. Studies of the spatial distribution of urban hospitals have examined their levels and scales, as they are designed to serve a large volume of patients and ensure that their needs are met [27]. The operational strategies of these facilities can be understood through the lens of the central place theory, given the high degree of similarity between the two systems.
The central place theory defines the threshold of a given process as the minimum number of individuals required to purchase a good or service in order for a supplier to remain in business. In such a scenario, all expenses are recouped, but the business may not generate a profit. Hospitals in urban centers have a greater likelihood of meeting their financial obligations and remaining operational due to their large customer base. This helps to reduce operational costs, increase revenue, and support institutional growth. The centralization of services in large cities enables companies to benefit from economies of scale, allowing them to expand their operations and improve efficiency.
The concept of range, as applied by the Central Place Theory, can aid in elucidating the disparities in access to medical care between rural and urban areas. The paucity of healthcare facilities and services in rural regions is a cause for concern; rural inhabitants are unable to evaluate the quality of services they receive in comparison to the functional systems in urban centers. According to the theory, range pertains to the determination of the distance a consumer is willing to travel to obtain a service. Urban centers boast an abundance of healthcare facilities and optimal healthcare services. In contrast, rural patients must traverse considerable distances to obtain quality care. The Central Place Theory posits that beyond a certain threshold, a service may become prohibitively expensive, with the costs of travel and time outweighing the benefits of the service. Rural residents must bear these costs to access the quality care they require. In a given region, a single city may be surrounded by smaller towns and hamlets; this same principle applies to healthcare units established within a locality [28]. There exists a positive correlation between a city’s growth and the availability of healthcare facilities. This implies that major hospitals will be encircled by numerous smaller clinics that rely primarily on the main hospital for specialized care. Just as residents migrate to cities in search of advanced services, rural hospitals refer patients to major healthcare units in urban centers. Patients must travel considerable distances to receive treatment services. Thus, it is evident that the central city plays a crucial role in fulfilling the healthcare needs of individuals residing in rural areas or “hinterlands.”
In rural areas, the population is spatially dispersed and may lack the financial resources to sustain a healthcare facility at optimal levels of operation. According to the central place theory, urban centers dominate rural areas, and the threshold concept may not be applicable in these regions. Some healthcare facilities may struggle to provide optimal services and may operate at a loss or even close due to their inability to reach the necessary threshold levels. A high- threshold function requires a substantial customer base to remain profitable. Urban centers, as conceptualized by the central place theory, require a large population to support their operations. This is also true for healthcare facilities located in urban areas, which rely on a large patient base to sustain their functionality. According to the central place theory, a high-range function attracts individuals from distant locations to access its services, explaining why urban healthcare systems often outperform their rural counterparts.
This finding is consistent with the tenets of growth pole theory, which posits that economic development is not uniformly distributed within a given region. Instead, it transpires around specific poles or clusters where industries are concentrated. Urban centers experience elevated levels of growth and development, primarily due to the advancement of core industries. The growth pole serves as a catalyst for economic growth within a region. The progression of working processes in and around large cities contributes to the development of surrounding regions. In contrast, rural areas exhibit lower levels of economic development due to limited exchange of goods and services [29]. As cities develop, all other working systems are expected to follow suit; this explains why healthcare units in urban centers are more advanced than those in rural areas. The frequency of commodity exchange between urban hospitals is heightened; they are interconnected, facilitating the sharing of information and skills, thereby placing them far ahead of rural units. Consequently, rural patients must travel to urban centers to obtain quality services.
Urban centers are fields of force, constituting homogeneous spaces in which all economic activities, including hospitals, enjoy similar environmental benefits. This enables healthcare units to achieve advanced growth and surpass their rural counterparts. Urban areas benefit from superior growth policies, effective economic planning, a skilled workforce, and advanced technological systems. Consequently, activities within urban centers are optimized, allowing healthcare units to operate at peak efficiency and attain their developmental objectives.
Perroux’s Growth Pole Theory is predicated on Schumpeter’s theory, which examines the role of innovation. Schumpeter’s theory posits that innovations are instrumental in driving economic growth within a region and that advancements in technological systems occur primarily within large firms. These dynamic, propulsive firms exert dominance over other entities, ensuring that they alone are best equipped to provide quality services. Healthcare units situated in these regions dominate their rural counterparts, thereby limiting their capacity for innovation and growth. In contrast, hospitals located in rural areas suffer from inadequate planning among stakeholders [30]. These factors contribute to the significant disparities between hospitals situated in rural and urban settings.
Hospitals located in urban settings stand to benefit more from technological advancements than their rural counterparts. According to the Growth Pole Theory, individuals residing in areas surrounding a major town tend to migrate to urban centers to conduct their various affairs, a phenomenon that further enhances these settings. Working systems, such as hospitals, receive substantial financial support; rural inhabitants play a role in developing urban hospitals rather than focusing on improving units closer to their homes.
Agglomerations and cumulative causation ensure that urban centers accumulate a large number of firms. This results in increased population levels, which in turn drives a high influx of patients to urban hospitals that enable these hospitals to sustain their operations and enhance the quality of their working processes. Consequently, primary care services are provided optimally, and patients can be assured of accessing the desired working processes. In rural areas, investment is often minimal. This leads to a deficit in medical access; hospitals established in such regions lack adequate medicine and physicians [31]. The absence of backward and forward linkages contributes to the lagging of rural areas. Working systems such as healthcare units lack the necessary resources to operate effectively, compelling rural residents to seek quality care in urban healthcare facilities. In urban centers, backward linkages ensure that inhabitants and hospitals receive a steady supply of primary goods and raw materials. This cycle of businesses ensures that economic activities within urban areas continue to flow and achieve desired working levels.
Methodology
McGrail and Humphreys found that the E2SFCA method is the best way to measure how easy it is for people in rural areas to get to primary care [8]. In order to accurately assess access to primary care, it is essential to consider the location and proximity of both providers and populations. In this study, population data was obtained from the 2016 Canadian national census using Dissemination Areas (DAs), which represent the smallest standard geographic areas containing all census data. On average, DAs in this study had a population of 496 and an area of 342 km2.
This study focuses on the four easternmost regions of Quebec province, which are primarily rural in nature with the exception of several small urban centers. While two small universities within these regions offer training for certain health professions, individuals seeking to become general practitioners must complete their formal medical education in Quebec City or beyond. Nursing education is more widely available throughout Eastern Quebec.
The Cote-Nord region has a vast land area of 240-7655 km2 and a population of 92518. The region is served by 77 dedicated full- time general practitioners, resulting in a ratio of 0.8-3 GP per one thousand inhabitants. The regional economy is primarily driven by mining, lumbering, aluminum production, and tourism. The Gaspésie-Iles-de-la-Madeleine region has a land area of 20,272 km2 and a population of 92,403. It is served by 131 general practitioners with a ratio of 1.45 GP per 1000 inhabitants. The economy has been centered on fishing, agriculture, and forestry. The Bas-Saint- Laurent region is demarcated by the Saint Lawrence River and has a population of 1,97,385. Within this region, 227 general practitioners were enumerated, yielding a ratio of 1.15 GP per 1000 inhabitants. Saguenay–Lac-Saint-Jean is known for the Saguenay Fjord and has a population of 2,75,552. The region has 288 general practitioners with a ratio of 1.04 GP per 1000 inhabitants. The manufacturing, education, health and social assistance, and trade sectors account for nearly half of the region’s GDP.
We will measure access to healthcare in those regions using a method called the Floating Catchment Area (FCA). This method calculates the number of doctors available for each person in an area by looking at how many medical facilities are within a reasonable distance. As the distance between doctors and patients increases, the number of times they interact decreases [4]. This is shown in this model:
Where, A represents the sum of the spatial accessibility from population i, Sj is the number of general practitioners at location j, dij constitutes the travel time between i and j and V is the population demand defined as following:
Where, Pk is population demand at location k, dkj is travel time between k and j while β is the distance decay (travel impedance) coefficient. This method uses a buffer radius to show how far people are willing to travel to get healthcare services. It assumes that people want to minimize their costs when choosing where to go for healthcare.
In order to understand the accessibility of medical clinics for rural populations, we utilized a combination of geographic information systems and network analysis. Using the “closest facility” tool of QGIS’s Network Analysis module and the TravelTime (TM) API, we calculated the proximity between geocoded medical clinics and population centroids within a maximum catchment size of 100 minutes. This catchment size is based on previous research that suggests a distance of 60 minutes to 120 minutes is generally considered appropriate in rural contexts. We obtained road network data from Open Streets and used travel time instead of distance by combining road length with average speed. This allowed us to apply the E2SFCA method to the exported data using a spreadsheet. Our beta coefficient was linear, corresponding to a 1% decrease in access per driven minute. Linear coefficients are commonly used in rural contexts and are easier to calculate while maintaining the internal rationale of the beta coefficient in the E2SFCA method [32].
The E2SFCA method is a powerful tool for understanding healthcare accessibility by aggregating data to create an accessibility measure. In the first step, a population-to-provider ratio is calculated for each healthcare clinic by including all population locations within our defined threshold, which in this case is 100 minutes. This step does not take into account distance decay as each clinic is static. In the second step, another population-to-provider ratio is calculated for each population centroid within each dissemination area using a distance decay of β to represent distance friction. This impedance function reflects reality by translating the cost of traveling further as a barrier to access, making clinics that are farther away less accessible to the population. Without this function, access would be the same for everyone within the catchment area, which is not realistic. This approach provides a nuanced understanding of healthcare accessibility in rural areas.
The ideal ratio of general practitioners to population is a topic of much debate within the field of healthcare accessibility. While this ratio can vary depending on a variety of factors, the most commonly recommended ratios range from 22.5 to 40.5 family physicians per 100,000 inhabitants. This range is based on extensive research and analysis of healthcare systems and population health outcomes. In our analysis, we will use this range as the lower and upper limits for determining whether access to general practitioners is insufficient (below 22.5) or overprovisioned (above 40.5). This will allow us to create three categories of access that demonstrate the level of access offered to the population. By using these categories, we can gain a nuanced understanding of healthcare accessibility in different regions and identify areas where access may be lacking or where there may be an overabundance of general practitioners [33].
In our study, we will incorporate data from the Canadian Census to evaluate potential spatial mismatches across four regions in terms of population education levels, work activity, commute duration, and the Pampalon Deprivation Index (PDI). The PDI is a valuable tool for identifying regions with high levels of material and social deprivation and for measuring social inequalities over time and space. Through a rigorous analysis of the data, we aim to determine if there are any discrepancies between individuals’ residential locations and their places of employment or education. This will provide us with a deeper understanding of the challenges individuals may face in accessing education, employment opportunities, and healthcare within their communities. Our approach will offer valuable insights into the spatial dynamics of these regions and aid in identifying areas where interventions may be necessary to improve access to education, employment, and healthcare. By comprehending the complex interplay between residential location, employment, education, and healthcare access, we can develop more effective strategies for addressing spatial mismatches and enhancing the well-being of individuals in these communities [34-36].
Results
According to the results obtained through the application of the Enhanced Two-Step Floating Catchment Area (E2SFCA) method, as illustrated in Figure 1, it is evident that the southeast regions, which are more densely populated, enjoy better access to healthcare services. In contrast, the less populated and remote areas experience a significant decrease in access to these services. As such, populations residing in small towns located near main roads can benefit from improved access to general physicians, as they can easily reach nearby towns where these services are available. This is further supported by data showing that patients from these areas often seek medical attention at emergency rooms or clinics located in neighboring towns, thereby increasing their actual medical access. On the other hand, individuals living in more remote areas, further away from main roads and relying on unnumbered rural roads or dirt roads, face significant challenges in accessing healthcare services. These challenges are further exacerbated by the limited availability of healthcare providers in these regions. Overall, the results obtained through the application of the E2SFCA method highlight the disparities in healthcare access between urban and rural areas and underscore the need for targeted interventions to improve access to healthcare services for populations living in remote regions (Figure 1).
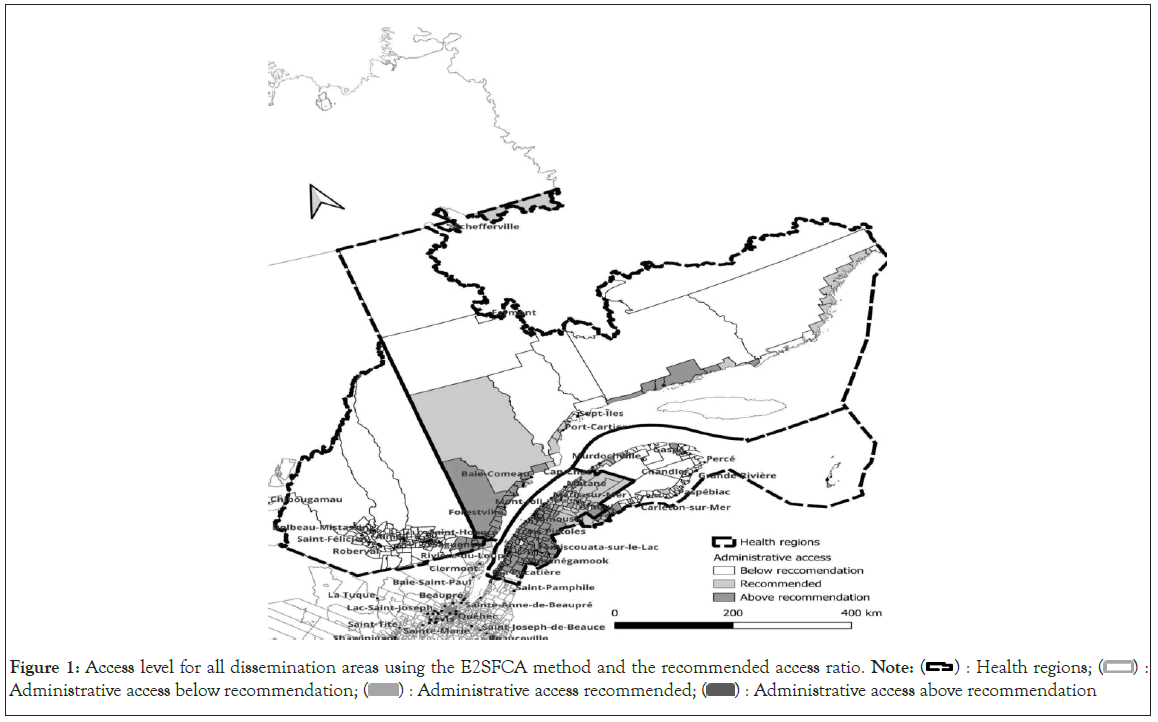
Figure 1: Access level for all dissemination areas using the E2SFCA method and the recommended access ratio. Note:  Administrative access below recommendation;
Administrative access below recommendation;  Administrative access recommended;
Administrative access recommended; Administrative access above recommendation
Administrative access above recommendation
The analysis of healthcare accessibility in relation to the distance from the provincial capital, as shown in the lower left section of the map, reveals a significant reduction in accessibility as one moves further away from the capital. This highlights the crucial role played by a well-developed road network in ensuring optimal accessibility to healthcare services. In regions with access to highways, accessibility is significantly improved, as these areas are well-connected to major urban centers where healthcare services are readily available. However, as the road network transitions from highways to regular roads, rural roads, and ultimately dirt roads, accessibility diminishes considerably. By using the access average to create a new map of healthcare accessibility, as illustrated in Figure 2, the contrast between regions with high and low accessibility becomes more apparent. This further underscores the importance of investing in the development and maintenance of a robust road network to improve access to healthcare services for populations living in remote regions (Figure 2).
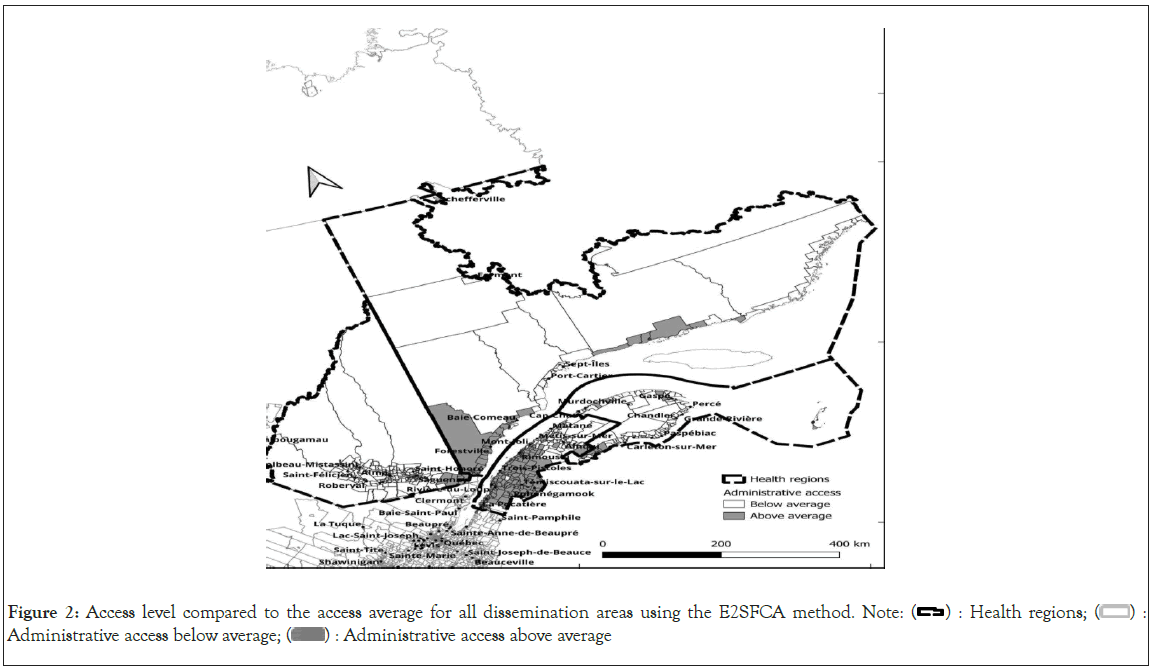
Figure 2: Access level compared to the access average for all dissemination areas using the E2SFCA method. Note: 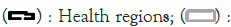 Administrative access below average;
Administrative access below average;  Administrative access above average
Administrative access above average
Using the Enhanced Two-Step Floating Catchment Area (E2SFCA) method, primary care accessibility was analyzed in four regions. In the Bas-Saint-Laurent region, accessibility was satisfactory up to the end of the Transnational Highway, but decreased further eastward and in smaller towns lacking direct highway access. 5.4% of dissemination areas had low access to primary medical care. In the Saguenay region, 94.9% of dissemination areas fell below the recommended physician-to-population ratio, with a pronounced deficiency in rural areas due to limited road network extension. In the Gaspesie region, even the easternmost Gaspé region had suboptimal accessibility, with 58.3% of dissemination areas having low access to primary care. The Cote-Nord region exhibited a similar pattern, with diminished road access correlating with reduced primary care accessibility and 28.8% of the region lacking sufficient access.
Data from Statistics Canada in 2016 showed that in 14 Dissemination Areas (DAs), over 20% of the population had a commute time exceeding one hour to reach their workplace, and in 13 DAs, no residents had a commute time of less than 15 minutes. This suggests that access to primary medical care may also take longer due to the vast distances that must be traversed. Private automobiles were the predominant mode of transportation to work, accounting for 75% of all transportation in over 90% of our DAs. In contrast, active modes of transportation, such as walking, were less commonly used, with less than 10% of the population commuting to work by walking in more than 77% of DAs, and no residents walking to their workplace in 48% of DAs.
The Deprivation Index (DPI) is a composite measure that incorporates unemployment data and education level as its core components. Given the presence of autocorrelation, it would be methodologically unsound to measure the correlation of the DPI with these data sets. However, within the confines of our study area, an analysis of the data reveals a negative correlation between social deprivation and material deprivation (-0.231). Furthermore, social deprivation is positively correlated with the mode of transportation to one’s place of employment, specifically walking (0.316), while exhibiting a negative correlation with car ownership (-0.296). It is therefore not unexpected that social deprivation is also correlated (0.253) with proximity to one’s place of employment, defined as a commute time of less than 15 minutes. An analysis of unemployment data and educational attainment levels reveals a positive correlation (0.343) between unemployment and the absence of a high school diploma.
A more detailed examination of access data reveals weak but statistically significant correlations between improved access to primary care services and the absence of a high school diploma (0.141), as well as between better access to primary care and higher unemployment rates (0.144). Dissemination Areas (DA) characterized by higher levels of educational attainment, specifically high school diplomas and post-secondary diplomas, exhibit a decrease in access to primary care services (-0.152).
The data presented can be interpreted through two distinct logical frameworks. The first framework posits that state-led redistribution efforts improve access to essential services for those most in need, thereby demonstrating the positive impact of such policies on vulnerable populations. Conversely, the second framework suggests that individuals with higher levels of educational attainment are more likely to be homeowners and may choose to reside further away from urban centers where hospitals and medical clinics are typically located, resulting in the observed negative correlation in the data. These two frameworks offer contrasting interpretations of the data and highlight the complex interplay between social and economic factors in shaping access to essential services. Further research is needed to better understand these relationships and to develop effective policy interventions to address disparities in access to primary care services.
Discussion and Conclusion
The data presented in this study suggests that the mismatch between accesses to primary medical care cannot be adequately explained by the Spatial Mismatch Hypothesis, as there is no observed correlation between poorer and less educated dissemination areas and reduced access to primary care services. As such, it is necessary to turn our attention to the Central Place Theory in order to analyze and interpret our findings. In light of this theoretical framework, the concentration of medical activity near urban centers and in proximity to major road networks appears to corroborate the premise of the Central Place Theory, which posits that more developed and advanced business centers tend to agglomerate near a central location, resulting in a snowball effect.
These findings underscore the importance of considering alternative theoretical frameworks in order to better understand the complex relationships between social, economic, and spatial factors in shaping access to essential services. Further research is needed to fully elucidate these relationships and to develop effective policy interventions to address disparities in access to primary medical care.
Healthcare services are less readily available in rural areas than in urban centers, resulting in patients residing in rural regions being more likely to travel to urban centers in search of quality care that is unavailable in nearby facilities. However, the Spatial Mismatch Hypothesis (SMH) framework does not appear to be an appropriate framework for addressing healthcare inequities in rural areas. In contrast, the Central Place Theory, which posits that urban centers exert considerable control over a large patient population, seems more suitable to do so. In rural areas, the quality of primary care is suboptimal due to limited investment; consequently, many residents migrate to urban centers in search of treatment services. This development is not uniformly distributed and tends to occur within specific poles. This principle applies to the development of healthcare; urban units are more advanced and provide optimal care to their patients. Rural units lack certain necessities, compelling patients to travel to urban centers in search of optimal services.
The findings of this paper indicate that there is a small but significant mismatch in access to healthcare services among rural residents. However, this mismatch is better explained by the Central Place Theory than by the Spatial Mismatch Theory. This mismatch is due to several factors, including longer travel distances and times required to reach healthcare facilities, a limited number of healthcare facilities and services available in rural areas, and a shortage of medical professionals willing to work in rural communities. There are several promising policy recommendations that can be implemented to improve access to primary care in rural areas. One potential solution is to increase funding for rural healthcare facilities, which could involve providing financial assistance to struggling facilities and incentivizing the development of new facilities in rural areas. Governments at the local and provincial levels can focus on programs that incentivize primary care providers to work within rural communities. Additionally, funding can be allocated towards training programs designed to equip rural residents with the knowledge and skills necessary to work in the healthcare field.
Another potential policy solution is the expansion of telemedicine services in rural areas. This innovative approach can increase access to healthcare and reduce the spatial mismatch between care providers and patients. The delivery of valuable healthcare services in rural and underserved areas can be achieved through novel technical innovations such as telemedicine, which enhances the process of service delivery. By implementing these and other policy recommendations, it is possible to reduce the spatial mismatch between healthcare providers and patients in rural areas and improve access to primary care. These efforts hold great promise for enhancing the health and well-being of rural residents. The findings of our study underscore the importance of considering alternative theoretical frameworks in order to better understand the complex relationships between social, economic, and spatial factors in shaping access to essential services. Further research is needed to fully elucidate these relationships and to develop effective policy interventions to address disparities in access to primary medical care.
References
- Apparicio P, Abdelmajid M, Riva M, Shearmur R. Comparing alternative approaches to measuring the geographical accessibility of urban health services: Distance types and aggregation-error issues. Int J Health Geogr. 2008;7(1):1-4.
[Crossref] [Google Scholar] [PubMed]
- Fone DL, Christie S, Lester N. Comparison of perceived and modelled geographical access to accident and emergency departments: a cross-sectional analysis from the Caerphilly Health and Social Needs Study. Int J Health Geogr. 2006;5(1):1-10.
[Google Scholar] [PubMed]
- Grumbach K, Vranizan K, Bindman AB. Physician supply and access to care in urban communities. Health Affairs. 1997;16(1):71-86.
[Crossref] [Google Scholar] [PubMed]
- Luo W, Qi Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health & place. 2009;15(4):1100-1107.
[Crossref] [Google Scholar] [PubMed]
- Shah TI, Clark AF, Seabrook JA, Sibbald S, Gilliland JA. Geographic accessibility to primary care providers: Comparing rural and urban areas in Southwestern Ontario. The Can Geogr. 2020;64(1):65-78.
- Arcury TA, Preisser JS, Gesler WM, Powers JM. Access to transportation and health care utilization in a rural region. The J Rural Health. 2005;21(1):31- 38.
[Crossref] [Google Scholar] [PubMed]
- Laditka JN, Laditka SB, Probst JC. Health care access in rural areas: Evidence that hospitalization for ambulatory care-sensitive conditions in the United States may increase with the level of rurality. Health & place. 2009;15(3):761-770.
[Crossref] [Google Scholar] [PubMed]
- McGrail MR, Humphreys JS. The index of rural access: An innovative integrated approach for measuring primary care access. BMC Health Serv Res. 2009;9(1):1-2.
[Crossref] [Google Scholar] [PubMed]
- McGrail MR, Humphreys JS. Measuring spatial accessibility to primary health care services: Utilising dynamic catchment sizes. Appl Geogr. 2014;54:182-188.
- Hausdorf K, Rogers C, Whiteman D, Newman B, Coxeter P, Youl P et al,. Rating access to health care: Are there differences according to geographical region? Aust J Public Health. 2008; 32(3):246-249.
- Champagne F, Contandriopoulos AP, Ste-Marie G, Chartrand E. L’accessibilité aux services de santé et aux services sociaux au Québec. 2018:1-48.
- Salze P, Banos A, Oppert JM, Charreire H, Casey R, Simon C et al,. Estimating spatial accessibility to facilities on the regional scale: an extended commuting-based interaction potential model. Int J Health Geogr. 2011;10:1-6.
[Crossref] [Google Scholar] [PubMed]
- Farrington J, Farrington C. Rural accessibility, social inclusion and social justice: Towards conceptualisation. J Transp Geogr. 2005;13(1):1-2.
- Al-Taiar A, Clark A, Longenecker JC, Whitty CJ. Physical accessibility and utilization of health services in Yemen. Int J Health Geogr. 2010;9(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- Sibley LM, Weiner JP. An evaluation of access to health care services along the rural-urban continuum in Canada. BMC Health Serv Res. 2011;11(1):1-1..
[Crossref] [Google Scholar] [PubMed]
- Jordan H, Roderick P, Martin D, Barnett S. Distance, rurality and the need for care: Access to health services in South West England. Int J Health Geogr. 2004;3(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Loccoh EC, Joynt Maddox KE, Wang Y, Kazi DS, Yeh RW, Wadhera RK. Rural-urban disparities in outcomes of myocardial infarction, heart failure, and stroke in the United States. J Am Coll Cardiol. 2022;79(3):267-279.
[Crossref] [Google Scholar] [PubMed]
- Garnelo L, Parente RC, Puchiarelli ML, Correia PC, Torres MV, Herkrath FJ. Barriers to access and organization of primary health care services for rural riverside populations in the Amazon. Int J Equity Health. 2020;19(1):1-4.
[Crossref] [Google Scholar] [PubMed]
- Wang L, Wu C, Zhao S. A Review of Spatial Mismatch Research: Empirical Debate, Theoretical Evolution and Connotation Expansion. Land. 2022;11(7):1049.
- Wang L, Guruge S, Montana G. Older immigrants’ access to primary health care in Canada: A scoping review. Can J Aging. 2019;38(2):193-209.
[Crossref] [Google Scholar] [PubMed]
- Coughlin SS, Clary C, Johnson JA, Berman A, Heboyan V, Benevides T et al,. Continuing challenges in rural health in the United States. J Environ Health Sci. 2019;5(2):90.
- Jensen L, Monnat SM, Green JJ, Hunter LM, Sliwinski MJ. Rural population health and aging: toward a multilevel and multidimensional research agenda for the 2020s. Am J Public Health. 2020;110(9):1328-1331.
[Crossref] [Google Scholar] [PubMed]
- Caldwell JT, Ford CL, Wallace SP, Wang MC, Takahashi LM. Racial and ethnic residential segregation and access to health care in rural areas. Health & place. 2017;43 (1):104-12.
[Crossref] [Google Scholar] [PubMed]
- Neely AH, Ponshunmugam A. A qualitative approach to examining health care access in rural South Africa. Soc Sci Med. 2019;230 (1):214-221.
[Crossref] [Google Scholar] [PubMed]
- Xu F, Zhen F, Qin X, Wang X, Wang F. From central place to central flow theory: An exploration of urban catering. In Tourism Places in Asia. 2021:121-142. Routledge.
- Liu L. China's dusty lung crisis: Rural-urban health inequity as social and spatial injustice. Soc Sci Med. 2019;233:218-228.
[Crossref] [Google Scholar] [PubMed]
- Shi L, Wurm M, Huang X, Zhong T, Taubenböck H. Measuring the spatial hierarchical urban system in China in reference to the Central Place Theory. Habitat Int. 2020;105(2):102264.
- Banerjee S. Determinants of rural-urban differential in healthcare utilization among the elderly population in India. BMC Public Health. 2021;21(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- Rauhut D, Humer A. EU Cohesion Policy and spatial economic growth: Trajectories in economic thought. Eur Plan Stud. 2020;28(11):2116-33.
[Crossref] [Google Scholar] [PubMed]
- Aljassim N, Ostini R. Health literacy in rural and urban populations: A systematic review. Patient Educ Couns. 2020;103(10):2142-2154.
- Cyr ME, Etchin AG, Guthrie BJ, Benneyan JC. Access to specialty healthcare in urban versus rural US populations: a systematic literature review. BMC Health Serv Res. 2019;19(1):1-7.
[Crossref] [Google Scholar] [PubMed]
- Kompil M, Jacobs-Crisioni C, Dijkstra L, Lavalle C. Mapping accessibility to generic services in Europe: A market-potential based approach. Sustain Cities Soc. 2019;47(1):101372.
- Palozzi G, Schettini I, Chirico A. Enhancing the sustainable goal of access to healthcare: Findings from a literature review on telemedicine employment in rural areas. Sustainability. 2020;12(8):3318.
- Potter AJ, Natafgi N, Ullrich F, MacKinney AC. Perceptions of the benefits of telemedicine in rural communities. Perspect Health Inf Manag. 2016:1.
- Singh K. Growth pole theory by perroux. Pan Geography. 2022.
- Williams J, Petersen N, Stoler J. Characterizing the spatial mismatch between intimate partner violence related healthcare services and arrests in Miami-Dade County, Florida. BMC Public Health. 2018;18(10):1-10.
[Crossref] [Google Scholar] [PubMed]
Citation: Simoneau C (2023) Evaluating the Spatial Mismatch Hypothesis: A Comprehensive Analysis of Access to Primary Care Physicians and Healthcare Disparities in Eastern Quebec. Health Care Curr Rev.11:371.
Copyright: © 2023 Simoneau C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

