Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Publons
- International committee of medical journals editors (ICMJE)
- Geneva Foundation for Medical Education and Research
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2021) Volume 24, Issue 9
Establishing De Novo, a Consultation-Liaison Psychiatry (CLP) Service in a Tertiary Hospital â Practical Considerations and Challenges.
Nawal Nasser*Received: 07-Jun-2021 Published: 28-Jun-2021
Abstract
Consultation-liaison psychiatry (CLP), also known as psychosomatic medicine, is a subspecialty of psychiatry that focuses on the care of patients with comorbid psychiatric and general medical/surgical conditions. CLP deals with the understanding and advancement of medical science, education, and the provision of healthcare for medically ill patients. There is a significant benefit in integrating inpatient CLP services. It facilitates diagnosis and management of patients with complex comorbid psychiatric and general medical conditions. Patients and their physicians perceive CLP services as destigmatizing, and often as a mean of ensuring optimal continuity of care. There are practical considerations, advantages and challenges that need to be considered when establishing a CLP service in any general hospital setting. Advantages include the provision of specialized multi-professional and holistic patient care which helps to shorten length of stay and facilitates a more coordinated approach to complex cases. Inpatient liaison Psychiatrists play a major role in collaborating with the medical/surgical teams to provide a strong focus on education and training of various medical/surgical teams. The phenomenology of somatization disorders, interactions of biopsychosocial factors, and the effectiveness of CLP interventions could yield potential collaborative research areas between liaison psychiatrists and the medical/surgical teams. The inpatient CLP service will require additional resource allocation to succeed otherwise it often will get encumbered by unpredictable schedules and variable numbers of consultations. These challenges could create obstacles in the path of the early-career psychiatrist (ECP) and foster an environment that may lead to dissatisfaction and burnout.
Keywords
Consultation-liaison psychiatry; Psychosomatic medicine; Tertiary hospital
Introduction
Over the past two decades research in psychiatry has identified Consultation-Liaison Psychiatry (CLP) as “The guardian of holistic approach to the patient” [1], underlining its pre-eminent role in management of patients who are admitted to a general hospital. The CLP objectives and operating procedures have evolved in recent years from administration of psychiatric treatment [2] to integrating therapy [3] into the bio-psychosocial model along the lines of the recommendation from an editorial in the Lancet “No health without mental health” [4]. Hospital staff is confronted daily by physical/psychiatric multi-morbidity [5] with its extensive costs of suffering for patient and consumption of medical and economic resources [3]. It is worth noting that psychiatric disorders, even when sub-clinical [6], worsen outcome, lengthen hospital stays and are associated with increased mortality and use of health service resources [7,8].
There is ample evidence in the literature that supports establishing inpatient Consultation Liaison Psychiatry (CLP) Services in hospitals around the world [9]. Findings indicate that implementing CLP with an emphasis on clinometric rather than psychometric approaches, especially in a multidisciplinary context and specifically for complex cases, on medical/surgical/ obstetrics-gynecology wards, yields holistic health benefits [9].
Establishing de novo CL Psychiatry Services has been studied in various parts of the world [10-13]. There are differences and variations among countries around the world with respect to access to CL Psychiatry Services in general hospitals, as well as in models of CL Psychiatry Services delivery. For example, various models of CL Psychiatry practice (referred to as ‘outpatient style’, ‘sick-call style’, ‘make-rounds style’, ‘on-the-ward style’) have been described in Japan [12].
Evidence suggests that the presence of specialized CL services does in fact help to shorten length of stay and facilitates a more coordinated approach to complex cases. As a result, several countries, including some in the Gulf region [13,14], have started to implement inpatient CL Psychiatry Services in general hospitals. Their experience suggests that there is a substantial need for inpatient CL Psychiatry which results in improving the accuracy in diagnosing and treating psychiatric illnesses in medically ill inpatients [13,14].
In Oman specifically, and in the Gulf region generally, there are no comprehensive statistics available on overall levels of activity, or resources allocated to CLP Services in general hospitals. General psychiatrists on call, who cover the services as needed, cover CLP services in the Ministry of Health General Hospitals.
The main objective of this communication is to report on the practical considerations and challenges associated with establishing de novo, a CLP service in a tertiary hospital.
Establishing CLP service-the rationale
The prevalence of co-morbid psychiatric disorders among patients in general hospitals is extremely high. Many of these problems typically go undiagnosed and untreated [11,15]. In the absence of effective intervention, patients’ response to medical treatment, quality of life and functioning as well as utilization of services, length of hospital stays, hence the cost of health care will be negatively affected [10,11,15,16]. Improvement in diagnosis and management of mental health conditions in general hospitals can significantly reduce the scale and cost of these problems [9,11]. Given these epidemiological considerations, there is a need for dedicated and specialized inpatient CLP services in general hospitals [11].
There is a current trend, informed by research and practice [11, 14,15], toward emphasizing the importance of collaboration among different medical specialists, and allied professionals in the treatment of patients with complex comorbidities. This includes combined medical-psychiatric consultation and longitudinal care in order to provide integrated and holistic care. CL Psychiatry plays a vital role in this endeavor and helps bridge the gap between the physical and mental health needs of patients to optimize health care and lower its cost [16].
Inpatient CL Psychiatry service affords numerous clinical advantages by facilitating the management of patients with complex comorbidities. It has a significant role in assessing comorbid physical and psychiatric disorders accurately and educating clinicians about the impact of these symptoms and the principals involved in their treatment [13,15,16].
There is evidence in the literature that suggests in some medical/surgical settings a significant proportion of patients suffer clinically significant mood disorders that were missed, hence they remained undiagnosed and untreated during hospitalization.
The standard of care for these patients should have included referral to CLP service.
The benefits of establishing CL services
There are numerous benefits discussed in the literature that support developing inpatient CLP service within the hospital system.
An important function of CLP service is the identification of patients that require complex bio psychosocial care. These are the patients that require an effective interdisciplinary team approach for their care.
Such patients need to be identified at admission, or early in their hospitalization, in order to optimize coordination and management necessary in their care.
There are validated tools such as (COMPRI-Complexity Prediction Instrument) and INTERMED available to CLP team that are useful in identifying needs of these complex cases [17,18] either at the time of admission or among the outpatient population.
Practical implementation of CLP service
Fulltime consultation-liaison psychiatrists are essential in establishing clear guidelines and in determining what constitutes optimal interventions for patient in need of complex care.
In addition, psychologists and social workers, with their expertise and interests, will greatly contribute to patients’ quality of life, and decrease the burden of care of such a highly complex patient population.
A liaison nurse is another essential professional necessary for a well-functioning interdisciplinary CLP service [10, 12].
The liaison nurse provides the needed support to nursing staff on medical/surgical floors inside the hospital and facilitates organizing mental health follow-up on discharge or transfer to psychiatric facilities.
Finally, in order to establish a viable CLP Service, it would be necessary to ensure adequate physical resources to support the team. A suggested flowchart of how such service could be embedded in the care of patients is illustrated in Figure 1.
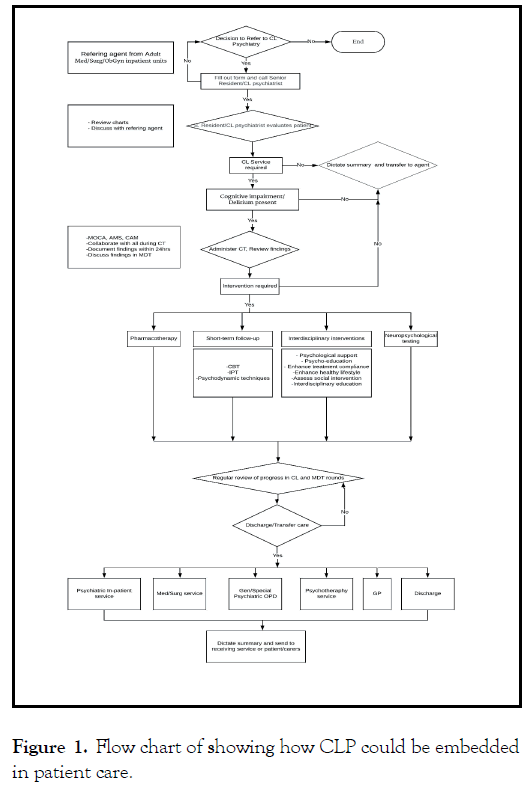
Figure 1: Flow chart of showing how CLP could be embedded in patient care.
Embedding education, training and research
With respect to medical education, there is authoritative evidence-base that supports integrating inpatient CLP into medical and surgical floors [10]. Liaison Psychiatry has been a core-training requirement of Residency Programs in certain parts of the world. There were indications that medical students who had exposure to CLP training were noted to have gained greater knowledge of and a positive attitude towards psychiatry, which might encourage recruitment to the profession [10,12]. Secondly, inpatient CL Psychiatrists may play a major role in collaborating with the medical team to provide a strong focus on education and training of various medical/surgical teams. This training could be on how to implement basic psychotherapeutic interventions that could facilitate patients’ coping with the stress of medical illness. In this manner, the importance of psychological factors will be more widely recognized and embedded in the routine care of patients.
In addition, many areas in medicine lend themselves to developing exciting research questions in the context of CLP. Psychiatric disorders and psychological factors in medical practice, the medical care process, the phenomenology of somatization disorders (somatoform disorders in ICD-10), interactions of bio-psychosocial factors, and the effectiveness of CL interventions are all areas of interest and could yield potential research questions for CLP.
Challenges in establishing CLP service
There could be several challenges associated with establishing de novo inpatient CLP Services. Studies indicate that in hospitals where CLP service exists, referral rates are very low [19]. Some factors that contribute to low referral rates include the fact that doctors on medical/surgical wards may not pick up patients’ emotional disturbances, and that many physicians are reluctant to use psychiatric services [19]. As a result, many patients could be missed, thus not getting the benefits of needed psychiatric assessment and appropriate intervention [20].
Baseline staffing of CL Psychiatry Services in general hospitals has been described in the literature [21,22]. There are multiple factors that determine efficient sizing of a CL Service. These include the institution’s number of beds, its level of acuity of illnesses, the presence/absence and needs of trainees that it hosts, and the financial constraints of the department and the institution. In order to provide benchmarks for both academic and non-academic CL Services, national survey data are needed from different settings.
The inpatient CLP service is often encumbered by unpredictable schedules, variable numbers of consultations from week to week, and high-volume days. These challenges can create obstacles in the path of the Early-Career Psychiatrist (ECP) and foster an environment that may lead to dissatisfaction and burnout. On another level, a new CLP service will require additional resource allocation that needs to be justified [21,22]. Therefore, evidence of its potential benefits on issues such as Length of Stay (LOS) and quality of patient care should be forcefully articulated if the hospital administration is to support the creation of such service [23,24].
Conclusion
In summary, there are significant benefits in integrating inpatient CLP Services. It facilitates timely diagnosis and management of complex cases. The liaison service helps to establish professional contact with medical/surgical and nursing colleagues, reduce mental health stigma, broaden the understanding of psychological reactions to physical disease and of psychogenic disorders, reduce unnecessary investigations, and provide more comprehensive patient care. In addition, CLP service could facilitate early detection of mental health problems in patients’ and provide support to the medical/surgical staff in caring for such patients.
REFERENCES
- Ajiboye PO. Consultation-liaison psychiatry: The past and the present. Afr J Med Med Sci. 2007;36(3):201-205.
- Zumbrunnen R. Psychiatrie de liaison. La consultation psychiatrique à l’hôpital général. Coll Médicine et psychothérapie. Paris: Masson; 1992.
- Smith GC. From consultation-liaison psychiatry to integrated care for multiple and complex needs. Aust N Z J Psychiatry. 2009;43(1):1-2.
- Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370(9590):859-877.
- Smith GC. Challenges for psychotherapy and psychoanalysis. Aust J Psychother. 2006;25:32-55.
- Ormel J, Vonkorff F, Oldenhinkel AJ, Simon G, Tiemens BG, Ustun TB. Onset of disability in depressed and non-depressed primary care patients. Psychol Med. 1999; 29(4):847-853.
- Saravay SM. Psychiatric comorbidity and length of stay in the general hospital: A critical review of outcome studies. Psychosomatics. 1994;35(3):233-252.
- Chilshom D, Dichr P, Knap M, Patrick D, Treglia M, Simon G. Depression status, medical comorbidity and re source costs: Evidence from an international study of major depression in primary care. Br J Psychiatry. 2003;183(2):121-131.
- De Giorgio G, Quartesan R, Sciarma T, Giulietti M, Piazzoli A, Scarponi L, et al. Consultation-liaison psychiatry–From theory to clinical practice: An observational study in a general hospital. BMC Res Notes. 2015; 8(1):1-6.
- Desan PH, Zimbrean PC, Weinstein AJ, Bozzo JE, Sledge WH. Proactive psychiatry consultation services reduce length of stay for admissions to an inpatient medical team. Psychosomatics. 2011; 52(6):513-520.
- Lloyd GG. Liaison psychiatry from a British perspective. Gen Hosp Psychiatry. 1980;2(1):46-51.
- Kurosawa H, Iwasaki Y, Watanabe N, Nakamura K, Kishi Y, Huse R. The practice of consultation-liaison psychiatry in Japan. Gen Hosp Psychiatry. 1993; 15(3):160-165.
- Fido AA, Mughaiseeb AL. Consultation liaison psychiatry in a Kuwaiti general hospital. Int J Soc Psychiatry. 1989;35(3):274-279.
- Aljarad AM, Al Osaimi FD, Al Huthail YR. Accuracy of psychiatric diagnoses in consultation liaison psychiatry. J Taibah Univ Medical Sci. 2008;3(2):123-128.
- Mhaolain AN, Butler JS, Magill PF, Wood AE, Sheehan J. The increased need for liaison psychiatry in surgical patients due to the high prevalence of undiagnosed anxiety and depression. Ir J Med Sci. 2008;177(3):211-215.
- Andreoli PB. A systematic review of studies of the cost-effectiveness of mental health consultation-liaison interventions in general hospitals. Psychosomatics. 2003;44(6):499-507.
- Huyse FJ, De Jonge P, Slaets JP, Herzog T, Lobo A, Lyons JS, et al. COMPRI-An instrument to detect patients with complex care needs: Results from a European study. Psychosomatics. 2001;42(3):222-228.
- Huyse FJ, Lyons JS, Stiefel FC, Slaets JP, De Jonge P, Fink P, et al. “INTERMED”: A method to assess health service needs. Gen Hosp Psychiatry. 1999;21(1):39-48.
- Alqataybi H, Almaqbali M, Asiri WA, Martin R, Alsinawi H. Patterns of referrals to consultation-liaison psychiatry in a tertiary care hospital in Oman. Arab J Psychiatry. 2018; 29:17–23
- Chen KY, Evans R, Larkins S. Why are hospital doctors not referring to consultation-liaison psychiatry?-A systemic review. BMC Psychiatry. 2016;16(1):1-2.
- Kunkel EJ, Del Busto E, Kathol R, Stern TA, Wise TN, Stoddard II FR, et al. Physician staffing for the practice of psychosomatic medicine in general hospitals: A pilot study. Psychosomatics. 2010;51(6):520-527.
- Holmes A, Handrinos D, Theologus E, Salzberg M. Service use in consultation-liaison psychiatry: Guidelines for baseline staffing. Australas Psychiatry. 2011;19(3):254-258.
- Muskin PR, Skomorowsky A, Shah RN. Co-managed care for medical inpatients, CL vs C/L psychiatry. Psychosomatics. 2016;57(3):258-263.
- Gopalan P, Azzam PN, Ackerman KD. The early-career consultation psychiatrist: Administrative innovations in psychosomatic medicine. Psychosomatics. 2015;1(56):103-105.
Citation: Nasser N (2021) Establishing de novo , A Consultation-Liaison Psychiatry (CLP) Service in a Tertiary Hospital-Practical Considerations and Challenges. J Psychiatry. 24: 481
Copyright: © 2021 Nasser N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

