Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
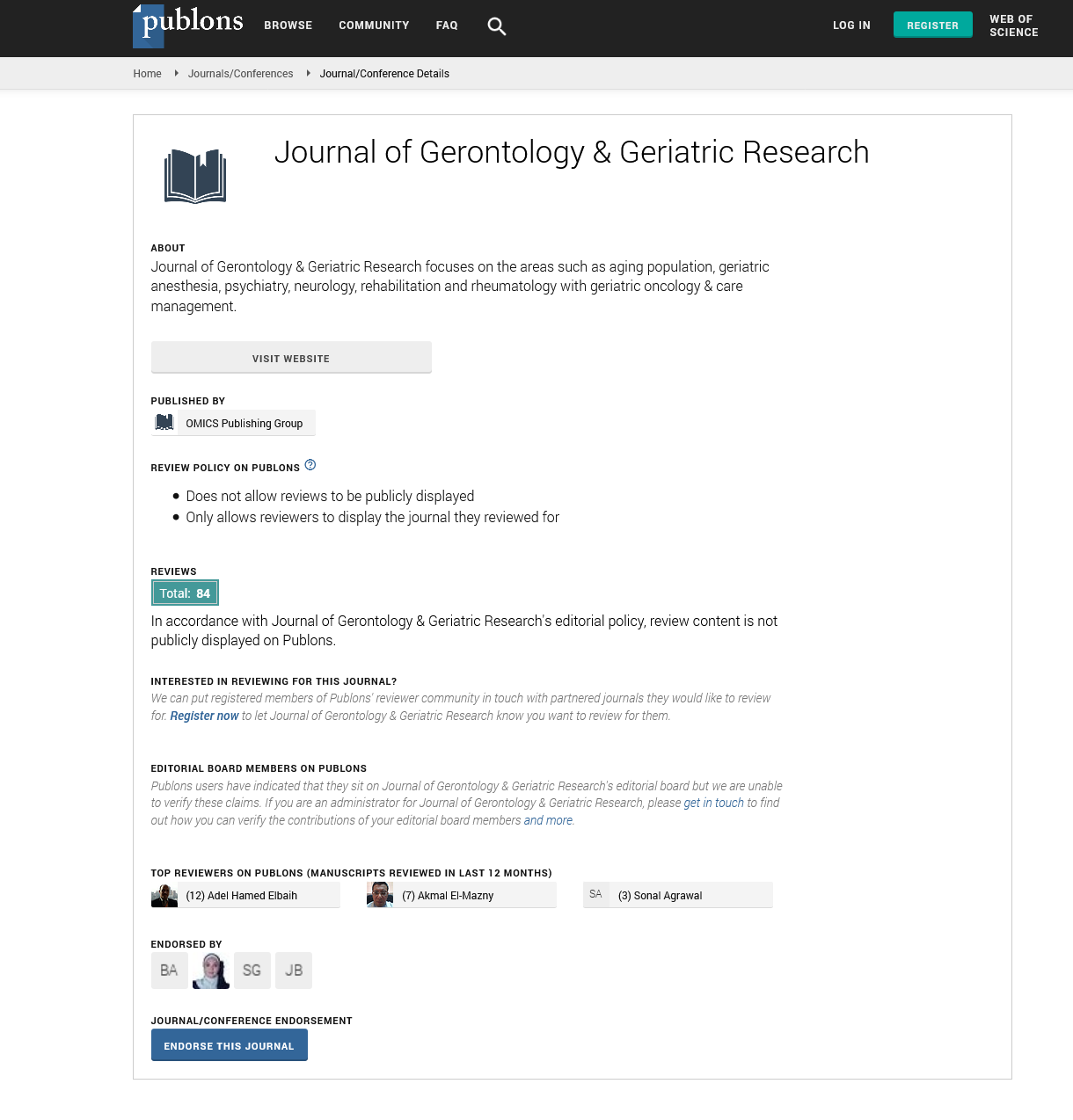
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2021) Volume 10, Issue 11
Epidemiology of Polypharmacy in Geriatric Patients
Sonia Puri*Received: 08-Nov-2021 Published: 29-Nov-2021, DOI: 10.35248/2167-7182.21.10.582
Perspective
The term polypharmacy is derived from the ancient Greek words 'pols' (many) and 'pharmakea' (drug usage). From a strictly language standpoint, this broad connotation is mirrored in the fact that there is no agreement on a clinical definition of polypharmacy. Should the word, for example, refer to just concurrent pharmaceuticals as opposed to successive medications, cover both short-term and long-term therapy, be limited to prescription-only medications, or include non-pharmacological products? These variables make it difficult to adequately measure the scope of the problem or make comparisons between health-care systems or locales.
Polypharmacy is the concurrent use of several medications by a single person. It frequently reflects the coexistence of many health issues, such as chronic diseases (such as diabetes and heart failure), acute ailments (such as infections), and sensations (such as pain) that worsen with age. When evidence-based prescription recommendations established for the care of a single disease are applied to persons with multimorbidity, complicated medication regimens might arise. As a result, the number of medications is larger among older persons than among middle-aged adults. If several medication treatments enhance health and quality of life, they may be clinically justified. However, it presents significant issues to doctors since many older persons are exposed to polypharmacy after the age at which medication treatment is no longer helpful.
In older persons, polypharmacy raises the risk of adverse drugrelated events. For starters, a greater number of medicines increases the potential of dangerous drug–drug interactions. Second, since ageing is accompanied with physiological changes (e.g., weight loss, worsening of liver and renal excretion, reduction in cardiac output, body composition remodelling) that render older persons more susceptible to hazardous medication responses. Third, the high frequency of chronic multimorbidity in the elderly increases the possibility of drug–disease interactions. Polypharmacy in older adults: the prevalence and types of medications they take. In addition, the prevalence and sorts of unneeded medications will be discussed in this section. The epidemiology of unfavourable health outcomes associated with polypharmacy will be discussed in the following section. Following that, evidence from randomised, controlled intervention trials including older persons with polypharmacy will be provided, demonstrating how medication use can be improved. The final portions will include an expert opinion and a conclusion.
The number of medications that surpass a simple numeric threshold is one of the most often used definitions of polypharmacy in practise. Polypharmacy is a continuum, and dichotomizing in this way is of minimal utility in diagnosing drug-related problems, despite its simplicity. Furthermore, due to the increased usage of medications in modern practise, formerly applicable cut-offs such as "five or more pharmaceuticals" may no longer be acceptable. According to the Centres for Disease Control and Prevention, patients 65 and over are the greatest consumers of prescription and non-prescription drugs in the United States, with prescription and non-prescription medication consumption having more than doubled since 1990 and continuing to climb (CDC).
Elderly Americans take one-third of all prescription prescriptions written each year, but accounting for less than a quarter of the population. The relatively high rates of drug usage among elderly patients, as well as a variety of other factors, contribute to the higher prevalence of medication-related morbidity and mortality in this group. Physiologic changes associated with ageing, such as decreased renal clearance, decreased hepatic function, decreased total body water and lean body mass, and age-related vision and hearing loss, are all significant contributors. For many elderly people, several of these changes might contribute to changes in the pharmacokinetics of drugs, such as altered distribution, metabolism, and elimination. Pathophysiologic changes associated with disease, the prevalence of chronic disease and medical comorbidities, communication hurdles, and healthcare delivery involving numerous prescribers are all significant factors.
Citation: Sonia P (2021) Epidemiology of Polypharmacy in Geriatric Patients. J Gerontol Geriatr Res. 10: 582
Copyright: © 2021 Sonia P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.