Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2024) Volume 21, Issue 6
Efficacy of Delivery Fees Exemption Policy on Utilization of Maternity Services at Nakuru County Referral Hospital
Gacaga Peter Mungai* and Nicholus MuraguriReceived: 28-Sep-2020, Manuscript No. CMCH-24-6632; Editor assigned: 01-Oct-2020, Pre QC No. CMCH-24-6632 (PQ); Reviewed: 15-Oct-2020, QC No. CMCH-24-6632; Revised: 01-Aug-2024, Manuscript No. CMCH-24-6632 (R); Published: 29-Aug-2024, DOI: 10.35248/2090-7214.24.21.500
Abstract
The reduction and elimination of pregnancy-related mortality remain a challenge in most low income countries. For this reason, many African countries have either reduced or eliminated delivery fees to promote health facility delivery service utilization. Healthcare seeking behavior is a central issue in service delivery. Cost has been highlighted as a major hindrance to utilization of medical services especially among the poor people. It has been shown that removal or reduction of user fees results to increased utilization of services. However, some studies have shown the opposite to be true. Following the free maternity services policy in Kenya, uninterrupted time series study was conducted in Nakuru county referral hospital to examine the effects of the policy on utilization of maternity services at the hospital and the effects on maternal and neonatal deaths. The study aimed at examining the efficacy delivery fees exemption policy on utilization of maternity services at Nakuru county referral hospital. Data was collected from facility-based records using a predesigned standard data extraction form. The study used Interrupted Time Series Analysis (ITSA), a strong longitudinal quasi-experimental design with a single group to assess the effects of the free maternity service policy to maternal health. The three indicators were observed 24 months pre (June 2011-May 2013) and 24 months post (June 2013-May 2015) free maternity service policy implementation, giving a total of 48 observations. There was a statistically significant increase in the number of skilled deliveries, significant reduction in neonatal mortality rates and a non-significant reduction in the maternal mortality ratio. These findings suggest that cost significantly limits access to skilled deliveries in Kenya thus the free maternity policy can successfully promote utilization of facility deliveries. However, free maternity alone cannot address maternal and neonatal mortalities thus there is needed to address other determinants of maternal and neonatal deaths such as the health service infrastructure and cultural practices.
Keywords
Infant mortality rate; Maternal mortality rate; Maternal mortality ratio; Neonatal mortality rate; Obstetric complication; Skilled delivery; User fee
Introduction
According to Dzakpasu S et al., user fees are charges levied at the point of use of any aspect of health services. User fees for health services were introduced or substantially increased in African countries following the 1987 joint World Health Organization/ United Nations Children’s Fund Bamako Initiative whose aim was to address severe problems in the financing of maternity care.
User charges for essential drugs were also introduced to generate funds to improve the quality of health services and equity in access to these services [1]. However, user fees have seldom produced these intended benefits Gilson L, et al. Instead, they have been a significant barrier to access of maternal health care services in Kenya. Studies done between 2003 and 2006 in three African countries found that the mean cost of a normal or a complicated delivery in Kenya was US $18.4 compared to US $7.9 and US $5.1 for Burkina Faso and Tanzania respectively Perkins M, et al. This has made user fees a prohibitive barrier to access to essential services even in Kenya El-Khoury M, et al.
Health is a fundamental commodity essential to people’s wellbeing and for their active participation in development. Majority of Kenya population are uninsured, medical care is usually procured through out of pocket payments. This is common in many developing countries as a result of the health sector restructuring done in early 90s which led to abolishment of free medical care and introduction of user fee in all government health facilities. With 45.9% of Kenyans living below the poverty line, many often delay seeking medical care due to the associated financial burden. Oftentimes appropriate medical care is sought when all other options fail; sometimes this is too late especially for pregnant women. High rates of maternal and child mortality and morbidity are the leading contributors of disease burden in Kenya. Studies have shown that delays in seeking medical care are partly responsible for the high maternal and child mortality [2].
To address the situation, the government of Kenya introduced a policy exempting user fee for antenatal and maternity services in 2013. The policy requires all public health facilities to provide antenatal and maternity services without charging the clients. The bills are then submitted to the government for reimbursement. However, few studies have been conducted to assess the policy impact in Kenya, with mixed results. According to the World Health Organization, globally, approximately over 800 women lose their lives daily due to preventable causes related to pregnancy and childbirth. Over 99% of all deaths occur in developing countries. It is estimated that for every 100,000 live births about 360 women lose their lives due to pregnancy related complications in Kenya. This translates to over 5000 deaths every year, which is 2% of the global burden. Most of the deaths are due to preventable causes which can be prevented especially through skilled deliveries [3].
Realizing the undesirable effects of the user fee policy, many countries have either reduced or removed the user fees for maternity care. User fee on health care services was introduced in Kenya in 1989, where the fee was to support general operations and management of public health facilities. Introduction of these fees was criticized as a move that would advance social exclusion and inequity in accessing health care services leading to its suspension in the year 1990. Owing to the economic limits within the country, user fees on health care services was later re-introduced in 1991 with exemptions applicable to children under-five including immunization charges, treatment for malaria, tuberculosis and sexually transmitted diseases [4]. In 2004, the government adopted the 10/20 policy where a minimal fee of KES 10 and 20 for registration was charged at the public dispensaries and health centers respectively. In July 2013, Kenya introduced a health policy allowing more women to access free maternity services in government health facilities. It was anticipated this would increase facility-based deliveries and contribute to reduced infant and maternal mortality.
The introduction of free maternity services by the government of Kenya in July 2013 meant that pregnant women delivering in health facilities were to be exempted from paying hospital user fees. Subsequently, health facilities are required to claim for reimbursement from the government for each delivery conducted. Every year, about 4 billion shillings are reimbursed for facility-based deliveries. However, it is not clear if introduction of free maternity services had had any impact on utilization of maternal health services and related health outcomes. Further it is not clear what the anticipated increment in deliveries in health facilities will have on the quality of care provided to women in labor. Quality of care can be reflected by changes in maternal and prenatal (newborn) death rates. Without knowledge of the impact, the government may continue spending on free maternity services while not making progress towards the SDGs. It is against this background that the study was undertaken to fill the missing knowledge gap by examining the effect of implementing free maternity services in Kenya: Case of Nakuru county referral hospital [5].
Materials and Methods
According to Dzakpasu P et al., in a systematic literature review, introduction of user fees decreases service uptake for both antenatal and maternity care. Removal of user fees on the other hand was noted to increase antenatal visits, facility-based deliveries and the number of facility managed complications. However, in some settings, there was an increase in maternal deaths following fee removal possibly due lack of sufficient resources to cope with the increased workload [6].
A similar study based on statistics and health survey (DHS) data from ten sub-Saharan African countries found that abolishing user fee resulted to a 3.1/100 live births increase in facility-based deliveries and a reduction 2.9/1000 births decline in neonatal deaths (i.e., 5% increase in facility-based deliveries and 9% reduction in neonatal deaths). However, despite the fear that facilities would deliver more women through caesarean in order to attract higher reimbursements from the governments, the survey did not find out any association [7].
This resulted to a rapid decline in unintended pregnancies from 12.8 per 100 women-years during the first year postpartum to 2.2 per 100 women-years, lower than that of permanent residents which stood at 3.8 per 100 women-years. This clearly demonstrates how cost hinders women’s access to essential services. In a cross-sectional survey conducted in Ethiopia covering 751 health facilities, it was observed that although the government policy is to provide free Emergency Obstetric and Newborn Care (EmONC) services, over half of the health facilities (65%) were charging a user fee for normal delivery with 20% of the facilities requiring that patients pay upfront. Perhaps due to this burden, only 6.6% of women gave birth in health facilities [8]. The case fatality rate was lower in facilities that charged user fees (3.8% versus 7.1%). On average, facilities that charged user fee had more delivery beds, more deliveries, more complications and a higher ratio of skilled attendants to patient.
It was observed that facilities charging user fees had more deliveries than those providing free maternity implies that there are other barriers hindering women from delivering under skilled attendance. The authors note that transport cost, food and lodging for accompanying relatives are among the notable barriers [9].
In Laos (southeast Asia), removing user fee resulted to an overall increase in the number of facility-based deliveries in both control and intervention areas. However, while the control areas only had a 40% increase, the number of facility-based deliveries tripped in the intervention group. This clearly displays the impact of the financial burden associated with facility-based deliveries. Elimination of user fee can therefore be an effective strategy for increasing facility-based deliveries and subsequent reduction in pregnancy related maternal and child mortality [10].
A study conducted in mali showed that despite the removal of user fees, richer women still accounted for more caesarean deliveries with women in the richest two quintiles accounting for 58% of all cesareans while only 27% were among women in the poorest two quintiles. Other studies have shown that removing user fees can worsen health outcomes especially if existing facilities cannot cope with the increased demand. This demonstrates that that fee exemption is necessary but not sufficient to ensure equality in access to care [11].
Penfold et al., observed that there is enough literature providing evidence that user fee removal for facility-based deliveries results in increased facility-based delivery rates but the evidence is weak studied fee exemptions for delivery care at public and mission facilities in Ghana, which were introduced in 2003. They conducted a household survey in 2 regions after the policy had been in place. There was a statistically significant increase (5 percentage points and 12 percentage points respectively) in rates of delivering in a health facility, comparing the period before and after policy implementation [12].
Witter et al. noted that there was some statistically significant evidence that user fee exemptions for caesarean sections resulted in increased caesarean section rates. The study conducted in Senegal reported a significant increase in caesarean section rates from 4.2% to 5.6% of facility-based deliveries over the one-year period after fees were removed. El-Khoury et al. analyzed data of the national health information system from Mali, which removed user fees for caesarean sections in 2005. The national caesarean rate increased significantly from 0.9% of estimated deliveries in 2005 to 2.3% in 2009; similar increases were apparent in each region of the country; pre-policy data was not available. It is important to note that neither study is able to address whether the C-sections were medically necessary but the increases observed put C-section rates after fee removal well within expected range for surgical deliveries of medical necessity.
Penfold et al., the literature provides evidence that user fee removal for facility-based deliveries results in increased facilitybased delivery rates but the evidence is weak studied fee exemptions for delivery care at public and mission facilities in Ghana, which were introduced in 2003.
They conducted a household survey in 2 regions after the policy had been in place for one (Volta region) or two years (Central region). Respondents reported a statistically significant increase (5 percentage points and 12 percentage points respectively) in recalled rates of delivering in a health facility, comparing the period before and after policy implementation. However, there was no comparison group.
This study was guided by social cognition models that posit that behavior change is motivated by certain beliefs and attitudes. The health belief model, self-efficacy model, theory of reasoned action, theory of planned behavior and the protection motivation theory are among the widely used social cognition models. The health belief model explains that an individual’s decision to seek medical care is determined by a combination of four variables: Perceived susceptibility/vulnerability to the risk, perceived severity/seriousness, perceived benefits, perceived barriers or costs. These act together with cues to influence the likelihood for action.
The Theory of Reasoned Action (TRA) on the other hand argues that most social behaviors are under volitional control thus the individual’s decision to act or not is dependent on one’s attitude towards the behavior and the perception of how others will react to his/her choice. The theory of planned behavior notes that there are behaviors that require more than will (Figure 1).
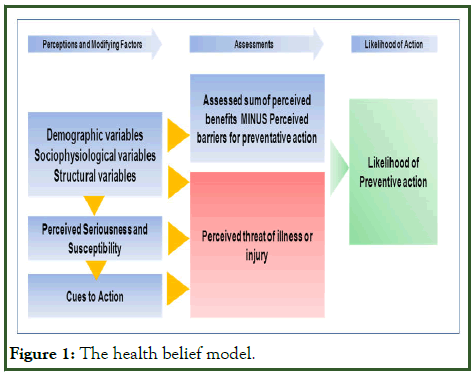
Figure 1: The health belief model.
The self-efficacy theory is very close to the health belief model. The model states that the two key determinants of behavior are perceived self-efficacy and outcome expectancies. The constructs in these two models relate closely to those in the protection motivation theory which explains that the motivation to protect oneself against a health threat is determined by vulnerability and severity, response efficacy or consumer satisfaction and perceived self-efficacy as demonstrated in Figure 2.
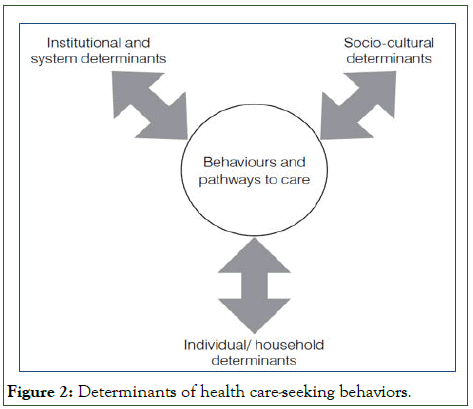
Figure 2: Determinants of health care-seeking behaviors.
Young et al., observed that like TRA, the choice-making model includes both individual perception and their social networks perception the perceptions of gravity and knowledge of home treatment. It observes that one is more likely to utilize a known more efficacious home remedy (based on referral and faith in the remedy) before visiting a medical practitioner. Basically, an individual will only utilize a treatment if they believe it is effective and accessible. Generally, the health behavior and health care utilization models have three factors in common: (1) Health care access including physical and social resources, (2) culture including values, practices and beliefs and (3) social networks. This is well summarized in the Cambodia health seeking behavior studies working paper where the authors conclude that behaviors and pathways to care are influenced by three key determinants as shown in figure below.
The study was conducted in Nakuru county, one of the fortyseven counties in Kenya. With a population of 2.2 million persons according to the 2019 housing and population census, Nakuru is the fourth most populous county in Kenya after Nairobi, Kakamega and Kiambu. Nakuru county was selected for the study because of its maternal health indicators, particularly uptake of maternal health services and maternal mortality. In 2013, Nakuru county had a maternal mortality rate of 374 per 100,000 live births and skilled delivery of 51%. It was ranked among the top four counties in Kenya with high maternal death burden by UNFPA in 2014 despite being one of the counties with the best infrastructure, high number of health workers and with 35% of its budget being allocated to health.
The study targeted all patient files at maternity between June 2011 and May 2015 which had a minimum of two data points collected pre-intervention and one post-intervention. There was no restriction on participants, language of study or type of outcome. Data were summarized using appropriate summary statistics. Thus, the study had 48 monthly data sets: 24 months before the policy and 24 months after the policy. To assess the utilization of maternity services in the pre and post program period, the study used 30% of total data from the period one and a half years prior to the implementation of the program (December 2011-May 2013) and the period one and a half years after the implementation of the program (June 2013-November 2014). Basing on the 30% of the total data as recommended by Mugenda, a total of 3600 files, 1800 from each period were reviewed.
Data was abstracted using a pre-tested data abstraction form. Data was limited to a period of 24 months prior to the introduction of free maternity services policy and 24 months after the introduction of the policy. A survey data abstraction form was used to collect information about women who delivered at Nakuru county referral hospital between January 2011 and December 2014. The information was collected from hospital anti-natal clinic register and maternity/delivery register to collect the required information for all the mothers who were recorded in the two registers during this period.
The study used Interrupted Time Series Analysis (ITSA), a strong longitudinal quasi-experimental design with a single group to assess the effects of the free maternity service policy to maternal health. The three indicators were observed 24 months pre (June 2011-May 2013) and 24 months post (June 2013- May 2015) free maternity service policy implementation, giving a total of 48 observations. Visual inspection of the data was done to check for any outliers, linear trends and data quality issues. Interrupted time series analysis of quarterly performance for the 3 indicators was performed using autoregressive integrated moving average models setting significance level at p<0.05. All analysis was done in SPSS with data consisting of monthly values for the three variables. Ordinary Least Squares (OLS) regression model with a time series specification (an intercept term, a trend term, a level change and a trend change) was used to check for serially correlated errors by plotting the graphs of the residuals from the OLS regression as well as generating the Autocorrelation and Partial Auto Correlation (ACF/PACF) plots. Significant and easily identifiable peaks at certain lags on the ACF/PACF plots were observed in 2 of the three variables.
Results
A total of 29,312 pregnant women attended Nakuru level 5 country referral hospital between June 2011and November 2014. Majority were aged between 30 and 49 years (41%), had 2 to 3 children (38%), had primary or no education (53%) and were not working (36%). Most respondents were christians (72%) predominantly residing in rural areas (55%). Overall, there were 75% more women who received care at the referral hospital 24 months post the policy period compared to similar period before the policy was instituted. The increase in service uptake was highest among elderly women with 2-3 children, low education, rural residents and the unemployed (Table 1).
| Indicator | Pre-policy (Jun 2011-May 2013) | Post-policy (Jun 2013-May 2015) | Change |
|---|---|---|---|
| Hospital deliveries | 10253 | 14392 | 40% |
| Live births | 9760 | 13999 | 43% |
| Maternal deaths | 67 | 80 | 19% |
| Neonatal deaths | 270 | 169 | -37% |
| Maternal mortality ratio/105) | 686.5 | 571.5 | -17% |
| Neonatal mortality rate (/1000) | 27.7 | 12.1 | -56% |
Table 1: Women attending maternity services at Nakuru county referral hospital.
There was a statistically significant increase in the number of skilled deliveries from 10,253 before policy implementation to 14,392 representing a 40% (95% CI: 39, 41%) increase. Analysis of deliveries indicated a declining trend prior to the policy (slope-14.52, p=0.16) and a significant increase after policy implementation (slope=49.16, p<0.05).
Stationary R2 yielded a value of 0.65 implying that 65% of the model was explained by the policy intervention. The mean absolute percentage error was 7.3 indicating that the values predicted by the model were on average, within 7.3% of the actual values (Table 2).
| Outcome | Pre-policy slope | Post-policy slope | Ljung-box |
|---|---|---|---|
| Institutional deliveries | -14.52 (p=0.16) | 49.16 (p<0.05) | 26.81 (p=0.05; df=17) |
| Maternal mortality ratio | -4.64 (p=0.07) | 2.74 (p=0.15) | 30.21 (p=0.03; df=17) |
| Neonatal mortality rate | 0.19 (p=0.52) | -0.24 (p<0.05) | 32.68 (p=0.23; df=17) |
Table 2: Trends in outcomes before and after the policy implementation.
Successful user fee policy implementation at scale required careful design, skilled management and careful oversight. Some countries had experienced problems with the initial implementation and medium-term support for user fee exemption policies, specifically relating to replacing lost fee revenue to health facilities and ensuring clear communication about the policy. Ghana had substantial problems in disbursing funds to health facilities. Many facilities eventually stopped implementing the fee exemptions because of shortfalls in supplies and drugs. In Senegal, there were insufficient delivery kits available to facilities in the first year of the policy and the distribution of kits did not mirror the needs of population. In general, reimbursing providers by giving them kits has been rife with challenges: Kits are much less flexible than cash in meeting needs of the facilities; they require transport and stock management and do not cover labour costs. In Burkina Faso, Ridde et al. concluded that the reduction of user fees was initiated before the groundwork was laid to make it a successful policy initiative. Confusion among health workers on the policy resulted in uneven implementation and there were insufficient funds to subsidize activities across all health centers.
Discussion
The study design allowed measurement of the effects of the policy in a real-world setting. However, being non-experimental, the strength of evidence and thus causality is limited owing to lack of a controlled environment. Nonetheless, the analytical approach enabled us to elicit compelling evidence on the effects of the policy. Further analysis should be done with the data disaggregated according to the various demographic dimensions. This may help the policy makers better understand the factors that may influence the performance of the policy. The results reported supported the hypothesis that user fee exemption lead to increased utilization of maternal health care. They also corroborate findings of the majority of evaluations that have shown increased utilization of health care after user fee removal. They underscored the importance of user fee exemption as a strategy for universal health coverage. An important implication of the results is that user fee exemption may not have the same importance for different types of maternal health services. This is inferred from the lack of significant effects for some variables and the significant positive effects for the other variables. The fact that the signs and statistical significance of the SLA coefficients were the same for corresponding utilization variables in the two sets of results shows the robustness of the primary set of results.
The percentage of pregnant women who make at least one ANC visit during pregnancy has been high in Kenya. The Demographic and Health Survey (MDHS) showed that it was 95% nationally while the MDHS showed that it rose to 99%. The data used in this study showed that, for CHAM health facilities with user fee exemption, it was 73% between 2003 and 2005 (before user fee exemption was introduced) and increased to 84% due to user fee exemption.
Conclusion
However, despite the effect of user fee exemption it still fell below the national average. For average ANC visits, the increase due to user fee exemption means that pregnant women were modestly better followed up at CHAM health facilities with SLAs, holding other factors constant. Nevertheless, even after user fee exemption, the average number of ANC visits was lower than the four visits recommended in the FANC approach. This could partially be attributed to what has been referred to as confidence selection where women who have had previous uneventful pregnancies consider themselves to be at low risk of complications and make fewer visits despite removal of the financial barrier.
To bring Kenya’s maternal health care services up to international standards, the country will need to re-evaluate the efficacy of its practices and policies on a regular basis. Further research on the free maternal policy’s effect on care and maternal and neonatal outcomes in Kenya’s maternity hospitals is an essential part of the information-gathering required to improve health care practices and policies.
Acknowledgement
I acknowledge Mt. Kenya university, for granting me an opportunity to pursue masters in development studies course. My gratitude goes to my supervisor Dr Peter Mungai for his dedication in providing support throughout the research process. Above all, I acknowledge my heavenly father for the gift of life.
Author Declaration
Bottom of Form We wish to draw the attention of the editor to the following facts, which may be considered as potential conflicts of interest and to significant financial contributions to this work: The nature of potential conflict of interest is described below.
Conflict of Interest
No conflict of interest exists.
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Funding
No funding was received for this work.
Research Ethics
We further confirm that any aspect of the work covered in this manuscript that has involved human patients has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
We understand that this author is the sole contact for the editorial process (including EVISE and direct communications with the office). He/she is responsible for communicating with the other authors, including the corresponding author, about progress, submissions of revisions and final approval of proofs.
References
- Bandura A. Self‐efficacy. Corsini Encyclopedia Psychol. 2010:1-3.
- Boudreaux C, Chanthala P, Lindelow M. Assessing the elimination of user fees for delivery services in Laos. PloS One. 2014;9(3):e89784.
[Crossref] [Google Scholar] [PubMed]
- French HM, Leeman KT, Wambach JA, Malik SK, Reber KM. Essentials of neonatal-perinatal medicine fellowship: An overview. J Perinatol. 2022;42(2):269-276.
[Crossref] [Google Scholar] [PubMed]
- El-Khoury F, Sutter-Dallay AL, Panico L, Charles MA, Azria E, van der Waerden J. Women's mental health in the perinatal period according to migrant status: The French representative ELFE birth cohort. Eur J Public Health. 2018;28(3):458-463.
[Crossref] [Google Scholar] [PubMed]
- Dzakpasu S, Soremekun S, Manu A, Ten Asbroek G, Tawiah C, Hurt L, et al. Impact of free delivery care on health facility delivery and insurance coverage in Ghana's Brong Ahafo region. PloS One. 2012;7(11):e49430.
[Crossref] [Google Scholar] [PubMed]
- Ridde V, Morestin F. A scoping review of the literature on the abolition of user fees in health care services in Africa. Health Policy Plan. 2011;26(1):1-1.
[Crossref] [Google Scholar] [PubMed]
- Witter S, Adjei S. Start-stop funding, its causes and consequences: A case study of the delivery exemptions policy in Ghana. Int J Health Plan Manag. 2007;22(2):133-143.
[Crossref] [Google Scholar] [PubMed]
- Edmond K, Zaidi A. New approaches to preventing, diagnosing and treating neonatal sepsis. PLoS Med. 2010;7(3).
- McKinnon B, Harper S, Kaufman JS. Who benefits from removing user fees for facility-based delivery services? Evidence on socioeconomic differences from Ghana, Senegal and Sierra Leone. Soc Sci Med. 2015;135:117-123.
[Crossref] [Google Scholar] [PubMed]
- Penfold S, Harrison E, Bell J, Fitzmaurice A. Evaluation of the delivery fee exemption policy in ghana: Population estimates of changes in delivery service utilization in two regions. Ghana Med J. 2007;41(3):100-109.
[Google Scholar] [PubMed]
- Feder HH. Hormones and sexual behavior. Annu Rev Psychol. 1984;35:165-200.
[Crossref] [Google Scholar] [PubMed]
- Vogel JP, Chawanpaiboon S, Watananirun K, Lumbiganon P, Petzold M, Moller AB, et al. Global, regional and national levels and trends of preterm birth rates for 1990 to 2014: Protocol for development of world health organization estimates. Reprod Health. 2016;13(1):76.
[Crossref] [Google Scholar] [PubMed]
Citation: Mungai GP, Muraguri N (2024) Efficacy of Delivery Fees Exemption Policy on Utilization of Maternity Services at Nakuru County Referral Hospital. Clinics Mother Child Health. 21:495.
Copyright: © 2024 Mungai GP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : No funding was received for this work.

