Indexed In
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Access to Global Online Research in Agriculture (AGORA)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- SWB online catalog
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2024) Volume 15, Issue 4
Effect of Behaviour Change Communication to Prevent Iron Deficiency Anemia and Hemoglobin Concentration among Children Growth Age 6-59 Months in Central Highland of Ethiopia: Cluster Randomized Control Trial
Abebe Ferede1*, Tefera Belachew2 and Muluemebet Abera32Department of Nutrition and Dietetics, Jimma University, Jimma, Ethiopia
3Department of Population and Family Health, Jimma University, Jimma, Ethiopia
Received: 14-Apr-2020, Manuscript No. JFPT-24-3875; Editor assigned: 17-Apr-2020, Pre QC No. JFPT-24-3875 (PQ); Reviewed: 01-May-2020, QC No. JFPT-24-3875; Revised: 15-Jul-2024, Manuscript No. JFPT-24-3875 (R); Published: 12-Aug-2024, DOI: 10.35248/2157-7110.24.15.1117
Abstract
Objective: Although the prevalence of anemia increased according to the recent demographic and health survey report, dietary Behavioral Change Communication (BCC) in the community especially in Ethiopia where not introduced rather than iron supplementation trial among individual children. BCC is important to modify community’s behaviour on intake of iron rich dietary intake of children. This study aimed to assets effect of BCC on haemoglobin concentration among children growth age 6 to 59 months.
Materials and methods: A Clustered Randomized Control Trial (CRCT) was carried out among children age 6-59 months and their index mothers, care givers in Arsi zone, central highlands of Ethiopia from February 2017 to April 2019. “Kebeles” (small administration units) were taken as clusters and randomly assigned to either the intervention or control arm. There was a sufficient buffer zone between the intervention and control clusters to avoid information contamination. mothers (care) givers and their index children were selected from both intervention and control clusters using simple random sampling technique at baseline. Data on the background characteristics and Hemoglobin concentration (Hbc) were collected from children age 6-59 months. Behaviour change communication was given on the intervention clusters for 15 months using explanatory poster and demonstration method. At the end line blood sample was taken from the same children and Hbc was determined using HemoCue Hb 301 analyzer. Descriptive statistics and a Generalized Estimating Equations (GEE) models were fitted to isolate independent predictors haemoglobin concentratuion.
Results: The mean (± sd) Hbc level was 143 g/L ± 1.6 g/L and 148.34 g/L ± 14.91 g/L for the intervention and control groups had 130.73 g/L ± 14.92 g/L. The difference of differences in the mean haemoglobin level was 7.69 for the intervention and 3.81 for the control (P=0.001). On generalized estimating equations analyses model after adjusting for the background variables the intervention group had increased Hbc by 9.93 mg/dl (β=9.93, P<0.05). Similarly, height for age Z-score was positively associated with Hbc mean level (β=7.151, P<0.05). The othyer variables positively associated with Hbc were: Consumption of organ meats in week (β=5.352, P<0.05) and not using cow milk as complementary food exclusively (β=8.110, P<0.05) and introduction of complementary food at age of 6th of children (β=4.031, P<0.05).
Conclusion: The study demonstrated positive effect of behaviour change communication on haemoglobin concentration of children implying the need for the galvanizing efforts to disseminate nutrition behaviour change communications to mothers and care givers of the underfive years old children to curb the increasing concern of anemia among these target group.
Keywords
Haemoglobin concentration children growth; Dietary intake; Behavioral change; Highland; Ethiopia
Abbreviations
Hbc: Hemoglobin concentration; g: Gram; L: Litter; g/L: Gram per litter of blood; n: Sample; Z: Z score; SD: Standard Deviation, Β: Beta; CI: Confidence Interval
Introduction
Particularly, Iron Deficiency (ID) in children is specifically associated with impaired mental and physical development. In advance of its effect, cognitive disturbances can be developed without sign of anemia. During infantile period of children age 2 to 6 months has a high risk of iron deficiency due to their rapid growth. Many of report agreed over untreated iron deficiency can affect a child's growth and development.
According to WHO report, iron deficiency globally estimated to over 2 billion people are anemic and in each year, around 0.8 million deaths (1.5% of the total) attributed to iron deficiency. In terms of the loss of healthy life, expressed in Disability- Adjusted Life Years (DALYs), iron-deficiency anemia results in 25 million DALYs lost (or 2.4% of the worldwide). Specifically in the African region, about 244 million (46%) of people were estimated to anemic [1].
Before twenty years ago, in developing countries 45% children aged less than 5 years affected with ID anemia. According to WHO global database sources, currently the prevalence of IDA in children 6 to 59 months excesses to 46% in selected countries of east and southern Africa. From Africa countries, Uganda leading by 72.6% and followed by Malawi was 62.5%. However, a trend analysis for anemia indicate that in East Africa the trend of anemia among children aged 6-59 months reducing from 74% (65-81) in 1995 to 55% (50-59) in 2011. From various current finding, the prevalence of anemia in developed countries became lower to 7% and among European children due to enhancing enriched foods, the use of supplements and change with dietary intake has become effective to significant drop to 2%-6% IDA among children.
In Ethiopia, the prevalence of anemia within children age 6 to 59 months has being increasing from time to time. At this age group, the trend of anemia was 54 percent in 2005, 44% in 2011 and 56% in 2016. There was little studies have been conducted via the country and mostly relayed to iron supplementation trials to prevent IDA. However, these studs were not linked to increasing Haemoglobin concentration (Hbc) through dietary behavioral change. To change young children dietary intake, mothers or caregivers have to get knowledge and attitude related to food sources and their preparation, means of self monitoring in gastrointestinal absorption enhancing and inhibiting dietary behaviors [2].
This BCC interventional study had initially taken a baseline assessment that addressed the past behavior of mothers/ caregivers in young children feeding, determined Hbc level and nutritional status of the children for base of BCC intervention.
The endline survey was focused to determine the effect of current BCC intervention project that compressed mothers/ caregivers had modified their behavor and the meeting point of self-monitoring was extant to increasing their children Hbc and growth comparative to clustered control group.
Materials and Methods
Study area and period
The study was conducted from February 2018 to April 2019 (for 15 months) in central highland of Ethiopia which includes area found near to arsi bale plateau and the neighbouring of Chilalo mountain. This includes, Tiyo, Limuna Bilalo, Digeluna Tijo districts and Asella town.
Community based Cluster Randomized Control Trial (CRCT) was used answer the study hypothesis. Sixteen kebeles were selected from highland districts of Arsi zone and randomly assigned either to intervention group or control group.
All children age 6-59 months and their pair mothers/caregivers found in districts central highland of Ethiopia were considered as the source population while children age 6 to 59 months old and their pair mothers/caregivers selected for this study form selected districts found in central highland of Ethiopia were considered as study population.
A total sample size of 1012 mother child pair (506 intervention and 506 control was determined using G power 3.0 software with assuming a power of 95%, precision of 5%, effect size of 0.227 and intervention to control ratio of one [3].
Multistage sampling method was applied to allocate intervention and control clusters randomly. First, sixteen kebeles were randomly assigned to either intervention or control cluster using Emergency Nutritional Assessment (ENA) software and eight kebeles were allocated to intervention; while the remainder eight were allocated to control. Finally, Individual Households (HH) and correspondent mothers/caregivers with their index children 6-59 months were selected using systematic random sampling technique.
During the first months of survey, assessment of women’s Knowledge and Attitude (KA) about prevention of IDA and dietary intake of children were assessed. Different recommended dietary sources intake and complementary foods modes used by children were assessed. During the baseline survey, Hbc was measured to determine the past experiences could sufficiently provided children with enough essential iron nutrients.
Mothers/caregivers were oriented about the need of requisition blood specimen collection from their children before taking specimen each child’s hand was warmed and relaxed, consequently, after mother/guardian agreed, she was asked to firm comfortable hold of her child to prevent minimum accidental injury.
A total of 1012 children blood samples were collected and analyzed for HBC at baseline. In the course of intervention, a total of 815 children and their pair mothers/caregivers were completed the dietary BCC intervention. At end line survey, 506 (100%) blood samples from intervention group and 309 (61.07) children from control groups were collected.
Trained laboratory technologists were collected each child’s blood samples and analyzed for determining hemoglobin concentration (Hbc using hemocue Hb 301 analyzer [4].
The communication activities among Health Extension Workers (HEW) played an important role. The BCC was given for 15 month with every 2 weeks frequency for each kebels by correspondent trained HEW and supervised during intervention event conducted and feedback was given for each HEW after her/his completion of each intervention event.
Women in the intervention clusters were provided with selfmonitoring, behavioral contracts and goal setting form February 2018 to April 2019 for sustainable and modifiable diversified dietary intake of children. These activities were accomplished mainly by HEW through regular time (every two weeks) interval. About maintaining plant and animal food sources when availability or affordability limited in community, complementary foods preparation for the small child which have sufficient nutrient content and density with micronutrient content and increasing the bioavailability of iron that may be affected by absorption inhibitors in the diet and challenges of plant-source based meals had been focused in the intervention programme. Most of the intervention time women were invited to ask about the massages that were needed revision or clarification any of knowledge or behavioural barriers at their homes related to iron nutrient intake [5].
Measurements
Blood test for Hemoglobin (Hbc): Before blood samples was collected, mothers/guardians had been informed about required blood sample and each child’s hand was warmed and relaxed for safe and precise finger prick at child’s finger to prevent minimum risk. Consequently, after mother/guardian agreed, she was asked to comfortably hold of her child to prevent sudden movement and accidental injury. Trained laboratory technologists collected each child’s blood samples for both periods of baseline and endpoint survey. Hemoglobin concentration (Hbc) was determined using hemocue Hb 301 analyzer. Each analyzed Hbv were adjusted for altitude.
Anthropometric measurements: Height was measured with bare feet to the nearest 1 cm using a stadiometer (a vertical tape fixed perpendicular to the ground on the wall) used for children age 24 months. Length board was used for children age less than 24 months. During measurement, the individual child relaxed with no shoes on and lied parallel to the long axis of the board and then measurement had been taken using 2 trained data collectors. Each child’s height was taken and calculated against his/her age for more anthropometric indices suchas Height for Age Z score (HAZ) index to determined children’s growth.
Weight measured in Kilogramme (Kg) without shoes and with slight cover dress, using a battery-powered digital scale for children whom were able to stand and hanging spring scale for children<2 years to the nearest of 100 gm to 200 gm. The weight scale was calibrated to zero before taking the next measurement. Additionally, each child’s weight taken was calculated against height for better anthropometric understanding using Weight for Height Z score (WHZ) indices to measure thinness. These anthropometric indices were absolutely taken and interpreted based on WHO reference [6].
Data processing and analysis: At the first step of data entering, children’s’ Height (Ht), Weight (Wt), age and sex were entered using Emergency Nutrition Assessment (ENA) software to determine children nutritional status. These variables transformed into HAZ and WHZ for each individual study subject. HAZ ≥ -2 Z-score Standard Deviation (ZSD) predicts as normal growth status and HFA ≤ -2 ZSD evidenced that child’s growth was stunted. In addition to this, WHZ analysed for each child to determine credence of body mass in relation to his/her height and WHZ ≥ -2 ZSD specify as normal and WHZ ≤ -2 ZSD had been considered as individual had thinness (wasting).
Differences between baseline and endpoint Hbc were compute. The association between Hbc and different background characteristics of the study participants was done both for the control and intervention groups for the baseline and endline survey. The differences of difference between intervention and control groups and other variables significance against Hbc declared at T-test pv<05. Variables that had P>0.2 were taken for further analyses with generalized estimating equations. The results were presented using with Beta coefficients (β) and 95% confidence intervals (Figure 1).
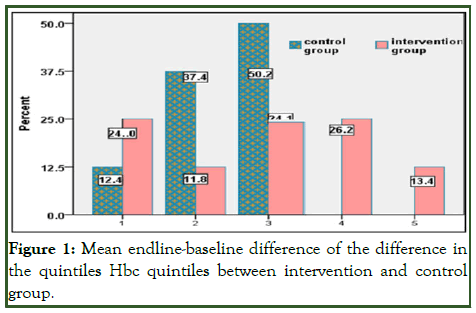
Figure 1: Mean endline-baseline difference of the difference in the quintiles Hbc quintiles between intervention and control group.
Results
From 1012 children and their mothers/caregivers who were participated at baseline survey, only 80% completed their period of intervention and participated at end line survey. Most (61.82%) of mothers/caregivers were found pm the reproductive age (20 to 35 years) and over half (54.72%) were from households that had 1000-5,000 annual income (Table 1) [7].
| Variables | Frequency (n=812) | Percent (%) |
|---|---|---|
| Maternal age | ||
| Age<20 | 119 | 14.6 |
| Age 20-35 | 503 | 61.72 |
| Age>35 | 193 | 23.68 |
| Education levels | ||
| Illiterate | 186 | 22.82 |
| Grade 1-4 | 166 | 20.44 |
| Grade 5-8 | 273 | 33.62 |
| Grade 9-12 | 190 | 23.4 |
| Marital status | ||
| Single | 36 | 4.42 |
| Married | 711 | 87.24 |
| Divorced | 47 | 5.77 |
| Widowed | 21 | 2.57 |
| Occupation | ||
| House wife | 466 | 57.17 |
| Farmer | 244 | 29.94 |
| Business women | 56 | 6.87 |
| Gov/NGO employee | 7 | 0.86 |
| Daily labourer | 42 | 5.16 |
| Annul income (Birr) | ||
| <1000 | 250 | 30.68 |
| 1000-5,000 | 446 | 54.72 |
| 5001-10,000 | 90 | 11.04 |
| >10,000 | 29 | 3.56 |
| Total | 815 | 1 |
Table 1: Mothers’/caregivers’ and paired children socio-demographic status of in central highland of Ethiopia, 2019.
All (100%) intervention group completed their dietary BCC intervention and participated at endline survey. But due to different grounds, only 61.07% of the controls participated in the endline survey.
At baseline, children age<24 months were 50.2% but, at end line survey, majority of children (70.92%) were age ≥ 24 months and children age<24 months was become 29.08% because of their age increased by 15 months, which was spent for this intervention.
Regarding their sex, 51.2% male and 48.8% female were enrolled in the study (Table 2).
| Variables | Baseline assessment, n=1012 groups | Endline assessment, n=815 groups | ||||
|---|---|---|---|---|---|---|
| Intervention (n=506 (%)) | Control (n=506 (%)) | % | Intervention (n=506 (%)) | Control (n=309 (%)) | % | |
| Age | ||||||
| >24 months | 254 (50.20) | 250 (49.41) | 49.8 | 442 (87.35) | 136 (44.01) | 70.92 |
| <24 months | 252 (49.80) | 256 (50.59) | 50.2 | 64 (12.65) | 173 (55.99) | 29.08 |
| Sex | ||||||
| Male | 263 (51.98) | 276 (54.55) | 53.26 | 259 (51.19) | 157 (50.81) | 51.04 |
| Female | 243 (48.02) | 230 (45.45) | 46.74 | 247 (49.81) | 152 (49.19) | 48.96 |
| Hbc | ||||||
| >110 g/L | 375 (74.11) | 453 (89.53) | 81.8 | 464 (91.7) | 279 (90.29) | 91.17 |
| <110 g/L | 131 (25.89) | 53 (10.47 | 18.2 | 42 (8.3) | 30 (9.71) | 8.83 |
Table 2: Prevalence of IDA among intervention and control groups during baseline and endline surveys, among children age 6 to 59 months, in central highland of Ethiopia, 2019.
Mean Hbc was increased (143 g/L ± 1.6 g/L) at endpoint than the baseline (125.5 g/L ± 1.73 g/L. Mean Hbc among intervention group was 122.55 (± 17.98) g/L at baseline and 148.34 (± 14.91) g/L at endline survey. However, no mean change among control group 130.71 (± 15.67) at baseline and 130.73 (± 14.92) g/L at endline.
The prevalence among children who participated in this study at baseline was (18.2% and thus, the baseline finding was higher compared to endpoint survey (8.83%), which was almost by more than the half of percent of IDA decreased among study subjects. At baseline survey, the prevalence of iron deficiency anemia (Hbc<110 g/L) among intervention group was higher (25.89%) than control group (10.47%). However, the prevalence of IDA among control group at endpoint survey almost had not change (9.71%) from the baseline finding. But, IDA among intervention group declined by more than three times (8.30%) at endline survey than the baseline [8].
In our rank analysis to compare the mean of endline-baseline difference of the difference in the quintiles of Hbc between intervention and control groups showed that near to 50% control group subjects found at lower ranks (1st and 2nd). However, significant proportion (40.1%) of in intervention group subjects found at higher rank (4th and 5th). But, nothing observed from the control group at 5th rank. In advance analysis, the proportion of study subjects assigned to control group had not found at higher ranks (4th and 5th). For more interpretation perceive Figure 1.
Additionally, at endline survey, 24.5% of intervention group had found at higher (5th) rank compared to control group that was 13, 1%. In analysis spectrum, the distribution of study subjects among intervention group was regular and increased while rank increased. The experience of control group along the rank appreciated as higher proportion of study subjects found at lower ranks (24.1%) and less proportion of subjects found at higher ranks (Figure 2).

Figure 2: Endline differences in HbC among children assigned to intervention and control group.
The difference of differences in the mean haemoglobin level was 7.69 for the intervention and 3.81 for the control. Mean Hbc during baseline and endline surveys had differences between intervention and control groups (MD Hbc=3.88, SE=1.02) g/L, p=0.001). The differences within baseline and end line showed that children who had stunted growth (< -2 Z SD) were more likely to be iron deficient (mean Hbc=3.76) g/L compared to those children who were normal (HFA ≥ -2 Z SD) mean Hbc=7.15) g/L consequential the mean Hbc difference was significant (MD=3.39, SE=1.21, p=0.001). Also children who had WAZ ≥ -2 Z SD had higher mean Hbc difference 6.92 g/L compared to children who had WAZ ≤ -2SD 2.07 g/L and differences mean Hbc among this nutritional status at baseline and endline survey statistically significant (MD=4.85, SE=1.89, p=0.001) g/L (Table 3).
| Variables | Haemoglobin concentration | ||||
|---|---|---|---|---|---|
| n (%) | Mean | Mean diff | SE | PV | |
| Groups | |||||
| Intervention | 506 (62.09) | 7.69 | |||
| Control | 309 (37.91 | 3.81 | 3.88 | 1.02 | 0.001* |
| Age | |||||
| ≥ 24 months | 578 (70.9) | 6.56 | |||
| <24 months | 237 (29.08) | 3.96 | 2.6 | 1.36 | 0.058* |
| Sex | |||||
| Male | 416 (51.04) | 6.68 | |||
| Female | 399 (48.96) | 5.92 | 0.76 | 0.81 | 0.348 |
| HAZ | |||||
| ≥ -2SD | 610 (74.85) | 7.15 | |||
| < -2SD | 205 (25.15) | 3.76 | 3.39 | 1.21 | 0.001* |
| WHZ | |||||
| ≥ -2SD | 653 (80.12) | 6.29 | |||
| < -2SD | 162 (19.88) | 6.37 | -0.08 | 1.02 | 0.936 |
| WAZ | |||||
| ≥ -2SD | 710 (87.12) | 6.92 | |||
| < -2SD | 105 (12.88) | 2.07 | 4.85 | 1.89 | 0.001* |
Note: Hbc, hemoglobin concentration; g, gram; L, Litter; g/L, gram per litter of blood; n, sample; HAZ, height for age SD; WHZ, weight for height SD; WAZ, weight for age SD; SD, Standard Deviation; Z, Z score
Table 3: Mean Hbc differences between baseline and endpoint survey within different variables among children age 6 to 59 months in central highland of Ethiopia.
Concerning children’s mothers’/caregivers’ knowledge and attitude status towards IDA prevention and self mentoring in dietary intake behavior was improved from baseline 49.9% to 74.72% end line. There was a difference in the attitude in IDA prevention between intervention group (80.04%) and control group (66.02%).
The mean Hbc differences endline-baseline was higher (139.87) g/L among children whose their mothers/caregivers who modified their commune attitude towards IDA prevention during intervention period than the control group (118.43) g/L and resulting in mean Hbc difference was significant (MD=21.44 SE=2.07, p=0.014).
Furthermore, understanding the way of preventing IDA among intervention group of mothers/care givers was increased to their children mean Hbc difference (135.45) g/L compared to the control group (124.27) g/L and this mean Hbc difference became substantial (MD=11.18, SE=1.34, p=0.016). Mothers/ caregivers who used basic diet from own production among intervention group had increased mean Hbc difference of their children (MD=29.0, SE=3.12, p=0.010) and behaviour experiencing with usual fruit consumption after meal among household during intervention period had increased mean Hbc of children (MD=30.75, SE=5.17, p=0.001) (Table 4).
| Variables | n=815 | Mean HbC (± sd) | Hbc mean differences (± sd) | SE | Pv | |
|---|---|---|---|---|---|---|
| Yes (%) | No (%) | |||||
| Commune attitude in iron deficiency | ||||||
| Intervention | 405 (80.04) | 101 (19.96) | 139.87 (± 11.03) | 4.36 (± 0.76) | 2.07 | (0.014)* |
| Control | 204 (66.02) | 105 (33.98) | 118.43 (± 14.33) | |||
| Awareness (knowing) of IDA | ||||||
| Intervention | 418 (82.61) | 88 (17.39) | 127.91 (± 10.12) | 3.93 (± 0.92) | 0.93 | 0.083 |
| Control | 179 (57.93) | 130 (42.07) | 123.98 (± 11.60) | |||
| Understand the cause of IDA | ||||||
| Intervention | 421 (83.20) | 85 (16.80) | 135.45 (± 11.81) | 11.18 (± 1.18) | 1.34 | 0.016* |
| Control | 165 (53.40) | 144 (46.60) | 124.27 (± 13.32) | |||
| Basic diet from own production | ||||||
| Intervention | 402 (79.45) | 104 (20.55) | 141.32 (± 12.13) | 29.00 (± 1.07) | 3.12 | 0.010* |
| Control | 126 (40.78) | 183 (59.22) | 112.32 (± 14.23) | |||
| Fruit intake after meal | ||||||
| Intervention | 413 (78.98) | 101 (21.03) | 148.13 (± 11.17) | 30.75 (± 3.21) | 5.31 | 0.001* |
| Control | 135 (46.71) | 154 (53.29) | 117.38 (± 14.45) | |||
| Use only cow milk as complementary fed | ||||||
| Intervention | 423 (83.60) | 83 (16.40) | 137.61 (± 13.21) | -5.61 (± 0.72) | 0.23 | 0.131 |
| Control | 144 (46.60) | 165 (53.40) | 143.22 (± 15.35) | |||
| Using tea/coffee with meal | ||||||
| Intervention | 432 (82.60) | 91 (31.49) | 124.27 (± 12.71) | 11.85 (± 2.17) | 0.65 | 0.163 |
| Control | 138 (47.75) | 151 (52.25 | 135.45 (± 16.32) | |||
Table 4: Endline mothers’/caregivers’ knowledge and attitude status about IDA prevention and children dietary intake in central highland of Ethiopia, 2019.
Finally, on Generalized Estimating Equations (GEE) model, mean Hbc difference increased by 9.93 mg/dl among intervention group (β=9.93, 95%, CI: 3.60-13.74), whereas, children growth (HAZ ≥ -2SD ) had positive association with Hbc (β=7.151,95% CI: 192-7.38).
Regarding dietary intake pattern, meal contained organ meats had a likely to increase Hbc mean (β=5.35, 95% CI: 1.04-8.65) and having diversified animal and plant source for complementary food increased mean Hbc (β=8.11, 95% CI: 1.26-15.96).
Discussion
After 15 months of behaviour chgnage communication intervention, the mean haemoglobin concentration among study subjects was higher and changed from 125.5 g/L at baseline to 143 g/L at endpoint survey compared to global mean haemoglobin trained change between 1995 and 2011 among children age under 5 years showed that minor improvement was reported (from 109 g/L to 111 g/L), but among high income countries was better (130.0 g/L) which is lesser than our current study findings [9].
The prevalence of anemia was very lower (8.74%) at the endline survey, especial among intervention group (7.65%) than global finding at different levels. According to WHO 2015 report, the prevalence of anaemia among children age 6 to 59 months in 2011 was 42.6% which is higher than our study finding. The national Demographic Health Surveys (EDHS) reported the prevalence pof anemia to be 56% and 44% in 2016 and 2011 in that order. Study conducted in Kilte Awulaelo districts of northern Ethiopia showed that the prevalence of anemia among children was 37.3% which is far higher than our findings. These differences could be due to the fact that our study area is high altitude, where malaria is very less and there will be physiological polycythemia. Furthermore, as the current study has an intervention, it is expected that the prevalence of anemia will be lower in the overall sample.
However, the prevalence of anemia in our current finding suggests that the problem can be considered as mild public health problem and comparable to that of developed and rapidly developing countries (6%-20%). This is good although a lot of work remains to be improved tin encouraging mothers or caregivers about infant and young child feeding to prevent anemia throughout the nation [10].
It was also observed that mean Hbc was significantly associated with height for age z-score, which is consistent a study conducted in Kazakhstan. A systematic review and meta-analysis study concluded that there no significant association between haemoglobin concentration and children growth. This might be due to the fact that the study analyzed multiple observational and short interventional studies that might not be sufficient to elucidate the effect of haemoglobin concentration on children growth. A positive association between haemoglobin and complementary foods that contain iron rich sources foods has also been reported. According to World Health Organization (WHO), children under 5 years are at risk of iron deficiency anemia due to not consuming animal source of foods (liver, meat and fish) which are rich in iron. Similar to the reports of WHO our findings showed that most of the mothers/caregivers did not feed iron rich with foods to their young children which could increase the risk of anemia.
It was also observed that households who regularly provided cow’s milk to their young children as exclusive complementary food had lower mean Hbc. Milk contains low iron (about 0.2 mg/l to 0.5 mg/l) which might not meet the requirement for young children. Especially, frequent milk consumption without alternative complementary food could lead to lower intake of iron. The introduction of cow milk with the long duration of feeding at early age of children became the most important dietary risk factor for anemia. Milk contained micronutrients (casein, whey proteins and calcium) that potentially inhibit the absorption of minute iron found in cow’s milk [11].
Our BCC intervention targeted individual mother/caregiver to promote better processing of household foods into the possible nutritious complementary foods for their children. In poor resource setting iron supplementation trials required meticulous for study subjects who are living or coming to areas where malaria and infectious diseases are common. Distinction to this, dietary BCC interventional study would not required these type of precondition to prevent IDA. Progressively more food-based approaches involving fortification, improving dietary quality through diversification/modification and nutrition education and biofortification are being pursued than iron supplementation. In Ethiopia, although essential nutrition actions behaviour change communication has been going on using urban and rural health extension workers to reduce micronutrient deficiency, the prevalence of anaemia rather increased. The findings imply the need for upgrading the level of education being given to mothers/care givers to prevent anaemia through dietary approaches. The study did not assess the prevalence of anemia through all citizens which should be considered by future researches [12].
Conclusion
The findings showed that the mean haemoglobin concentration increased from 122.55 g/L ± 17.98 g/L to 148.34 (± 14.91) g/L for the intervention group compared with to that of controls which increased from 130.71 ± 15.67 to 130.73 ± 14.92) g/L. The study demonstrated a positive effect of behaviour change communication on haemoglobin concentration of children implying the need for the galvanizing efforts to disseminate nutrition behaviour change communications to mothers and care givers of the under five years old children to curb the increasing concern of anemia among these target group. Dietary BCC intervention is better to use at everywhere and at any time contrasts to iron supplement trial.
Acknowledgement
We would like to express their gratitude to Arsi university for financial support and ethical approval. We extend our special gratitude to central highland provinces (Arsi and Bale), Munesa, Asella, Limuna Bilalo, Digeluna Tijo, Honkolo Wabe health offices for their administrative, technical and material support. Finally, we thank the study participants and health extension workers for their involvement in the study.
Ethical Approval
This research was approved by ethical review committee of Arsi university. Letter of permission was obtained from Arsi zone administrative and health department offices. At the end, we obtained permission from 8 district administrative offices 16 kebeles (smallest administrative units) which were site for data collection administrations offices. In addition, all of the study participants (children’s mothers/caregivers) were informed about the purpose of the study.
Each child’s mother or caregiver was informed about required blood sample from her child to be analyzed hemoglobin level. Consequently, mother/guardian were asked to have a firm comfortable hold of the child, and immobilize the finger to be punctured, to prevent sudden movement and accidental injury. All percussions were taken to prevent minimum risk and made safe during each child’s finger prick.
The respondents were notified that they have the right to refuse or terminate at any point of our request of survey. The information provided by each respondent was kept confidential.
Funding
The research was fully funded by Jimma university.
Conflict of Interest
None declared.
Author Contribution
A. Ferede: The conception of the design of the research project, data collection, data entry, analysis, preparation and write up manuscript and appraisal. Belachew T. and Muluemebet A. participated in the analysis of data, write up and preparation of manuscript for publication. All authors read and approved the final manuscript I read and approved the final manuscript for publication.
References
- Black MM. Micronutrient deficiencies and cognitive functioning. J Nutr. 2003;133(11):3927S-3931S.
[Crossref] [Google Scholar] [PubMed]
- Ryan AS. Iron‐deficiency anemia in infant development: Implications for growth, cognitive development, resistance to infection and iron supplementation. Am J Phys Anthropol. 1997;104(S25):25-62.
- Grantham-McGregor SM, Ani CC. The role of micronutrients in psychomotor and cognitive development. Br Med Bull. 1999;55(3):511-527.
[Crossref] [Google Scholar] [PubMed]
- Chin B. Income, health and well-being in rural Malawi. Demog Res. 2010;23(35):997-1030.
[Crossref] [Google Scholar] [PubMed]
- Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995-2011: A systematic analysis of population-representative data. Lancet Glob Health. 2013;1(1):e16-25.
[Crossref] [Google Scholar] [PubMed]
- Fentaw W, Belachew T, Andargie A. Anemia and associated factors among 6 to 59 months age children attending health facilities in Kombolcha town, northeast Ethiopia: A facility-based cross-sectional study. BMC Pediatr. 2023;23(1):209.
[Crossref] [Google Scholar] [PubMed]
- McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B. Worldwide prevalence of anaemia, WHO vitamin and mineral nutrition information system, 1993-2005. Public Health Nutr. 2009;12(4):444-454.
[Crossref] [Google Scholar] [PubMed]
- World Health Organization. Physical status: The use and interpretation of anthropometry. WHO Tech Rep. 1995;854:1-452.
- Gebreegziabiher G, Etana B, Niggusie D. Determinants of anemia among children aged 6-59 months living in Kilte Awulaelo Woreda, northern Ethiopia. Anemia. 2014;2014:245870.
[Crossref] [Google Scholar] [PubMed]
- Ferede A, Belachew T, Abera M. Effect of behaviour change communication to prevent anemia and haemoglobin concentration among children growth age 6-59 months in central highland of Ethiopia: Cluster randomized control trial. Biomed J Sci Tech Res. 2020;31(5):24595-24603.
- Larson LM, Kubes JN, Khishen S, Shankar AH, Prado EL. Effects of increased hemoglobin on child growth, development and disease: A systematic review and meta-analysis. Ann N Y Acad Sci. 2019;1450(1):83-104.
[Crossref] [Google Scholar] [PubMed]
- Male C, Persson LA, Freeman V, Guerra A, Haschke F. Prevalence of iron deficiency in 12-mo-old infants from 11 European areas and influence of dietary factors on iron status (Euro-growth study). Acta Paediatr. 2001;90(5):492-498.
[Crossref] [Google Scholar] [PubMed]
Citation: Ferede A, Belachew T, Abera M (2024) Effect of Behaviour Change Communication to Prevent Iron Deficiency Anemia and Hemoglobin Concentration among Children Growth Age 6-59 Months in Central Highland of Ethiopia: Cluster Randomized Control Trial. J Food Process Technol. 15:1117.
Copyright: © 2024 Ferede A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.