Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 0, Issue 0
Dysnatremia in COVID-19 Disease, Characteristics of Patients, Clinical Manifestation and Outcome in Pakistan
Faiza Saeed1*, Ashar Alam1, Shoukat Memon1, Javeria Chughtai1, Shahzad Ahmed1, Sobia Tariq1, Beena Salman2 and Salman Imtiaz32Department of Micro Biology, The Indus Hospital, Korangi Crossing Karachi-75190, Sindh, Pakistan
3Department of Nephrology, Chairperson Indus Nephrology Network, The Indus Hospital, Korangi Crossing Karachi-75190, Sindh, Pakistan
Received: 10-Mar-2021 Published: 01-Apr-2021, DOI: 10.35248/2157-7560.21.s12.001
Abstract
Background: Imbalance of serum sodium in the form of hypo and hypernatremia has negative prognostic impact, and is linked with increase in morbidity and mortality. COVID 19 is a deadly viral infection, and can be complicated with either of the two states. This increases the complications associated with the COVID 19 infection.
Material and methods: This is an observational cohort study, conducted at The Indus Hospital Karachi, from March 2020 to September 2020. All patients were divided into three groups on the basis of their serum sodium level, and distribution of variables was observed in all these three groups. To observe the effect of dysnatremias on outcome, binary logistic regression was run and odds ratios with 95% confidence interval were obtained.
Results: We included 655 patients, in which 70.7% were male, while 29.3% were female. Mean age was 54 ± 15.5 with minimum of 1 year and maximum of 95 year. Hyponatremia was more common 154(23.5%) than hypernatremia 79(12.1%). Dysnatremia were common in patients of age group of 51-65 years (Hyponatremia 72(46.8%) hypernatremia 36(45.6%). Hyponatremia didn’t show any significant effect on the clinical manifestation, critical illness and outcome of the patients except drowsiness (p=0.022). On the other hand hypernatremia had highly significant effect on clinical manifestation, critical illness and outcome of the patients. The patients who had hypernatremia died 16.8 times more than patients with normal sodium (p=0.001).
Conclusion: Dysnatremias has profound impact on the outcome of COVID-19 patients. We found development of hypernatremia has devastating effect on patient survival.
Keywords
Dysnatremias; Hyponatremia; Hypernatremia; COVID-19; Pakistan; Electrolytes imbalanc
Introduction
Water imbalance leading to Dysnatremia is the most common electrolyte disturbance observed in clinical medicine. Two different pathways control this tightly regulated mechanism; these include osmoregulation via ADH and volume regulation via RAAS and natriuretic hormones. Water and sodium balance are regulated independently by these pathways which prevent large changes in plasma osmolality and the effective circulating volume. Severe sodium disorders are related with increased morbidity and mortality [1], even mild hyponatremia, especially when it complicates conditions, such as heart failure and sepsis [2].
Hyponatremia is much common (50%) amongst hospitalized COVID-19 patients than expected [3],and a recent study further suggested that serum sodium concentration was inversely correlated with IL-6, and association of hyponatremia led to a more severe outcome of COVID-19 disease [4]. Similarly, Hypernatremia in patients treated in medical intensive care units (ICUs) varied between 6% and 26% [5]. During the treatment of patients with severe coronavirus disease 2019 (COVID-19), there was a frequent development of treatment-resistant hypernatremia possibly due to diuretics and steroids used as a part of COVID-19 infection treatment [6].
The impact of COVID-19 is different all over the world. Pakistan has relatively low prevalence of disease as up till now 530,818 cases have been detected, while total number of closed cases, 495,755 had an out come out, of which 484,508 (98%) recovered and 11,247 (2%) died. In contrast to France with 3,011,257 cases detected, with total number of 288,469 closed case which had an outcome, 215,822 (75%) Recovered 72,647 (25%) patients died [7]. COVID-19 is a highly infective organism and is now equipped with mutational characteristics. It can lead to a potentially lethal pneumonia which can cause mortality in hospitalized patients as high as 20.3-27.9% [8,9]. The association of hyponatremia and hypernatremia with viral infection and sepsis needs to be explicated and its relation with poor prognosis in patients admitted with COVID-19 need to be unraveled.
The primary objective of this study was to find out whether dysnatremias are associated with age, comorbid conditions, mechanical ventilation, vasopressor support or death.
Till date, very sparse data is available regarding sodium disorders associated with COVID-19. We conducted this study to determine the varying degree of sodium imbalance among patients with COVID-19 and identify the outcome associated with it in our region.
Materials and Methods
This is an observational cohort study of all patients admitted in Indus Hospital COVID ICU with a confirmed diagnosis of COVID pneumonia by RT-PCR from 1st March 2020 to 30th Sep 2020. Patients who did not have complete data were excluded. Permission from the institutional ethical review committee was taken prior to conduction of the study. History, clinical examination, laboratory investigations were acquired from the Health Management Information System (HMIS) record of the patients admitted in COVID ICU of The Indus Hospital Korangi, Karachi. Data was collected on a structured preform which included variables like age, gender, comorbid conditions, clinical presentation, hemodynamic status and lab parameters. Outcome of the patients like discharge or death was noted.
Statistical analysis
The data was entered and analyzed on IBM, SPSS version 21. Cleaning and ordering of data was done prior to analysis. Mean ± STD were computed for continuous data while frequencies with percentage were obtained for categorical data. All patients were divided in three groups according to their sodium status (Eunatremia, hyponatremia and hypernatremia) and distribution of variables was observed in these three groups. Age of the patients was also categorized in three groups, and age group of 17-50 years was taken as reference category for other age groups in logistic regression. To observe the effect of hypo and hypernatremia on outcome, critical illness of the patients, drowsiness, and confusion, binary logistic regression was run and odds ratio with 95% confidence interval were obtained. Similarly, logistic regression was also run to calculate the amount of effect of different variable like age, Acute Kidney Injury (AKI), co morbid conditions and volume status on sodium. P value of ≤ 0.05 was considered significant.
Results
There were a total of 655 patients in our study out of which 463 (70.7%) were male, while 192 (29.3%) were female. Mean age was 54 ± 15.5 with minimum of 1 year and maximum of 95 year. In terms of clinical presentation, most of our patients with dysnatremias were euvolumic and asymptomatic (Figures 1A and 1B).
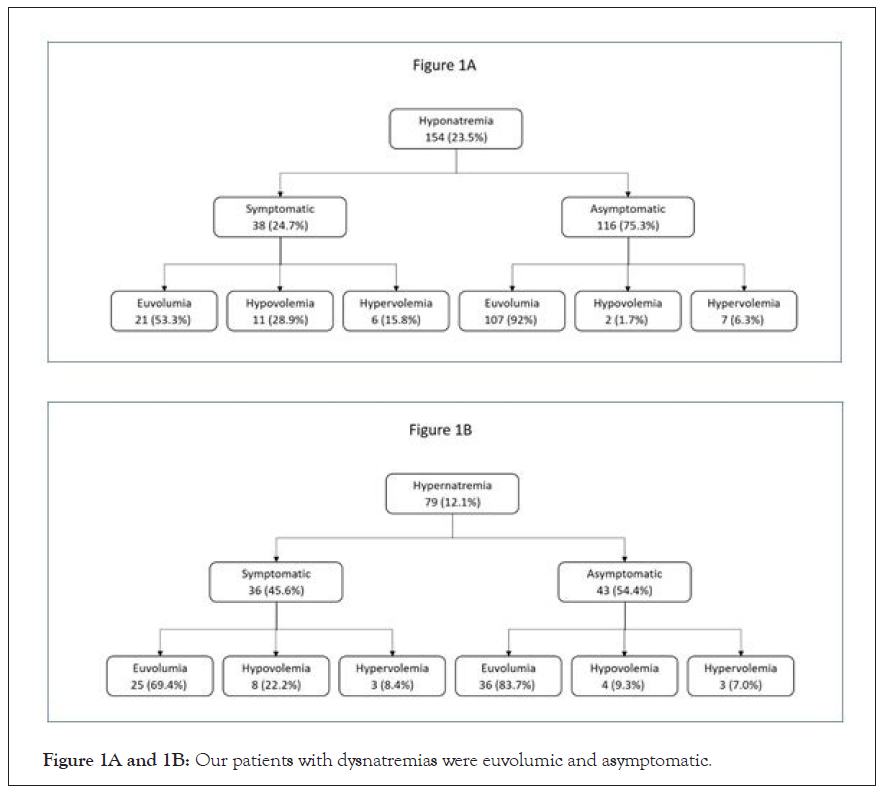
Figure 1A and 1B: Our patients with dysnatremias were euvolumic and asymptomatic.
The patients who had hypernatremia were 79 (12.1%), while hyponatremia was present in 154 (23.5%) patients, on the other hand 422 (64.4%) patients had normal range of sodium. Dysnatremia was common in patients of age group of 51-65 years (Hyponatremia 72 (46.8%) hypernatremia 36 (45.6%), as compared to other age groups. Among co morbid conditions Hypertension (HTN) was the most prevalent comorbid 380 (58%) and hypertensive patients had more hyponatremia and hypernatremia, as compared to normotensive patients. Similarly the diabetic patients also had more hypo and hypernatremia than non-diabetics. Multi organ dysfunction is a manifestation of severe COVID and in our cohort AKI was the most occurring complication, encountered by 209 (31.9%) patients and hypernatremia was widespread in this group of the patients 53 (67.1%) as compared to non AKI patients 26 (32.9%) (Table 1A).
| Variables | Eunatremic 422(64.4) | Hyponatremic 154(23.5) | Hypernatremic79(12.1) | Total 655(%) | |
|---|---|---|---|---|---|
| Age(years) | |||||
| ≤ 50 | 171(76) | 40(26) | 14(17.7) | 225(34.4) | |
| 51-65 | 175(41.5) | 72(46.8) | 36(45.6) | 283(43.2) | |
| >65 | 76(18) | 42(27.3) | 29(36.7) | 147(22.4) | |
| Gender | Male | 299(70.9) | 102(66.2) | 62(78.5) | 463(70.7) |
| Female | 123(29.1) | 52(33.8) | 17(21.5) | 192(29.3) | |
| Comorbid of patients | |||||
| HTN | Yes | 225(53.5) | 99(64.3) | 56(70.9) | 380(58) |
| No | 197(46.7) | 55(35.7) | 23(29.1) | 275(42) | |
| DM | Yes | 167(39.6) | 84(54.5) | 46(58.2) | 297(45.3) |
| No | 225(60.4) | 70(45.5) | 33(41.8) | 358(54.7) | |
| IHD | Yes | 58(13.7) | 39(25.3) | 19(24.1) | 116(17.7) |
| No | 364(86.3) | 115(74.7) | 60(75.9) | 539(82.3) | |
| Complications of COVID-19 infection | |||||
| AKI | Yes | 103(24.4) | 53(34.4) | 53(67.1) | 209(31.9) |
| No | 319(75.6) | 101(65.6) | 26(32.9) | 446(68.1) | |
| CCF | Yes | 17(4) | 8(5.2) | 5(6.3) | 30(4.6) |
| No | 405(96) | 146(94.8) | 74(93.7) | 625(95.4) | |
| TEE | Yes | 13(3.1) | 8(5.2)10(12.7) | 10(12.7) | 31(4.7) |
| No | 409(96.9) | 146(94.8) | 69(87.3) | 624(95.3) | |
Abbreviations: HTN: Hypertension; DM: Diabetes Mellitus; IHD: Ischemic Heart Disease; AKI: Acute Kidney Injury; CCF: Congestive Cardiac Failure; TEE: Thromboembolic Event
Critically ill patients who needed ventilatory and vasopressor support were 182(27.8%) and 194(29.6%) respectively, and hypernatremia was more common in these patients as compared to non-critical patients. (Ventilatory support 53 [(67.1%) vs. 26 (32.9%) and vasopressor support 57 (72.2%) vs. 22 (27.8%)]. Likewise hypernatremia was more frequent in patients who died 69 (87.3%) than patients who recovered 10 (12.7%) (Table 1B).
| Variables | Eunatremic 422(64.4) | Hyponatremic 154(23.5) | Hypernatremic 79(12.1) | Total 655 | |
|---|---|---|---|---|---|
| Volume status | Euvolumic | 382(90.5) | 128(83.1) | 61(77.2) | 571(87.2) |
| Hypovolumic | 13(3.1) | 13(8.4) | 12(15.2) | 38(5.8) | |
| Hypervolumic | 27(6.4) | 13(8.4) | 6(7.6) | 46(7) | |
| Drowsiness | Yes | 31(7.3) | 21(13.6) | 27(34.2) | 79(12.1) |
| No | 391(92.7) | 133(86.4) | 52(65.8) | 576(87.9) | |
| Confusion | Yes | 33(7.8) | 19(12.3) | 31(39.2) | 83(12.7) |
| No | 389)92.2) | 135(87.7) | 48(60.8) | 572(87.3) | |
| Vomiting | Yes | 31(7.3) | 18(11.7) | 6(7.6) | 55(8.4) |
| No | 391(92.7) | 136(88.3) | 73(92.4) | 600(91.6) | |
| Ventilatory support | Yes | 102(24.2) | 27(17.5) | 53(67.1) | 182(27.8) |
| No | 320(75.8) | 127(82.5) | 26(32.9) | 473(72.2) | |
| Vasopressor support | Yes | 106(25.1) | 31(20.1) | 57(72.2) | 194(29.6) |
| No | 316(74.9) | 123(79.9) | 22(27.8) | 461(70.4) | |
| Outcome | Died | 123(29.1) | 35(22.7) | 69(87.3) | 227(34.7) |
| Recovered | 299(70.7) | 119(77.3) | 10(12.7) | 428(65.3) | |
Table 1(B): Distribution of clinical parameters of patients according to sodium levels n(%)=655.
Effect of demographic and comorbid variables on hyponatremia
Age, Diabetes Mellitus (DM) and Ischemic Heart Disease (IHD) were risk factors for developing hyponatremia in COVID-19 patients. The patients in age group of 51-65 years suffered hyponatremia 1.6 time more than patients of age group of 17-50 years (p<0.039). Similarly, patients of age>65 years had 1.9 times more at risk for hyponatremia than 17-50 years of age group (p=0.015). The risk of hyponatremia in diabetics was 1.6 times than non-diabetics (p=0.009). Similarly the patients with IHD developed hyponatremia 1.9 times more than patients without IHD p=0.005 (Table 2).
| Variables | Hyponatremia | Hypernatremia | |||||
|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI Lower-Upper | p value | Odds Ratio | 95% CI Lower-Upper | p value | ||
| 1 | |||||||
| Age(years) | ≤ 50 | 1 | 1 | 1 | |||
| 51-65 | 1.6 | 1.0 - 2.4 | 0.039 | 2.2 | 1.2 - 4.2 | 0.017 | |
| >65 | 1.9 | 1.1 - 3.1 | 0.015 | 3.7 | 1.9 - 7.3 | <0.001 | |
| HTN | Yes | 1.4 | 0.97- 2.1 | 0.072 | 1.9 | 1.1- 3.2 | 0.015 |
| DM | Yes | 1.6 | 1.13 - 2.3 | 0.009 | 1.8 | 1.1 - 2.9 | 0.014 |
| AKI | yes | 1.2 | 0.79 - 1.7 | 0.446 | 5.5 | 3.3 - 9.1 | <0.001 |
| IHD | Yes | 1.9 | 1.2 - 2.9 | 0.005 | 1.6 | 0.9 - 2.7 | 0.118 |
| CCF | Yes | 1.2 | 0.5 -2.7 | 0.677 | 1.5 | 0.55 - 4 | 0.431 |
| TEE | Yes | 1.1 | 0.49 - 2.6 | 0.78 | 3.8 | 1.7 - 8.5 | 0.001 |
| Volume status | Euvolumia | 1 | 1 | 1 | 1 | ||
| Hypovolemia | 1.8 | 0.89 - 3.6 | 0.099 | 3.9 | 1.9 - 8.0 | <0.001 | |
| Hypervolumeia | 1.4 | 0.69 - 2.7 | 0.365 | 1.3 | 0.511 - 3.1 | 0.62 | |
Abbreviations: HTN: Hypertension; DM: Diabetes Mellitus; IHD: Ischemic Heart Disease; AKI: Acute Kidney Injury; CCF: Congestive Cardiac Failure; TEE: Thromboembolic Event
Effect of demographic and comorbid variables on hypernatremia
In parallel with hyponatremia, hypernatremia was not only affected by the older age and DM, but with HTN, AKI and Thromboembolic event (TEE) as well. The age group of 51-65 years had greater risk of hypernatremia about 2.2 times than the age group of 17- 50 years (p=0.017). Same as patients of >65 years of age had 3.7 times more hypernatremia than patients of age of 17-50 years (p<0.001). Hypertensive patients suffered with hypernatremia 1.9 times higher than normotensive (p=0.015). Similarly, DM also 1.8 times more effect on hypernatremia than non-diabetic (p=0.014). Presence of AKI in COVID patients had 5.5 times more at risk for development of hypernatremia than non AKI patients (p<0.001). Likewise,patients with TEE had 3.8 times more hypernatremia than patients without TEE (p=0.001). Patients with hypovolemic status had 3.9 times more hypernatremia than patients with euvolumia (p<0.001).
Effect of dysnatremia on clinical status and outcome of the patients
Hyponatremia didn’t show any significant effect on the clinical manifestation, critical illness and outcome of the patients except drowsiness, as patients who had hyponatremia developed drowsiness 2 times more than the eunatremic patients (p=0.022). (Eunatremia was the reference category)
On the other hand, hypernatremia had highly significant effect on clinical manifestation, critical illness and outcome of the patients. The patients who had hypernatremia died 16.8 times more than patients with normal sodium (p=0.001). Similarly, patients with hypernatremia needed vasopressors support 7.7 times more than the eunatremic patients (p<0.001). Patients with hypernatremia required 6.4 times more ventilatory support as compared to the patients with normal level of sodium (<0.001). Likewise, hypernatremic patients were also 6.6 times more drowsy than eunatremic patients (p<0.001). Confusion was also 7.6 times higher in hypernatremia than eunatremic patients p<0.001 (Table 3).
| Variables | Odds Ratio | 95% CI Lower-Upper | p value | |
|---|---|---|---|---|
| Hyponatremia | Death | 0.72 | 0.46-1 | 0.127 |
| Vasopressor need | 0.75 | 0.48-1.2 | 0.214 | |
| Ventilatory support | 0.67 | 0.42-1.1 | 0.092 | |
| Drowsiness | 2 | 1.1- 3.6 | 0.022 | |
| Confusion | 1.7 | 0.9 - 3.0 | 0.097 | |
| Hypernatremia | Death | 16.77 | 8.4-33.6 | 0.001 |
| Vasopressor need | 7.7 | 4.5-13.2 | <0.001 | |
| Ventilatory support | 6.4 | 3.8-10.8 | <0.001 | |
| Drowsiness | 6.6 | 3.6-11.8 | <0.001 | |
| Confusion | 7.6 | 4.3 - 13.5 | <0.001 | |
Table 3: Effect of Dysnatremia on disease severity in COVID-19 infection.
Discussion
This is the first study from this country, reporting the sodium disorder in COVID-19 patients admitted in COVID-19 facility at Indus Hospital Karachi.
This study showed that the higher age, HTN, DM, IHD, AKI, TEE and Hypovolemia had a devastating impact on sodium balance. We found that hyponatremia was more prevalent than hypernatremia 23% vs. 12.1%, but hypernatremia has catastrophic effect on patient’s survival as compared with hyponatremia. There is reason for it, as we know that higher age impairs water metabolism, there is relative as well as absolute reduction in total body water, which makes elderly population distinctly inclined to developed dysnatremias [10]. Ageing, not only impairs the thirst mechanism [11], but it also reduces the concentrating capability of kidneys which increases the risk of dehydration and hypernatremia [12]. On the other hand, their ability to excrete water load is also hampered, this predisposition contributes to the commonly observed episode of hyponatremia in elderly hospitalized patients who received hypotonic fluid without proper monitoring [13].
We found significantly higher number of DM patients with both conditions in our population like other studies in which DM is a well-known cause of dysnatremias [14]. In an another study of 113 patients, Liamis et al found poorly controlled sugar level was the major factor in the development of hypernatremia in one third (34%) of their patients. The possible explanation of this observation is the glycosuria induced osmotic diuresis, which tends to raise the serum sodium levels. Steroids are the mainstay of COVID 19 therapy, which has dual effect on the generation of hypernatremia Steroids tend to raise the blood sugar level and makesit difficult to control, causes osmotic diuresis, concomitantly, they have mineralocorticoid activity which retain sodium and causes hypernatremia. Similarly, hyponatremia can also develop in DM patients by various mechanisms. Firstly, hyperglycemia causes water shift from intracellular to extracellular space, which causes trans locational hyponatremia. Secondly, excessive thirst causes increase water intake and in the background of covid pneumonia, an increase surge of antidiuretic hormone can cause hyponatremia [15].
In our study, hypertension was significantly associated with hypernatremia, although hyponatremia was also common but didn’t reach to a significant level. Ruiz and Cuesta in HOPECOVID- 19 registry analysis also found significant association of hypernatremia in hypertensive patients, the mechanism of this finding is not evident and it will need further evaluation [16]. The hyponatremia on the other hand is also reportedly associated with covid hypertensive patients. The underlying mechanism is supposed to be an increased proinflammatory cytokine release like interleukin (IL)-6 which induces Antidiuretic Hormone (ADH) production by direct non osmotic stimulation of ADH. Indirect stimulation of IL-6 is mediated by an injury to the alveolar basement membrane, resulting in activation of hypoxic pulmonary vasoconstriction pathway that leads to ADH release 61 [17].On the contrary, IHD was significantly associated with hyponatremia than hypernatremia. This association is also reported in HOPE – COVID-19 registry [16].
In our population, sodium metabolism was affected by the complications of COVID-19 infection like, AKI and TEE. We found that the patients who had AKI developed hypernatremia 5.5 times more as compared to those who did not have AKI. Sjostrom and Rysz examined the value of sodium as a prognostic marker for length of hospitalization, AKI and mortality in a cohort of 223 critically ill patients with COVID 19. They found patients who developed AKI developed severe hypernatremia along with high mortality [18]. Similarly, TEE is a well known complication of COVID 19 infection and we found this complication in those who have hypernatremia. The underlying pathophysiology of this macro and micro thrombi in small vessels is not clear and it needs further study [19]. Multiple small studies in which critically ill patients with COVID-19 were routinely screened for thrombotic disease demonstrated high rates of thrombotic complications in these patients ranging from 69% to 85% despite thrombo prophylaxis [20-22]. Similar to this we also observed hypernatremia lead to critical illnesses like need of vasopressor and ventilatory support and high mortality. In a case series of COVID patients with hypernatremia, Zimmer found similar observation of increased ventilatory support along with increased ICU stay [5]. On the other hand, we didn’t find any significant effect of hyponatremia on severity of disease. However in a registry analysis, Sanchez found hyponatremia as an independent risk factor for an increase in mortality as well as for an increase in the development of sepsis and requirement for intensive therapy. The reason of their finding might be due to relatively larger sample size of their study [16].
Conclusion
We found dysnatremias are a frequent feature of COVID-19 infection. The risk factors for this are, older age, comorbid conditions and development of complications. Among the dysnatremias, hypernatremia had distressing impact on severity of disease and outcome.
Declarations
Ethics approval and consent to participate was taken from IRDIRB (Reference #-IRD_IRB_2020_04_017).
Author contributions
1. FS: conception and design of the study along with acquisition of data.
2. AA: Reviewed the article.
3. SM: Reviewed the article.
4. JC: Acquisition of data and reviewed the article
5. SA: Acquisition of data and reviewed the article
6. ST: Acquisition of data and reviewed the article
7. BS: Analysis and interpretation of Data
8. SI: Drafting, conception, final review of the article along with interpretation and analysis of data.
Data availability statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgement
We acknowledged Dr Jahanzaib Khan (Senior Medical Officer- Dialysis) for helping us in collecting and arranging the Data and manuscript preparation.
REFERENCES
- Reynolds RM, Padfield PL, Seckl JR. Disorders of sodium balance. BMJ. 2006;332(7543):702-705.
- Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000;342(21):1581-1589.
- Aggarwal S, Garcia-Telles N, Aggarwal G, Lavie C, Lippi G, Henry BM. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): Early report from the United States. Diagnosis. 2020;7(2):91-96.
- Marr MJ. The future of behavior analysis: Foxes and hedgehogs revisited. The Behavior Analyst. 2017;40(1):197-207.
- Zimmer MA, Zink AK, Weißer CW, Vogt U, Michelsen A, Priebe HJ, Mols G. Hypernatremia-a manifestation of COVID-19: A case series. A&a Practice. 2020;14(9):e01295.
- Lindner G, Funk GC. Hypernatremia in critically ill patients. J Crit Care. 2013;28(2): 216e11.
- Worldometers. Coronavirus. Pakistan 2021.
- Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, et al. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. Jama. 2000 Aug 2;284(5):592-597.
- Nunez-Gil IJ, Estrada V, Fernández-Pérez C, Fernández-Rozas I, Martín-Sánchez FJ, Macaya C. The COVID-19 curve, health system overload, and mortality. Emergencias Rev la Soc Esp Med Emergencias. 2020;32(4):293-295.
- Ayus JC, Arieff AI. Abnormalities of water metabolism in the elderly. InSeminars in nephrology 1996; 16(4):277-288.
- Phillips PA, Rolls BJ, Ledingham JG, Forsling ML, Morton JJ, Crowe MJ, et al. Reduced thirst after water deprivation in healthy elderly men. N Engl J Med. 1984;311(12):753-759.
- Rowe JW, Shock NW, DeFronzo RA. The influence of age on the renal response to water deprivation in man. Nephron. 1976;17(4):270-278.
- Beck LH. Fluid and Electrolyte Balance in the Elderly. Nephrology and Geriatrics Integrated. 2000:51-55.
- Liamis G, Rodenburg EM, Hofman A, Zietse R, Stricker BH, Hoorn EJ. Electrolyte disorders in community subjects: prevalence and risk factors. Am J Med. 2013 Mar 1;126(3):256-63.
- Liamis G, Tsimihodimos V, Doumas M, Spyrou A, Bairaktari E, Elisaf M. Clinical and laboratory characteristics of hypernatraemia in an internal medicine clinic. Nephrology Dialysis Transplantation. 2008;23(1):136-143.
- Ruiz-Sánchez JG, Núñez-Gil IJ, Cuesta M, Rubio MA, Maroun-Eid C, Arroyo-Espliguero R, et al. Prognostic impact of hyponatremia and hypernatremia in COVID-19 pneumonia. A Hope-COVID-19 (Health Outcome Predictive Evaluation for COVID-19) registry analysis. Front Endocrinol. 2020;11.
- Lim JH, Jung HY, Choi JY, Park SH, Kim CD, Kim YL, et al. Hypertension and Electrolyte Disorders in Patients with COVID-19. Electrolytes & Blood Pressure. 2020;18(2):23.
- Sjöström A, Rysz S, Sjöström H, Höybye C. Hypernatremia is common in patients with severe COVID-19 and indicates a poor prognosis. 2020.
- Spyropoulos AC, Levy JH, Ageno W, Connors JM, Hunt BJ, Iba T, et al. Scientific and Standardization Committee communication: Clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Tromb Haemost. 2020;18(8):1859-1865.
- Llitjos JF, Leclerc M, Chochois C, Monsallier JM, Ramakers M, Auvray M, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020.
- Nahum J, Morichau-Beauchant T, Daviaud F, Echegut P, Fichet J, Maillet JM, et al. Venous thrombosis among critically ill patients with coronavirus disease 2019 (COVID-19). JAMA network open. 2020;3(5):e2010478.
- Ren B, Yan F, Deng Z, Zhang S, Xiao L, Wu M, et al. Extremely high incidence of lower extremity deep venous thrombosis in 48 patients with severe COVID-19 in Wuhan. Circulation. 2020;142(2):181-183.
Citation: Saeed F, Alam A, Memon S, Chughtai J, Ahmed S, Tariq S, et al. (2021) Dysnatremia in COVID-19 Disease Characteristics of Patients, Clinical Manifestation and Outcome in Pakistan. J Vaccines Vaccin. S12:001.
Copyright: © 2021 Saeed F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

