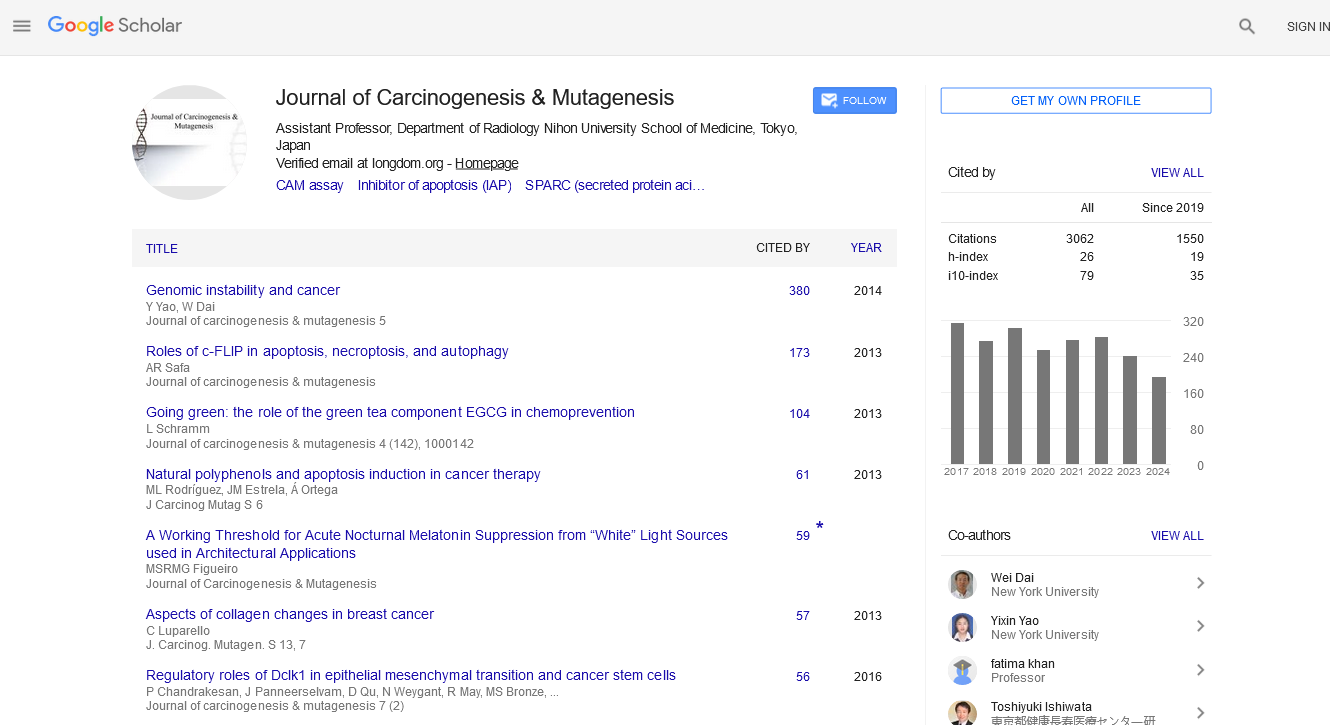
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2021) Volume 0, Issue 0
Does the Absence of Down-Regulation of MHC-I in Cancer Cells Necessarily Lead to their Annihilation by Immunologic Attack?
Pushpam Kumar Sinha*Received: 18-Jan-2021 Published: 11-Feb-2021, DOI: 10.35248/2157-2518.21.s6.001
Abstract
It has long been known now that MHC-I is down-regulated in several cancers and this has been linked with impaired immune attack against cancer cells. It is obvious then that low MHC-I expression is also linked with poor survival of cancer patients. But, however, through a careful analysis of the prognostic influence of MHC-I expression in colorectal cancer, head and neck squamous cell carcinoma, and biliary tract cancer, I conclude that the percentage of deaths of patients with high MHC-I expression in tumor (due to tumor alone) out of the total number of deaths (due to tumor alone) is not insignificant when compared to the percentage of deaths of cancer patients with low MHC-I expression in tumor. Hence the absence of down-regulation of MHC-I in cancer cells does not necessarily lead to their annihilation by immunologic attack. Stated differently, the down-regulation of MHC-I in cancer cells is not a necessary step in the genesis of cancer. New research needs to be directed at finding the immune evasion mechanism in cancer cells with high MHC-I expression. I finish the paper by speculating on few such mechanisms. Two of the important mechanisms speculated are clonal deletion of T cells (in the thymus) directed against antigens on Cancer Stem Cells, and down-regulation of MHC-II in metastatic cells which arise possibly by the fusion of hematopoietic stem cells and their lineages with tumor cells
Keywords
Immunity; Tumors; Antigenic peptides; Null hypothesis; Alternative hypothesis; Prognostic
Introduction
Is down-regulation of MHC-I in cancer cells a necessary step in the genesis of cancer ? The perspective in the question stated here is the same as that in the question stated in the title above. MHC-I is an immunologic glycoprotein, and hence, before we answer this question let us first see the role of MHC-I in the immunity of cells.
Though both innate immunity and adaptive immunity can kill tumors, in this paper I will be concerned only with adaptive immunity against tumors [1]. Adaptive immunity is a type of acquired immunity exercised by the lymphocytes- T cells and B cells. So based on whether the immunologic attack is by T cells or B cells, adaptive immunity is called Cell Mediated Immunity (CMI) or Humoral Immunity (HI) respectively. Major Histocompatibilty Complex (MHC) molecule of class I play a role in CMI. Hence, further, in this paper I am concerned with CMI and not HI. Though HI has been observed against some cancers, their outcome has remained elusive to scientists, more so, because HI also targets those antigens that are present not only in cancer cells but also in healthy cells [2]. From next section, the perspective, that CMI plays obvious role against tumors, is evident.
T cells have T Cell Receptor (TCR) on their surface which recognize and attach to broken antigenic peptides bound to MHC, to start the cascade of activation processes of T cells. The cells which present the antigenic peptides bound to MHC are popularly known as Antigen Presenting Cells (APC). There are two subsets of T cells: the CD4+ T Cell known as helper T cell (Th), and the CD8+ T Cell known as cytotoxic T cell (Tc). The killing of target cells is performed by Tc and not by Th, but without the activation of Th, Tc cannot perform its destructive function. Tc is activated by MHC-I antigenic peptide complex, where as Th is activated by MHC-II antigenic peptide complex. MHC-I is expressed in all the cells of the body, where as MHC-II is present in macrophages, dendritic cells, B cells. Priming of TCR in both subsets of the T cells is followed by costimulatory signals for complete activation. On complete activation Th produces IL-2, and also IL-2 receptor, on itself and Tc whose TCR has been primed. Complete activation of Th also increases the CD80/86 expression by the APC which has primed Tc. The CD80/86 interaction with CD28 on Tc leads to its differentiation to mature and effector Tc that thereby acquires cytotoxicity, and hence kills the target cell (APC here).
MHC-I and Cancer
MHC-I has been known to be down-regulated in Cancer Stem Cells (CSCs) of Glioblastoma Multiforme Cancer (GBM), Melanoma and Colorectal Cancer (CRC) [3]. Many cancers now is known to have stem cell basis, specially cancers of those organs that have Adult Stem Cells (ASCs) at their base [4]. When ASCs and or multi-potent progenitors and or, in some cases, terminally differentiated cells of a particular organ accumulate multiple genetic mutations in multiple stages in a sequence spread over many years, they are transformed to CSCs [4,5]. CSCs, like their counterpart ASCs are rare, quiet and have self-renewing capability [3].
Even otherwise, the MHC-I expression is known to be downregulated in tumors of several cancers, and not merely in CSCs alone: CRC [6], Head and Neck Squamous Cell Carcinoma (HNSCC), Biliary Tract Cancer (BTC), melanoma, pancreatic cancer, breast cancer, GBM, lung cancer, etc.. [7-14]. I have the data available on effect of MHC-I expression on overall survival of patients in tumors of CRC, HNSCC, and BTC. In a sample size of 455 CRC patients, 311 tumors showed high level of MHC-I expression, 32 tumors showed low level of MHC-I expression, and 112 had no MHC-I expression [6]. I will now discuss and or analyze the results of Kaplan-Meiercurves of overall survival or disease specific survival in all the three [6-8]. But, however, I will consider only those Kaplan-Meier curves for which p<0.05. For such low values of p one is sure that alternative hypothesis is true, and null hypothesis is invalid.
According to the figures, the curve labelled high reaches last horizontal line at 92.7 months of survival from operation date and the value of cumulative survival for that interval is 0.5, which means nearly 155 deaths in absolute number of patients with tumors having high MHC-I expression [6]. The curve labelled low reaches last horizontal line at 47.3 months of survival from operation date and the value of cumulative survival for that interval is 0.26, which means nearly 23 deaths in absolute number of patients with tumors having low MHC-I expression. The curve labelled absent reaches last horizontal line at 67.3 months of survival from operation date and the value of cumulative survival for that interval is 0.42, which means nearly 65 deaths in absolute number of patients with tumors having no MHC-I expression. Hence, the percentage of deaths of CRC patients (due to CRC alone) with high level of MHC class I expression in tumor cells out of the total number of deaths of CRC patients (due to CRC alone) is 63.8.
In a sample size of 158 HNSCC patients, 103 were PD-L1 positive; and amongst this 103, 63 had strong MHC-I expression, 29 had weak and 11 showed no MHC-I expression[7]. In the background of PD-L1 negative tumor cells, the MHCI expression had no prognostic significance (p=0.426) as in the figures [7]. In the background of PD-L1 positive tumor cells as in the figures, by an analysis similar to what was done with similar to the figure, the percentage of deaths of HNSCC patients (due to HNSCC alone) with strong MHC class I expression in tumor cells out of the total number of deaths of HNSCC patients (due to HNSCC alone) is 37.5.PD-L1 (Programmed Death- Ligand 1), when, binds to the trans-membrane protein PD-1 (Programmed Death-1) on the surface of T cells, it inhibits the proliferation of cytotoxic effector T cells. Thereby PD-L1/PD-1 interaction has anti-inflammatory effect on T cells [6,7].
In a sample size of 302 BTC patients, 157 had MHC-I antigen expression score 0-6 IRS, while 145 had MHC-I antigen expression score 8-12 IRS by an analysis similar to what was done in figures [6]. The percentage of deaths of BTC patients (due to BTC alone) with MHC class I expression score 8-12. According to the figures, IRS in tumor cells out of the total number of deaths of BTC patients (due to BTC alone) is 42. IRS stands for immunoreactive score, it is calculated by the multiplication of the staining intensity score of the antibody directed against MHC-I and the percentage score of the percentage of cells stained with the antibody directed against MHC-I [8,15-18]. The staining intensity score and the percentage score are calculated according to the scheme given in Table 1.
| Staining intensity score | Percentage score | ||
|---|---|---|---|
| Quality of staining | Score | Percentage of cells stained | Score |
| None | 0 | <10% | 1 |
| Weak | 1 | 10-50% | 2 |
| Moderate | 2 | 51-80% | 3 |
| Strong | 3 | >80% | 4 |
Table 1: The two components of the Immunoreactive Score (IRS).
Table 2 summarizes the result of analysis done in previous section. The percentage of deaths of CRC patients with high MHC-I expression in tumor cells is exceptionally high. The absolute number of the deaths of CRC patients with high MHC-I expression in tumor cells is also very high. The percentage of deaths of HNSCC patients with strong MHC-I expression in tumor cells is nearly comparable to that with weak MHC-I expression in tumor cells.
| Percentage of deaths of CRC patients | Percentage of deaths of HNSCC patients | Percentage of deaths of BTC patients | |||
|---|---|---|---|---|---|
| High MHC-I expression | Low MHC-I expression | Strong MHC-I expression | Weak MHC-I expression | 8-12 IRS MHC-I expression | 0-6 IRS MHC-I expression |
| 63.8 | 9.5 | 37.5 | 40.6 | 42 | 58 |
Table 2: Result of analysis done in previous section.
Discussion and Conclusion
It seems that tumor cells highly expressing MHC-I have also found ways to evade immune attack. Ever since the discovery that MHC-I is normally down-regulated in cancer cells of many cancers, most of the research has focused on unearthing mechanisms of down-regulation of MHC-I in cancer cells. By this article it is clear that there is a need to do research to find out also the immune evading mechanisms by tumor cells highly expressing MHC-I. A few of the possible mechanisms could be
1. Direct down-regulation of CD80/86, most likely, by epigenetic mutation. In fact CD80/86 has been found to be absent in CSCs.
2. Indirect down-regulation of CD80/86 by IL-10. IL-10 is known to cause down-regulation of CD80/86 in the APC which has primed Tc with tumor antigens. High levels of IL-10 have been found in the serum of patients suffering from certain cancers, and reduced survival of patients have been observed in these cases. It will be interesting to measure the levels of expression of IL-10 in the microenvironment of tumor cells highly expressing MHC-I.
3. Clonal deletion of T cells in the thymus. The normal healthy cells of the human body also induce immune response by T cells through binding of the TCR to MHC-self antigen peptide complex. However, such activated T cells against self-antigens are negatively selected, and annihilation of these T cells take place in the thymus. Now, CSCs share several of the properties of their counterpart non-mutated ASCs. So, like their counterpart ASCs it is expected that CSCs too evade immune attack by clonal deletion of T cells in the thymus
4. Down-regulation of MHC-II. One of the hypotheses of the cellular origin of metastasis is that the inflamed tumor microenvironment causes the transformation of hematopoietic stem cells and or their lineages (HSCs/l) into metastatic cells, alternatively the fusion of HSCs/l with tumor cells give rise to metastatic cells. It is possible that MHC-II in these metastatic cells is down-regulated, thereby evading immune attack.
5. Removal of the tumor antigens from cell surface by modulation so that they are not available for priming Tc and initiate immune attack.
REFERENCES
- Mohanty SK, SaiLeela K. Textbook of Immunology(2ne edn), Jaypee Brothers Medical Publishers Ltd, Daryaganj, New Delhi, 2014.
- Yuen GJ, Demissie E, Pillai S. B lymphocytes and cancer: a love-hate relationship. Trends Cancer 2016;2(12): 747-757.
- Maccalli C, Volonte` A, Cimminiello C, Parmiani G. Immunology of cancer stem cells in solid tumours: A review. Euro JCancer 2014;50(3): 649-655.
- Sinha PK. The common genesis of all cancers. JCarcinog Mutagen 2019;10(3):342.
- Corces-Zimmerman MR, Majeti R. Pre-leukemic evolution of hematopoietic stem cells: the importance of early mutations in leukemogenesis. Leukemia 2014;28(7): 2276-2282.
- Watson NFS, Ramage JM, Madjd Z, Spendlove I, Ellis IO, Scholefield JH, et al. Immunosurveillance is active in colorectal cancer as downregulation but not complete loss of MHC class I expression correlates with a poor prognosis. Int J Cancer 2006;118(1) :6-10.
- Yoo SH, Keam B, Ock CY, Kim S, Han B, Kim JW, et al. Prognostic value of the association between MHC class I downregulation and PD-L1upregulation in head and neck squamous cell carcinoma patients. Scientific Rep 2019; 9(5):7680.
- Goeppert B, Frauenschuh L, Zucknick M, Roessler S, Mehrabi A, Hafezi M, et al. Major histocompatibility complex class I expression impacts on patient survival and type and density of immune cells in biliary tract cancer. British J Cancer 2015;113(3):1343-1349 (2015).
- Lee JH, Shklovskaya E, Lim SY, Carlino MS, Menzies AM, Stewart A, et al. Transcriptional downregulation of MHC class I and melanoma de- differentiation in resistance to PD-1inhibition. Nature Comm 2020;11(4):1897
- Byrne EH, Fisher DE. Immune and molecular correlates in melanoma treated with immune checkpoint blockade. Cancer 2017;123(11):2143-2153.
- Huang X, Zhang X, Bail X, Liang T. Eating self for not be eaten: pancreatic cancer suppresses self-immunogenicity by autophagy-mediated MHC-I degradation. Signal Transd Targ Ther 2020;5(6):94.
- Inoue M, Mimura K, Izawa S, Shiraishi K, Inoue A, Shiba S, et al. Expression of MHC Class I on breast cancer cells correlates inversely with HER2 expression. Onco Immun 2012;1(7):1104-1110.
- Zagzag D, Salnikow K, Chiriboga L, Yee H, Lan L, Ali MA, et al. Newcomb, downregulation of major histocompatibility complex antigens in invading glioma cells: stealth invasion of the brain. Lab Invest 2005;85(3):328-341.
- Morrison BJ, Steel JC, Morris JC. Reduction of MHC-I expression limits T-lymphocyte-mediated killing of Cancer-initiating cells. BMC Cancer 2018;18(4):469.
- Cornel AM, Mimpen IL, Nierkens S. MHC class I downregulation in cancer: underlying mechanisms and potential targets for cancer immunotherapy. Cancers 2020;12(7):1760.
- Sheikhpour E, Noorbakhsh P, Foroughi E, Farahnak S, Nasiri R, Neamatzadeh H. A survey on the role of interleukin-10 in breast cancer: a narrative. Repo Biochem Mole Biol 2018;7(1):30-37.
- Gonzalez Garza MT, Cruz Vega DE, Bernal CM. IL10 as Cancer Biomarker. Translational Res Cancer 2019;10(2)25.
- Seyfried TN, Huysentruy LC. On the origin of cancer metastasis. Crit Rev Oncog 2013;18(2):43-73.
Citation: Sinha PK (2021) Does the Absence of Down-Regulation of MHC-I in Cancer Cells Necessarily Lead to their Annihilation by Immunologic Attack? J Carcinog Mutagen S16: 001.
Copyright: © 2021 Sinha PK. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.