Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 6, Issue 6
Disseminated Cutaneous Leishmaniasis: A Case Report
Edna Indira Rodriguez Garcia* and Román Mercado EstefaníaReceived: 09-Nov-2021 Published: 30-Nov-2021, DOI: 10.35248/2684-1436.21.6.140
Abstract
Leishmaniasis is a parasitic disease caused by intracellular protozoan Leishmania genus, considered an occupational disease, which mainly affects farmers, and is associated with conditions of poverty. With a wide spectrum of clinical manifestations that can make early diagnosis and timely treatment difficult, the case presented is an immunocompetent patient who developed disseminated cutaneous leishmanisis.
Keywords
Cutaneous leishmaniasis; Disseminated cutaneous; Immune-competent
Introduction
Cutaneous leishmaniasis is a chronic skin disease caused by intracellular protozoa, of Leishmania genus that transmit infection to mammals by insect vectors of the Phlebotomus and Lutzomia families. Leishmaniasis is characterized by a spectrum of clinical manifestations: Localized Cutaneous (LCL), Disseminated Cutaneous (LCD), Mucocutaneous Leishmaniasis (CML), and Visceral Leishmaniasis (VL). We present the case of an immune-competent patient with disseminated cutaneous leishmaniasis with an adequate response to systemic treatment.
Clinical Case
A 68-year-old male patient from tabasco and a veracruz resident with a history of type 2 diabetes with adequate adherence to treatment. His condition began 1 year prior to diagnosis with the appearance of an asymptomatic red papule of approximately 1 cm on the left arm, with progressive increase in size and formation of a vesiculopustular lesion, 4 months later, central depression of the lesion appeared, borders erythematous, and purulent material leakage, one month later the lesions spread to the left arm, neck, thorax and face with the same characteristics (Figures 1 and 2)

Figure 1:Initial lesion with raised, erythematous borders with central depression.
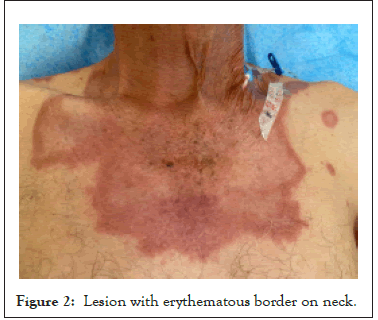
Figure 2: Lesion with erythematous border on neck.
Diagnosis
He went to his medical unit where he was treated with unspecified topical medication without achieving improvement in the lesion, with progressive extension to the lower extremities and abdomen. At 6 months the lesions were found disseminated, the patient attended a dermatological evaluation where a biopsy of the lesions was taken, which reported a chronic and granulomatous inflammatory process with giant Langhans-type cells in its cytoplasm with the presence of Leishmania bodies (Figure 3).
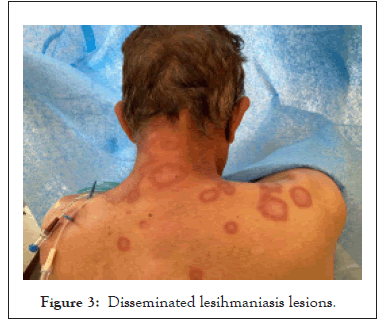
Figure 3: Disseminated lesihmaniasis lesions.
Treatment
Start of antimionate meglumine was indicated, it was not administered due to the lack of availability of the drug. He attended an evaluation at the General Hospital of the Zone, where the initiation of liposomal amphotericin B was indicated at a dose of 3 mg/kg of weight. At 20 days, in all the lesions the raised edges and the erythema diminished. Of the adverse effects of amphotericin administration, the patient had moderate hypokalemia, which was treated with intravenous potassium replacements.
Results and Discussion
Leishmaniasis is a chronic disease of the skin, mucosa or viscera caused by different species of the genus Leishmania. The WHO classifies leishmaniasis as an emerging and uncontrolled disease since it is endemic to 98 countries on five continents and around 1.2 million new cases are reported each year [1,2].
In Mexico, the disease has been known since the pre-Hispanic era, it has been categorized as an occupational disease, affecting biologists, ornithologists, hunters, peasants, and the military. The prevalence and development of leishmaniasis are largely dependent on environmental factors and natural conditions, climatic changes and deforestation have been associated with an increase in leishmaniasis case reports, living conditions, poverty, marginalization and Immunosuppression states are some other risk factors associated with the disease [3,4].
It is a disease caused by several species of obligate intra-macrophage protozoan parasites of the genus Leishmania, transmitted to humans by females of the genera Phlebotomus and Lutzomyia, as well as several other species of mammals, including rodents, bats, baboons, leopards, and hyenas. Transmitting mosquitoes inhabit low and humid plains, proliferate in rainy seasons and have nocturnal activity; the female bites the parasites in the form of amastigotes from the reservoir blood, which transform into procyclic premastigotes and then promastigotes. metacyclic, the infectious form [1,4].
The state of health, the species and the transmission vector are decisive in the clinical presentation of the infection, once within the body immunity mechanisms are activated, the transmitted promastigotes are processed by dendritic cells, presented to T cells naive that will produce a cascade of cytokines and a change from Th1 to Th2 with increases in the production of interleukin-4 (IL-4), IL-6, and through the inhibition of tumor necrosis factor alpha (TNFα), interferon gamma (IFNγ), IL-12 and nitric oxide production. The immune response can vary according to each clinical form [5,6].
The cutaneous form originates from L. tropica, it has an incubation period ranging from 1 to 4 weeks, but it can take years. At the site of the sting, a papular lesion appears, generally asymptomatic, which days later becomes a pustular vesicle lesion, then a nodular lesion that ulcerates, with raised purplish edges, a typical case presented by the patient. The mucocutaneous form originates from L. braziliensis and L. mexicana, affects young people in the form of a nodule that ulcerates in an exposed area. Diffuse cutaneous leishmaniasis affects all of the skin, predominates in exposed areas, ears, and extremities. Lastly, in the visceral form due to L. donovani there is weight loss, fever, adenomegaly, and hepatosplenomegaly [1].
The diagnosis is clinical and is based on a consistent epidemiological context, confirming the diagnosis with the identification of parasite. It can be seen in smears or imprints stained with Giemsa or Wright. Inoculation is also used for culture, which must be obtained from the active edge of the lesion. The Montenegro skin test is another useful diagnostic tool, positive in localized forms and negative in anergic forms, not forgetting to mention that a positive test supports the diagnosis, but a negative one does not exclude it [1,6].
Currently, treatments for leishmaniasis include antimonials for cutaneous forms and amphotericin B for visceral disease, and even drugs such as ketoconazole have been used as alternative therapy, however, these therapies have significant disadvantages, including cytotoxicity and drug resistance. Given the high resistance in some endemic areas, new therapies have been developed, including the use of immunotherapy and azole antifungal molecules, with marked antileishmania activity. It should be noted that the treatment of LCD is associated with a worse prognosis due to the high probability of recurrences [1,6-8].
Conclusion
Leishmaniasis represents a diagnostic and therapeutic challenge, increasingly arising due to factors such as climate change. Disseminated cutaneous leishmaniasis is a rare manifestation, which we must not forget since the prognosis depends on the early start of treatment, in the patient the diagnosis was delayed for almost a year, however presents a good response to the administered treatment.
REFERENCES
- Murphy-Chutorian B, Han G, Cohen SR. Dermatologic manifestations of diabetes mellitus: A review. Endocrinol Metab Clin. 2013;42(4):869-98.
- Kurdi AT. Bullosis diabeticorum. The Lancet. 2013;382(9907):e31.
- Dinulos JG. Habif'Clinical Dermatology E-Book. Elsev Heal Sci. 2019.
- Jean B, Joseph LJ, Julie VS. Other Vesiculo bullous diseases. Dermatol. 2021.
- Downing C, Tamirisa A, Khan F, Tyring S, Lapolla W. Bullosis diabeticorum: A rare bullous eruption in diabetes mellitus. J Am Acad Dermatol. 2014;70(5):115.
- Parikh S, Murphy M, Chen A. A case of bullosis diabeticorum restricted to the fingers: 6756. J Am Acad Dermatol. 2018;79(3).
- Frioui M, Aouiche S, Ouerdane K, Boudiba A. P2131 Ŧ Bullose diabétique: A propos d’un cas ŧ. Diabetes Metab. 2013;39:A99.
Citation: Garcia EIR, Estefanía RM (2021) Disseminated Cutaneous Leishmaniasis: A Case Report. J Dermatitis. 6:140.
Copyright: © 2021 Garcia EIR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

