Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2024) Volume 9, Issue 2
Differentiation between Tuberculosis Peritonitis and Cancerous Peritonitis Caused by Advanced Ovarian Cancer: A Short Communication
Hiroaki Ishida*, Megumi Manrai, Mizuki Nonaka and Akiko TakashimaanielleReceived: 25-Mar-2024, Manuscript No. JIDD-24-25265; Editor assigned: 27-Apr-2024, Pre QC No. JIDD-24-25265 (PQ); Reviewed: 10-Apr-2024, QC No. JIDD-24-25265; Revised: 17-Apr-2024, Manuscript No. JIDD-24-25265 (R); Published: 24-Apr-2024, DOI: 10.35248/2576-389X.24.09.259
Abstract
Laparoscopy for intra-abdominal? Exploration and tissue? Sampling is useful in advanced ovarian cancers, in which it is presumed to be difficult to achieve complete? Tumour reduction in the initial surgery. We reported on a case in which we suspected advanced ovarian cancer, performed diagnostic laparoscopy, and experienced tuberculosis peritonitis after the postoperative diagnosis. Tuberculosis peritonitis has many similarities with cancerous peritonitis caused by advanced ovarian cancer in terms of clinical symptoms and clinical test data, so how can we differentiate between tuberculosis peritonitis and cancerous peritonitis before surgery? This brief examination examines whether it is feasible to distinguish between tuberculosis peritonitis and malignant peritonitis before surgery.
Keywords
Tuberculosis peritonitis; Ovarian cancer; Biopsy
About the Study
In recent years, for ovarian cancer that is predicted to be difficult to remove based on preoperative diagnosis, laparoscopy is performed to observe the inside of the abdominal cavity, confirm the spread of the lesion, and perform using tissue biopsy for histopathological examination and genetic testing [1]. Although the infection rate of tuberculosis peritonitis is thought to be low, medical personnel who perform surgery without suspecting tuberculosis are exposed to the risk of infection [2]. It is necessary to remember and take infection control measures. Tuberculosis peritonitis has many similarities with cancerous peritonitis caused by advanced ovarian cancer in terms of clinical symptoms and clinical test data, so how can we differentiate between tuberculosis peritonitis and cancerous peritonitis before surgery? This study is based on the literature review.
Clinical characteristics of tuberculosis peritonitis and similarities between tuberculosis peritonitis and cancerous peritonitis
The clinical symptoms of tuberculosis peritonitis are similar to advanced ovarian cancer, such as abdominal distention, abdominal pain, and shortness of breath, weight loss, the presence of ascites, and a pelvic mass [3]. Some studies have shown that the younger age at onset (median age 20-40 years) of patients with peritoneal tuberculosis may be a distinguishing feature from malignant tumors (median age 50-70 years) [3]. Tuberculosis peritonitis is characterized by ascites, peritoneal thickening, and increased omental adipose tissue density on CT images [1]. Serum CA125 is a tumor marker for ovarian cancer, but it also increases in tuberculosis peritonitis [4]. In addition, it is known that Fluorodeoxyglucose (FDG) uptake increases in tuberculosis peritonitis when the inflammatory response due to tuberculosis is high [5]. The positive rate of mycobacterial culture in ascetic fluid is 20% to 50% [6], and the positive rate of PCR testing is approximately 60% to 80% [7]. Therefore, these are not highly sensitive tests. For these reasons, tuberculosis peritonitis is often misdiagnosed as cancerous peritonitis due to advanced ovarian cancer and is diagnosed postoperatively.
How can we differentiate between tuberculosis peritonitis and cancerous peritonitis due to ovarian cancer before surgery?
Although histopathological diagnosis using laparoscopic surgery is a useful definitive diagnosis of tuberculosis peritonitis, Figure 1, shows how to suspect tuberculosis peritonitis before surgery. In tuberculosis peritonitis, cytopathological examination of ascites is negative for malignant cells [3]. In tuberculosis peritonitis, Adenosine Deaminase (ADA) in ascites is 40 U/L in over 95% of cases, making it one of the most sensitive tests [3]. The T-SPOT TB test (T-SPOT) is a test for diagnosing tuberculosis infection, which stimulates peripheral blood with mycobacteria and measures the levels of tuberculosis-specific antigens and Interferon-γ (IFN-γ) produced [1]. The T-SPOT is not a test that can definitively diagnose current infection, as it will give a positive result if you are currently infected or have had a history of infection. However, if it is positive, tuberculosis peritonitis should be considered [1].
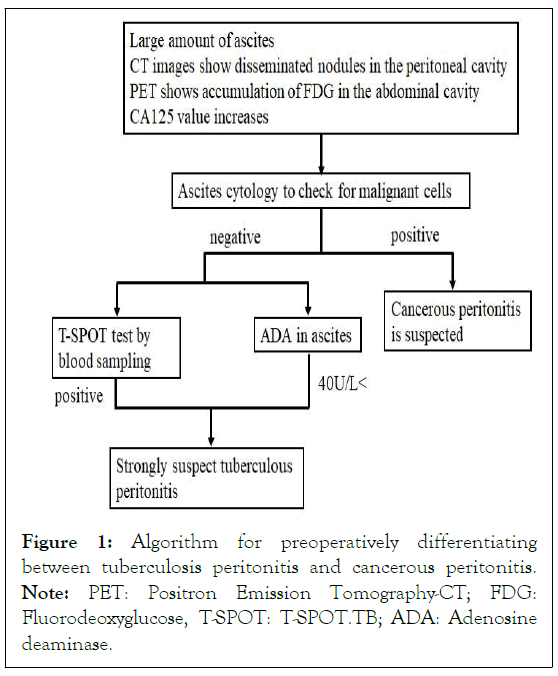
Figure 1: Algorithm for preoperatively differentiating
between tuberculosis peritonitis and cancerous peritonitis.
Note: PET: Positron Emission Tomography-CT; FDG: Fluorodeoxyglucose, T-SPOT: T-SPOT.TB; ADA: Adenosine deaminase.
Intraperitoneal findings of tuberculosis peritonitis
Tuberculosis peritonitis has characteristic macroscopic findings, shown in Figure 2 [1]. Massive ascites is similar to cancerous peritonitis, but small nodules are scattered throughout the uterus, bilateral appendages, and peritoneum and the nodules are smaller than in cancerous peritonitis [1]. Fibrous adhesions between the peritoneum and the small intestine are also characteristic of tuberculosis peritonitis [1]. Laparotomy or laparoscopic biopsy has been reported to have a sensitivity of 95% for the diagnosis of tuberculosis peritonitis [8,9]. Therefore, after taking adequate infection control measures, laparoscopic histopathological diagnosis of tissues showing tuberculosis peritonitis is an accurate, minimally invasive and useful method.

Figure 2: Characteristic Laparoscopic findings of Tuberculosis peritonitis; a) Massive ascites; b) Small nodules diffusely disseminated over the uterus, bilateral adnexa, and peritoneum; c) Fibrous adhesions between the peritoneum and the small intestine; d) Numerous disseminated nodules were observed on the surface of the right fallopian tube.
Conclusion
Tuberculosis peritonitis is a disease that has a negative prognosis if the start of treatment is delayed. In addition, laparoscopic surgery may involve the risk of aerosol infection, so it is necessary to take infection control measures in advance, taking into account the possibility of tuberculosis. In our case, tuberculosis could not be suspected before surgery. However, as a result of this study, it may possible to predict tuberculosis peritonitis in advance in the early stage by performing a preoperative ascetic fluid cytology test, measuring ADA in ascetic fluid, and examining T-SPOT in a blood test.
References
- Nonaka M, Ishida H, Manrai M, Takashima A. Tuberculosis peritonitis diagnosed following laparoscopic examination for suspected advanced ovarian cancer. BMJ Case Rep. 2024;17(3):257973.
[Crossref] [Google Scholar] [PubMed]
- Jensen PA, Lambert LA, Iademarco MF, Ridzon RC, Centers for Disease Control and Prevention. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep. 2005;54(17):1-141.
[Crossref] [Google Scholar] [PubMed]
- Maheshwari A, Gupta S, Rai S, Rekhi B, Kelkar R, Shylasree TS, et al. Clinical and laboratory characteristics of patients with peritoneal tuberculosis mimicking advanced ovarian cancer. South Asian J Cancer. 2021;10(2):102-106.
[Crossref] [Google Scholar] [PubMed]
- Liu Q, Zhang Q, Guan Q, Xu JF, Shi QL. Abdominopelvic tuberculosis mimicking advanced ovarian cancer and pelvic inflammatory disease: A series of 28 female cases. Arch Gynecol Obstet. 2014;289(3):623-629.
[Crossref] [Google Scholar] [PubMed]
- Hara T, Kosaka N, Suzuki T, Kudo K, Niino H. Uptake rates of 18F-fluorodeoxyglucose and 11C-choline in lung cancer and pulmonary tuberculosis: A positron emission tomography study. Chest. 2003;124(3):893-901.
[Crossref] [Google Scholar] [PubMed]
- Marshall JB. Tuberculosis of the gastrointestinal tract and peritoneum. Am J Gastroenterol. 1993;88(7):989-999.
[Crossref] [Google Scholar] [PubMed]
- Sherman S, Rohwedder JJ, Ravikrishnan KP, Weg JG. Tuberculosis enteritis and peritonitis: Report of 36 general hospital cases. Arch Intern Med. 1980;140(4):506-508.
[Crossref] [Google Scholar] [PubMed]
- Bhargava DK, Chopra P, Nijhawan S, Dasarathy S, Kushwaha AK. Peritoneal tuberculosis: Laparoscopic patterns and its diagnostic accuracy. Am J Gastroenterol. 1992;87(1):109-112.
[Crossref] [Google Scholar] [PubMed]
- Chow KM, Chow VC, Hung LC, Wong SM, Szeto CC. Tuberculosis peritonitis-associated mortality is high among patients waiting for the results of mycobacterial cultures of ascetic fluid samples. Clin Infect Dis. 2002;35(4):409-413.
[Crossref] [Google Scholar] [PubMed]
Citation: Ishida H, Manrai M, Nonaka M, Takashimaanielle A (2024) Differentiation between Tuberculosis Peritonitis and Cancerous Peritonitis Caused by Advanced Ovarian Cancer: A Short Communication. J Infect Dis Diagn. 9:259.
Copyright: © 2024 Ishida H, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

